CONCEPTS IN BIOLOGY
PART VI. PHYSIOLOGICAL PROCESSES
27. Human Reproduction, Sex, and Sexuality
27.10. Contraception
Throughout history, people have tried various methods of conception control. In ancient times, conception control was encouraged during times of food shortage or when tribes were on the move from one area to another in search of a new home. Writings from as early as 1500 B.c. indicate that the Egyptians used a form of tampon medicated with the ground powder of a shrub to prevent fertilization. This may sound primitive, but we use the same basic principle today to destroy sperm in the vagina. As you read about the various methods of contraception, remember that no method except abstinence is 100% effective for avoiding pregnancy. Another important consideration is that only condoms are effective in preventing the spread of sexually transmitted diseases (STDs).
Barrier Methods
One way to prevent conception is to physically prevent the sperm from reaching the egg.
The male condom is probably the most popular contraceptive device. It is a thin sheath placed over the erect penis before intercourse. In addition to preventing sperm from reaching the egg, this physical barrier also helps prevent the transmission of the microbes that cause sexually transmitted diseases (STDs), such as syphilis, gonorrhea, and AIDS, from being passed from one person to another during sexual intercourse (Outlooks 27.3). The most desirable condoms are made of a thin layer of latex that does not reduce the sensitivity of the penis. Latex condoms have also been determined to be the most effective in preventing transmission of HIV. The condom is most effective if it is prelubricated with a spermicidal material, such as nonoxynol-9. This lubricant also has the advantage of providing some protection against the spread of HIV.

Condoms for women are also available. One, called the Femidom, is a polyurethane sheath, which, once inserted, lines the contours of the woman’s vagina.
It has an inner ring, which sits over the cervix, and an outer ring, which lies flat against the labia. Research shows that this device protects against STDs and is as effective a contraceptive as the condom used by men.

Other methods of conception control that prevent sperm from reaching the egg include the diaphragm, cervical cap, and sponge. A diaphragm is a specially fitted membranous shield that is inserted into the vagina before intercourse and positioned so that it covers the cervix, which has the opening of the uterus. Because of anatomical differences among females, diaphragms must be fitted by a physician. The diaphragm’s effectiveness is increased if spermicidal foam or jelly is also used. A cervical cap functions in a similar way. A contraceptive sponge, as the name indicates, is a small amount of absorbent material soaked in a spermicide. The sponge is placed within the vagina, where it chemically and physically prevents sperm cells from reaching the egg.

Chemical Methods
Contraceptive jellies and foams make the vaginal environment more acidic, which diminishes the sperm’s chances of survival. Spermicidal (sperm-killing) foam or jelly is placed in the
vagina before intercourse. When the sperm make contact with the acidic environment, they stop swimming and soon die. These methods of contraception are often used in combination with other methods of contraception (condoms, diaphragm etc.) as additional protection in the event that the other methods fail.
Hormonal Control Methods
The first successful method of hormonal control was “the pill,” or “birth-control pill,” which contained a combination of the hormones estrogen and progesterone. Today there are two kinds of birth-control pills: those that contain estrogen and progesterone and those that contain progesterone only. The combination birth-control pill works primarily by preventing ovulation, and secondarily by interfering with implantation. The quantity and balance of hormones (estrogen and progesterone) in the pill fools the ovaries into functioning as if the woman were already pregnant.
Therefore, ovulation does not occur, so conception is highly unlikely. The combination pills are taken daily for 21 days and then stopped (some brands have 21 pills with hormones and the last 7 do not contain hormones). This allows for menstruation to occur.

The progesterone-only pill (POP, or mini pill) is taken continuously without a break. The progesterone in these pills has several effects that helps to prevent conception. Progesterone thickens the mucus at the cervix, alters the uterine lining to make implantation unlikely, and appears to interfere with the movement of sperm and egg.
Other hormone methods involve delivering the hormones by way of implants, adhesive patches, or vaginal rings that slowly release hormones and prevent the maturation and release of eggs from the follicle. The major advantage of an implant is its convenience.
Once the implant has been inserted, the woman can forget about contraceptive protection for several years. If she wants to become pregnant, the implants are removed and her normal menstrual and ovulation cycles return over a period of weeks. Similarly, discontinuing the use of the patch allow normal ovulation to resume.

