Biology of Humans
12a. Cardiovascular Disease
In the previous chapter, you examined the heart and blood vessels as they function in health. In this chapter, you will consider the problems that arise in some common cardiovascular diseases.
The Prevalence of Cardiovascular Diseases
Cardiovascular Disease and Cigarette Smoking
Cardiovascular disease is the single biggest killer of men and women in the United States. It affects slightly more men than women because, until menopause, women receive some natural protection from cardiovascular disease through the action of the sex hormone estrogen. Ironically, although slightly fewer women than men have heart attacks, women who do have heart attacks are twice as likely to die within the following weeks as are men. Because heart attacks are commonly thought of as a male problem, women and their physicians often fail to recognize the symptoms, thus delaying treatments that could be lifesaving.
High Blood Pressure
In the previous chapter, we learned that blood pressure is the outward pressure exerted by blood against the vessel walls. It must be high enough to circulate blood, but not so high that it stresses blood vessels. Recall that blood pressure is usually reported with two numbers. The first value—the systolic value—is the pressure when the heart is contracting. The second value, called the diastolic pressure, is the pressure when the heart is relaxing.
High blood pressure, or hypertension, is often called the silent killer. It is silent because it does not produce any telltale symptoms. It is a killer because it can cause fatal problems, usually involving the heart, brain, blood vessels, or kidneys. Hypertension damages the heart in a number of ways, primarily by causing the heart to work harder to keep the blood moving. In response, the heart muscle thickens, and the heart enlarges. The enlarged heart works less efficiently and has difficulty keeping up with the body's needs. At the same time, the increased workload increases the heart's need for oxygen and nutrients. If these cannot be delivered rapidly enough, a heart attack can result.
· A stress test reveals how the heart responds to exertion. This test can help you develop a healthful exercise program.
High blood pressure can also damage the kidneys, reducing the blood flow through them. In response, the kidneys make matters worse by secreting renin, a chemical that leads to further increases in blood pressure in an ever-escalating cycle.
Although about 90% of the cases of hypertension have no known cause, many contributing factors have been identified. When a cause can be identified, the kidneys are sometimes to blame. If kidneys have an impaired ability to handle sodium, the resulting fluid retention increases blood pressure by increasing blood volume. In other cases of hypertension, the sympathetic nervous system reacts too strongly to stress, constricting the blood vessels and increasing heart rate. Thus, more blood per minute is pumped through vessels that provide a greater resistance to flow.
Most physicians agree that a blood pressure of 160/90 is high and should be treated (see Figure 12a.1). But uncertainty clouds the treatment issue when the person's diastolic pressure is between 80 and 89—the higher end of normal. Although drug treatment may help in borderline cases, it usually must be continued for life. A diagnosis of high blood pressure may influence other aspects of a person's life, such as life insurance premiums. So, sometimes, only lifestyle changes are recommended for high normal values of blood pressure.
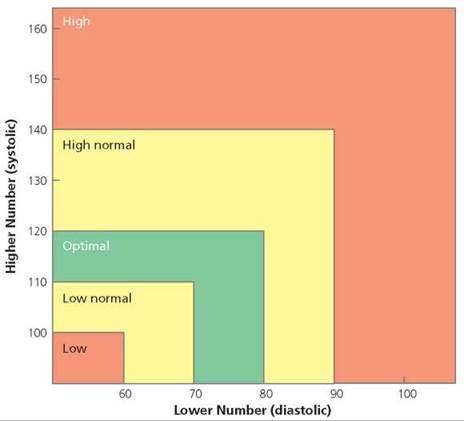
FIGURE 12a.1. Values of blood pressure in adults
When the diagnosis of hypertension is clear, one or more of various kinds of drugs can be prescribed, each type combating a different mechanism that contributes to high blood pressure. The diuretics, for instance, decrease blood volume by increasing the excretion of sodium and fluids, thereby reducing blood pressure by reducing blood volume. Other drugs cause the blood vessels to dilate (become wider), reducing hypertension in instances where is it caused by overly constricted vessels.
A number of changes in lifestyle are recommended to treat or prevent hypertension.
