CONCEPTS IN BIOLOGY
PART VI. PHYSIOLOGICAL PROCESSES
24. Materials Exchange in the Body
24.4. Gas Exchange: The Respiratory System
The respiratory system is the organ system that moves air into and out of the body; it consists of the lungs, trachea, airtransport pathway, and diaphragm. The lungs are organs of the body that allow gas exchange to take place between the air and blood. Associated with the lungs is a set of tubes, part of the air-transport pathway, that conducts air from outside the body to the lungs. The single, large-diameter trachea is supported by rings of cartilage that prevent its collapse. It branches into two major bronchi (singular, bronchus), which deliver air to smaller and smaller branches. Bronchi are also supported by cartilage. The smallest tubes, bronchioles, contain smooth muscle and are therefore capable of constricting. Finally, the bronchioles deliver air to clusters of tiny sacs, known as alveoli (singular, alveolus), where the exchange of gases between the air and the blood takes place.
The nose, mouth, and throat are also important parts of the air-transport pathway because they modify the humidity and temperature of the air and clean the air as it passes. The lining of the trachea contains cells with cilia, which beat in one direction to move mucus and foreign materials from the lungs. The foreign matter can then be expelled by swallowing or coughing. Figure 24.6 illustrates the various parts of the respiratory system.
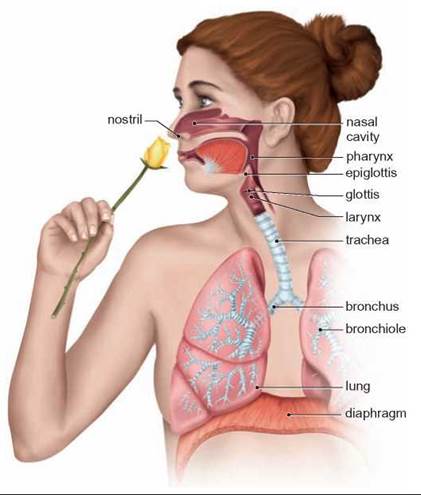
FIGURE 24.6. Respiratory Anatomy
Although gas exchange takes place in the alveoli of the lungs, there are many other important parts of the respiratory system. The nasal cavity cleans, warms, and humidifies the air entering the lungs. The trachea is also important in cleaning the air going to the lungs.
Mechanics of Breathing
Breathing is the process of moving air in and out of the lungs. It is accomplished by the movement of several muscles. The diaphragm is a muscular organ that separates the chest cavity, which contains the lungs, from the abdominal cavity. In addition, intercostal muscles located between the ribs are involved in breathing. During inhalation, the diaphragm contracts, causing it to move downward and the external intercostal muscles of the chest wall contract, causing the chest wall to move outward and upward. Both of these actions cause the volume of the chest cavity to increase. This results in a lower pressure in the chest cavity compared with the outside air pressure. Thus, air flows from the outside high-pressure area through the trachea, bronchi, and bronchioles to the alveoli. During normal, relaxed breathing, exhalation is accomplished by the chest wall and diaphragm simply relaxing and returning to their normal positions. Muscular contraction is not involved (figure 24.7).
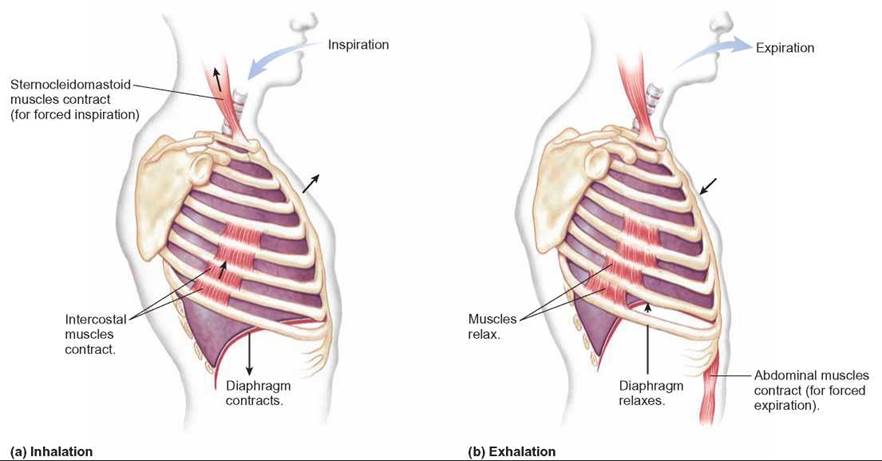
FIGURE 24.7. Breathing Movements
During (a) inhalation, the diaphragm and external intercostal muscles between the ribs contract, causing the volume of the chest cavity to increase. During a normal (b) exhalation, these muscles relax, and the chest volume returns to normal.