The vaginal ring releases a continuous low dose of estrogen and progestin for 21 days. At the end of the 21 days, the ring is removed for 7 days to allow the menstrual period to occur. A new ring is then inserted monthly.
Contraceptive hormones can also be used to stop menstrual periods, preventing the symptoms of premenstrual syndrome and improving a woman’s sex life.
The emergency contraceptive pill (ECP), or “morning-after pill,” uses a high dose of the same hormones found in oral contraceptives, which prevents the woman from becoming pregnant in the first place. In fact, “the pill” in higher dosages can be used as an ECP. The common medication available in the United States is known as Plan B®. These pills work by inhibiting ovulation and thickening mucus, which makes it difficult for the sperm to get to the egg.
OUTLOOKS 27.3
Sexually Transmitted Diseases
Sexually transmitted diseases (STDs) were formerly called venereal diseases (VDs). Although these kinds of illnesses are most frequently transmitted by sexual activity, many can also be spread by other methods of direct contact, such as hypodermic needles, blood transfusions, and blood-contaminated materials. Currently, the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, recognizes over 25 diseases as being sexually transmitted (table 27.A).
TABLE 27.A. Sexually Transmitted Diseases
Disease |
Agent |
Genital herpes |
Virus |
Gonorrhea |
Bacterium |
Syphilis |
Bacterium |
Acquired immunodeficiency syndrome (AIDS) |
Virus |
Candidiasis |
Yeast |
Chancroid |
Bacterium |
Genital warts |
Virus |
Gardnerella vaginalis |
Bacterium |
Genital Chlamydia infection |
Bacterium |
Genital cytomegalovirus infection |
Virus |
Genital Mycoplasma infection |
Bacterium |
Group B Streptococcus infection |
Bacterium |
Nongonococcal urethritis |
Bacterium |
Pelvic inflammatory disease (PID) |
Bacterium |
Molluscum contagiosum |
Virus |
Crabs |
Body lice |
Scabies |
Mite |
Trichomoniasis |
Protozoan |
Hepatitis B |
Virus |
Gay bowel syndrome |
Variety of agents |
The United States has the highest rate of sexually transmitted disease among the industrially developed countries. There are about 19 million new infections each year. About half of the infections occur in young adults aged 15-24 years of age. Table 27.B lists the most common STDs and estimates of the number of new cases each year. Some of the most important STDs are described here because of their high incidence in the population and the inability to bring some of them under control. For example, there is no known cure for HIV, responsible for AIDS.
TABLE 27.B. Cases of Sexually Transmitted Diseases in the United States Reported in 2008
Disease |
Cases Reported in 2008 |
Comments |
Chancroid |
25 |
|
Hepatitis B |
4,519 |
Up to 1.4 million people may have undiagnosed disease |
HIV/AIDS |
37,041 |
About 1.1 million people infected |
Syphilis |
46,277 |
Incidence is increasing |
Vaginal trichomoniasis |
204,000 |
Probably over 7 million cases/year |
Genital herpes |
292,000 |
About 16% of population infected (about 50 million) |
Gonorrhea |
336,742 |
700,000 cases/year estimated |
Genital warts |
385,000 |
About 1% of sexually active persons have genital warts |
Chlamydia |
1,213,523 |
Estimated 2.3 million infected |
Other vaginal infections |
3,571,000 |
Most common sexually transmitted disease |
Despite efforts to educate the public and the availability of effective methods for treatment, several STDs are actually increasing in frequency. In particular, Chlamydia infections have increased to over a million new infections per year. There has also been an increase in the number of cases of syphilis, especially among gay and bisexual men. In addition, a penicillin-resistant strain of Neisseria gonorrhoeae has led to an increase in the number of cases of gonorrhea.
The spread of STDs during sexual intercourse is significantly diminished by the use of condoms. Other types of sexual contact (e.g., hand, oral, anal) and transmission from a mother to the fetus during pregnancy help maintain some of these diseases in the population. Therefore, public health organizations, such as the U.S. Public Health Service, the CDC, and state and local public health agencies, regularly keep an eye on the number of cases of STDs. All of these agencies are involved in attempts to raise the general public health to a higher level. Their investigations have resulted in the successful control of many diseases and the identification of special problems, such as those associated with the STDs. Because the United States has an incidence rate of STDs that is 50 to 100 times higher than that of other industrially developed countries, there is still much that needs to be done.
The high-risk behaviors associated with contracting STDs include sex with multiple partners and the failure to use condoms. Whereas some STDs are simply inconvenient or annoying, others severely affect health and can result in death. As one health official stated, "We should be knowledgeable enough about our own sexuality and the STDs to answer the question, 'Is what I'm about to do worth dying for?'"
The Timing Method
Not all methods of birth control require the use of physical barriers, spermicides, or hormones. Any method that prevents sperm from reaching the egg prevents conception. One method is to avoid intercourse during the times of the month when an egg may be present. This is known as the rhythm method of conception control. Although at first glance it appears to be the simplest and least expensive, determining when an egg is likely to be present can be very difficult. A woman with a regular 28-day menstrual cycle typically ovulates about 14 days before the onset of the next menstrual flow. To avoid pregnancy, couples need to abstain from intercourse a few days before and after this date. However, if a woman has an irregular menstrual cycle, there may be only a few days each month for intercourse without the possibility of pregnancy. In addition to calculating safe days based on the length of the menstrual cycle, a woman can better estimate the time of ovulation by keeping a record of changes in her body temperature and vaginal pH. Both changes are tied to the menstrual cycle and can therefore help a woman predict ovulation. In particular, at about the time of ovulation, a woman has a slight rise in body temperature—less than 1°C. Thus, she should use an extremely sensitive thermometer. A digital-readout thermometer on the market spells out the word yes or no.
However, all variations of the rhythm method have high failure rates—up to 25 percent per year.
Intrauterine Devices (IUD)
The intrauterine device (IUD) is an object that must be fitted and inserted into the uterus by a physician. IUDs are very effective. This method of contraception has a failure rate of about 1%. How this device works is not completely known. There are two major kinds of IUDs: those that contain copper and those that contain the hormone progesterone. It appears that the copper interferes with the sperm’s swimming ability and also alters the lining of the uterus, which makes implantation unlikely. IUDs with progesterone appear to thicken the layer of mucus around the cervix and also alter the nature of the uterine lining, making implantation less likely. A major advantage of an IUD is that it can be left in place and be effective for years, but it can be removed if pregnancy is desired.
The IUD can also be used for “emergency contraception”— in cases of unprotected sex, forced sex, or the failure of a conception-control method (e.g., a broken condom). To be used for this purpose, the IUD must be inserted within 7 days of unprotected sex.