1. Control weight. Maintaining normal body weight can help control blood pressure. Many overweight people with high blood pressure benefit from shedding just a few extra pounds. The best way to lose weight is to eat a moderate, balanced diet; reduce fat intake; and increase physical activity.
2. Exercise regularly. Aerobic exercise, such as brisk walking, jogging, swimming, or cycling, performed for at least 20 minutes at least three times a week, helps lower blood pressure and keep it low.
3. Do not smoke. Cigarette smoke contains nicotine, a drug that increases heart rate and constricts blood vessels; both of those effects increase blood pressure.
4. Limit dietary salt. Some people with hypertension can lower their blood pressure by lowering the amount of salt in their diet. Salt can affect fluid retention and, therefore, blood volume.
Atherosclerosis
Atherosclerosis (ather-, yellow, fatty deposit; sclerosis, a hardening) is a buildup of fatty substances in the walls of arteries, fueled by an inflammatory response. In some cases, the deposits narrow the artery (Figure 12a.2). Such narrowing causes problems because it reduces blood flow through the vessel, choking off the vital supply of oxygen and nutrients to the tissues served by that vessel. But contrary to the beliefs held just a few years ago, atherosclerosis is more than just a plumbing problem, akin to a clog in a passive pipeline.
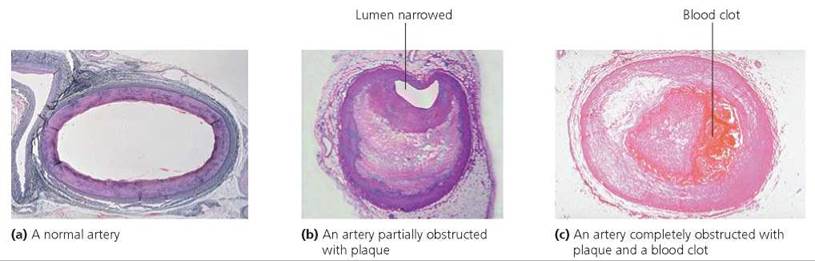
FIGURE 12a.2. Atherosclerosis, a low-level inflammatory response in the wall of an artery is associated with the formation of fat-filled plaques. Plaque can obstruct blood flow through the artery, thus depriving the cells that would be fed life-sustaining blood by the artery. Plaque can also rupture, causing a blood clot to form. The clot may then completely clog the vessel and cause the death of tissue downstream.
The inflammatory response thought to cause atherosclerosis is the same process that wards off infection when you scrape your knee (discussed in Chapter 13). In this case, it begins with an injury to the wall of an artery. The injury may be caused by some kind of bloodborne irritant (such as the chemicals inhaled in cigarette smoke), by cholesterol deposits in the artery lining, or by infection. Perhaps the excessively rapid or turbulent blood flow caused by high blood pressure can also produce such arterial damage. The damaged cells begin to pick up low-density lipoproteins (LDLs), the so-called bad form of cholesterol. This accumulation of LDLs is most likely to occur when the LDL concentration in the blood is high. The LDLs undergo chemical changes that stimulate the cells of the arterial lining to enlist the body's defense responses: inflammatory chemicals and defense cells. Growth factors produced by defense cells stimulate smooth muscle cells in the arterial wall to divide, thereby thickening the wall. Other defense cells engulf LDLs, become enlarged, and form fatty streaks on the arterial lining. As these defense cells continue to scavenge lipids, the fatty streak increases in size and forms plaque, a bumpy, fatty layer in the artery wall. The plaque can bulge into the artery channel, blocking the blood flow, or it can expand outward into the artery wall. Although the plaque has a fibrous cap that initially keeps pieces from breaking away, the fat-filled cells secrete inflammatory substances that weaken the cap. A small break in the cap can allow the plaque to rupture, which triggers the formation of a blood clot. In any case, restriction of the blood flow can starve and kill the cells lying downstream. Such an occurrence in the heart (leading to a heart attack) or brain (leading to a stroke) can be fatal. Because plaques do not necessarily bulge into the artery and cause symptoms of atherosclerosis before they rupture, heart attacks often occur in patients without previous symptoms.