When the body’s demand for oxygen increases during exercise, the breathing system responds by exchanging the gases in the lungs more rapidly. This can be accomplished both by increasing the breathing rate and by increasing the volume of air exchanged with each breath. An increase in volume exchanged per breath is accomplished in two ways. First, the muscles of inhalation can contract more forcefully, resulting in a greater change in the volume of the chest cavity. Second, the lungs can be emptied more completely by contracting the muscles of the abdomen, which forces the abdominal contents upward against the diaphragm and compresses the lungs. A set of internal intercostal muscles also helps compress the chest.
Breathing System Regulation
Several mechanisms can cause changes in the rate and depth of breathing, but the primary mechanism is tied to the amount of carbon dioxide present in the blood. Carbon dioxide, a waste product of aerobic cellular respiration, becomes toxic in high quantities because it combines with water to form carbonic acid:
![]()
As mentioned previously, if carbon dioxide cannot be eliminated, the pH of the blood is lowered. Eventually, this can cause death.
Exercising causes an increase in the amount of carbon dioxide in the blood, because the muscles are oxidizing glucose more rapidly. This lowers the blood’s pH. Certain brain cells and specialized cells in the aortic arch and carotid arteries are sensitive to changes in blood pH. When these cells sense a lower blood pH, they cause the brain to send nerve impulses more frequently to the diaphragm and intercostal muscles. These muscles contract more rapidly and more forcefully, resulting in more rapid, deeper breathing. Because more air is being exchanged per minute, carbon dioxide is lost from the lungs more rapidly. When exercise stops, blood pH rises, and breathing eventually returns to normal (figure 24.8).
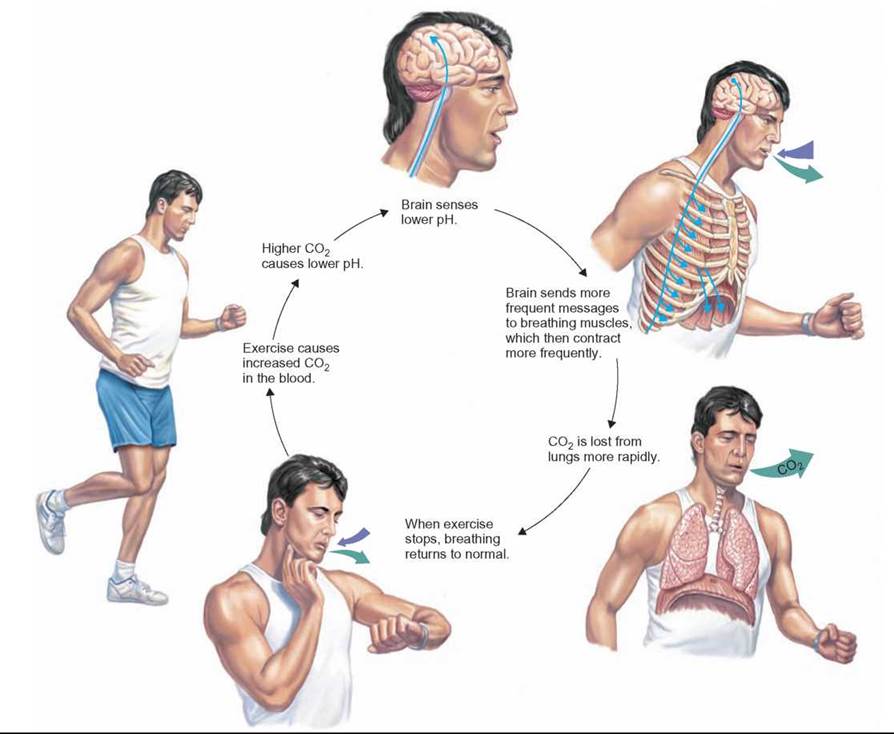
FIGURE 24.8. Control of Breathing Rate
The rate of breathing is controlled by cells in the brain, aorta, and carotid arteries that sense the pH of the blood. When the amount of CO2 increases, the pH drops (the blood becomes more acidic) and the brain sends more frequent messages to the diaphragm and intercostal muscles, causing the breathing rate to increase. More rapid breathing increases the rate at which CO2 is lost from the blood; thus, the blood pH rises (it becomes less acidic) and the breathing rate decreases.