Surgical Methods
Two contraceptive methods that require surgery are tubal ligation and vasectomy (figure 27.19). Tubal ligation is the cutting and tying off of the oviducts; it can be done on an outpatient basis, in most cases. An alternative to sterilization by tubal ligation involves the insertion of small, flexible devices, called Micro-inserts, into each oviduct (fallopian tube). Once inserted, tissue grows into the inserts, blocking the tubes. Ovulation continues as usual, but the sperm and egg cannot unite.
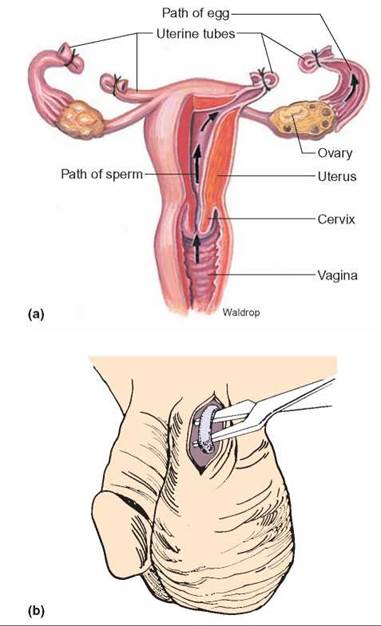
FIGURE 27.19. Tubal Ligation and Vasectomy
Two very effective contraceptive methods require surgery. (a) Tubal ligation involves severing the oviducts and suturing or sealing the cut ends. This prevents the sperm cell and the egg from meeting. This procedure is generally considered ambulatory surgery; at most, it requires a short hospitalization period. (b) Vasectomy requires minor surgery, usually in a clinic under local anesthesia. Following the procedure, minor discomfort may be experienced for several days. The severing and sealing of the vas deferens prevents the release of sperm cells from the body during ejaculation.
A vasectomy can be performed in a physician’s office. A small opening is made above the scrotum, and the spermatic cord (vas deferens) is cut and tied. This prevents sperm from moving through the ducts to the outside. Because most of the semen is produced by the seminal vesicles, prostate gland, and bulbourethral glands, a vasectomy does not interfere with normal ejaculation. The sperm that are still being produced die and are reabsorbed in the testes. Vasectomy is not the same as castration. Castration is the surgical removal of testes.
Neither tubal ligation nor vasectomy interferes with normal sex drives. However, these medical procedures are difficult to reverse and should not be considered by those who may want to have children at a future date. These procedures are not 100% effective since, in rare instances, the tubes might reattach, allowing gametes to pass from one severed side of the duct to the other.
27.10. CONCEPT REVIEW
21. Describe hormonal methods of conception control.
22. Describe barrier methods of conception control.