There are several approaches to treating atherosclerosis. A healthy lifestyle promotes healthy arteries, so control your weight, engage in regular aerobic exercise, and eat a heart-healthy diet (see Chapter 15a). Medications to treat atherosclerosis include drugs to lower blood pressure, drugs to reduce blood cholesterol levels, and drugs to prevent unwanted blood clot formation. Some physicians recommend a daily dose of a low-strength aspirin, because aspirin reduces the risk of blood clot formation.
Stop and think
C-reactive protein (CRP) is an inflammatory chemical released by injured cells in the artery lining. Why might CRP prove to be a better predictor of atherosclerosis than blood cholesterol level?
Coronary Artery Disease
Coronary artery disease is a condition in which the fatty deposits associated with atherosclerosis form within coronary arteries, the arteries that nourish the heart muscle. Coronary artery disease is the underlying cause of the vast majority of heart attacks.
A temporary shortage of oxygen to the heart is accompanied by angina pectoris—chest pain, usually experienced in the center of the chest or slightly to the left. The name angina comes from the Latin word angere, meaning "to strangle." The name is apt, since the pain of angina is often described as suffocating, viselike, or choking. Typically, the pain begins during physical exertion or emotional stress, when the demands on the heart are increased and the blood flow to the heart muscle can no longer meet the needs. The pain stops after a period of rest. Angina serves as a warning that part of the heart is receiving insufficient blood through the coronary arteries, but it does not cause permanent damage to the heart. The warning should be taken seriously, however, because each year up to 15% of those people who have angina later die from a heart attack.
Although coronary artery disease is usually diagnosed from the symptoms of angina and a physical examination, a procedure called coronary angiography may be used to spot areas in the coronary arteries that have become narrowed by atherosclerosis. In this procedure, a contrast dye that is visible in x-rays is released in the heart, allowing the coronary vessels to be seen on film. A catheter (a slender, flexible tube) is inserted into an artery in the arm or leg and then threaded through the blood vessels until it reaches the heart. The dye is then squirted into the openings of the coronary arteries, and its movement through the arteries is recorded in a series of high-speed x-rays.
Coronary artery disease can be treated with medicines or with surgery. Among the medicines commonly used are some that dilate (widen) blood vessels, such as nitroglycerin. Certain other drugs specifically dilate only the coronary arteries. Wider blood vessels make it easier for the heart to pump blood through the circuit. When the coronary arteries dilate, more blood is delivered to the heart muscle. Also used are drugs that dampen the heart's response to stimulation from the sympathetic nervous system, thus decreasing its need for oxygen.
Two surgical operations for treating coronary artery disease are balloon angioplasty and coronary artery bypass. In angioplasty, the channel of an artery narrowed by soft, fatty plaque is widened by inflating a tough, plastic balloon inside the artery (Figure 12a.3). First the tiny, uninflated balloon is attached to the end of a catheter and inserted through an artery in the arm or upper thigh. It is then pushed to the blocked spot in a coronary artery; high-speed x-rays are used to track its progress. After it reaches the blockage, the balloon is inflated under pressure, stretching the artery and pressing the soft plaque against the wall to widen the lumen.
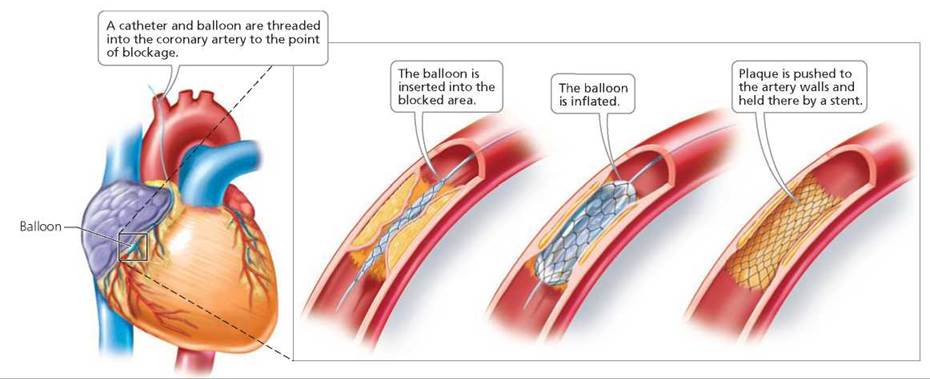
FIGURE 12a.3. Balloon angioplasty opens a partially blocked artery.