Lung Function
The lungs allow blood and air to come into close contact with each other. Air flows in and out of the lungs during breathing. The blood flows through capillaries in the lungs and is in close contact with the air in the alveoli of the lungs. For oxygen to enter or carbon dioxide to exit the body, the molecules must pass through a surface. The efficiency of exchange is limited by the surface area available. This problem is solved in the lungs by the large number of tiny sacs, the alveoli. Each alveolus is about 0.25 to 0.5 millimeters across. However, alveoli are so numerous that the total surface area of all these sacs is about 70 square meters—comparable to the floor space of many standard-sized classrooms. The walls of both the capillaries and the alveoli are very thin, and the close association of alveoli and capillaries in the lungs allows the easy diffusion of oxygen and carbon dioxide across these membranes (figure 24.9).
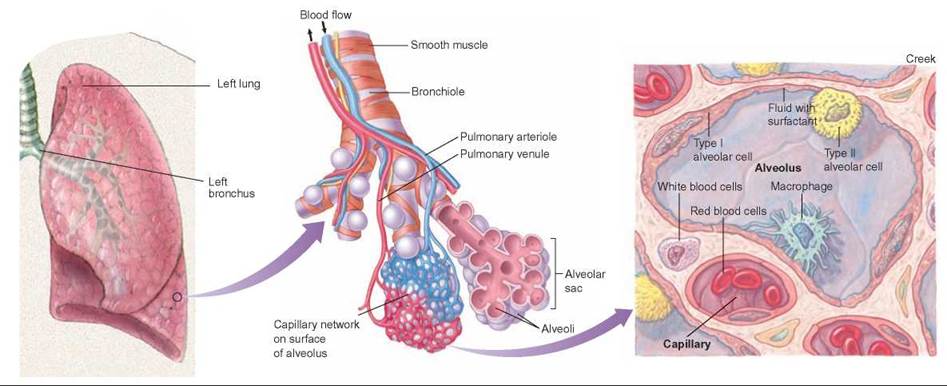
FIGURE 24.9. The Association of Capillaries with Alveoli
The exchange of gases takes place between the air-filled alveolus and the blood-filled capillary. The capillaries form a network around the saclike alveoli. The thin walls of the alveolus and capillary are in direct contact with one another; their combined thickness is usually less than 1 micrometer (a thousandth of a millimeter).
Another factor that increases the efficiency of gas exchange is that both the blood and the air are moving. Because blood is flowing through capillaries in the lungs, the capillaries continually receive new blood that is poor in oxygen and high in carbon dioxide. As blood passes by the alveoli, it is briefly exposed to the gases in the alveoli, where it gains oxygen and loses carbon dioxide. Thus, blood that leaves the lungs is high in oxygen and low in carbon dioxide. Although the movement of air in the lungs is not in one direction, as is the case with blood, the cycle of inhalation and exhalation allows air that is high in carbon dioxide and low in oxygen to exit the body and brings in new air that is rich in oxygen and low in carbon dioxide. This oxygen-rich, bright red blood is then sent to the left side of the heart and pumped throughout the body.
Any factor that interferes with the flow of blood or air or alters the effectiveness of gas exchange in the lungs reduces the efficiency of the organism. A poorly pumping heart sends less blood to the lungs, and the person experiences shortness of breath. Similarly, diseases such as asthma, which cause constriction of the bronchioles, reduce the flow of air into the lungs and inhibit gas exchange.
Any process that reduces the number of alveoli also reduces the efficiency of gas exchange in the lungs. For example, emphysema is a progressive disease in which some of the alveoli are lost. As the disease progresses, those afflicted have less and less respiratory surface area and experience greater and greater difficulty getting adequate oxygen, even though they may be breathing more rapidly. Often, emphysema is accompanied by an increase in the amount of connective tissue and the lungs do not stretch as easily, further reducing their ability to exchange gases.
24.4. CONCEPT REVIEW
7. Describe the muscles involved in breathing and explain how they cause air to flow into and out of the lungs.
8. How are CO2, blood pH, and breathing rate interrelated?
9. How do each of the following affect the efficiency of gas exchange in the lungs: poorly functioning heart, contracted bronchioles, reduced number of alveoli?