After angioplasty, physicians commonly insert a metal-mesh tube called a stent into the treated arteries. The stent prevents the arteries from collapsing and keeps loose pieces of plaque from being swept into the bloodstream. Although stents boost the percentage of arteries that stay open, they sometimes trigger an inflammatory response, and some arteries become clogged again, even with a stent in place. Some stents slowly release drugs that further reduce the risk that the artery will become blocked again.
A coronary bypass is a procedure in which a segment of a leg vein is removed and grafted so that it provides an alternate pathway that bypasses a point of obstruction between the aorta and a coronary artery (Figure 12a.4).
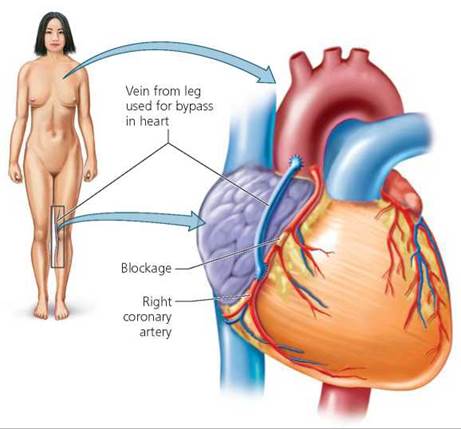
FIGURE 12a.4. In coronary bypass surgery, a section of a leg vein is removed. One end of the vein is attached to the heart’s main artery, the aorta, and the other to a coronary artery, bypassing the obstructed region. The grafted vein provides a pathway through which blood can reach the previously deprived region of heart muscle.
Stop and think
In a coronary bypass operation, why is it important for the surgeon to insert the grafted vein in the correct orientation? What would happen if the piece of vein were inserted backward?
Heart Attack
In a heart attack, technically known as a myocardial infarction, a part of the heart muscle dies because of an insufficient blood supply. (Myocardial refers to heart muscle; infarct refers to dead tissue.) Heart muscle cells begin to die if they are cut off from their essential blood supply for more than 2 hours. Depending on the extent of damage, the effects of a heart attack can spread quickly throughout the body: As a result of a heart attack, the brain receives insufficient oxygen; the lungs fill with fluid; and the kidneys fail. Within a short time, white blood cells swarm in to remove the damaged heart tissue. Then—if the individual survives—over the next 8 weeks or so, scar tissue replaces the dead cardiac muscle (Figure 12a.5). Because scar tissue cannot contract, part of the heart permanently loses its pumping ability.
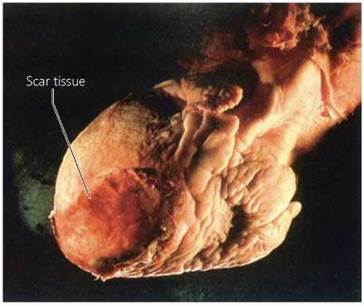
FIGURE 12a.5. The ravages of a prior heart attack are visible as scar tissue at the bottom of this lifeless heart. Scar tissue replaced cardiac muscle when the blood supply to the heart muscle was shut down. Because scar tissue cannot contract, that part of the life-sustaining pump becomes ineffective.
Heart attacks can be caused in many ways. The most common type of heart attack is a coronary thrombosis, which means the attack is caused by a blood clot blocking a coronary artery. Coronary thrombosis is unlikely to happen unless the artery already contains plaques of atherosclerosis, as occurs in coronary artery disease. In some instances, the blood clot is formed elsewhere in the body but is swept along in the bloodstream until it lodges in a coronary artery. In other instances of heart attacks, the blockage is temporary, caused by constriction of a coronary artery, called a coronary artery spasm.
Chest pain is a common indication that a heart attack is in progress, especially in men. Unlike angina, the pain is not necessarily brought on by activity, and it doesn't go away with rest. In some cases, the victim feels a severe, crushing pain that begins in the center of the chest and often spreads down the inside of one or both arms (most commonly the left one) as well as up to the neck and shoulders. Although the pain is usually severe enough to cause the victim to stop whatever he or she is doing, it is not always so strong that it is recognized as a sign of heart attack. A heart attack may also cause nausea and dizziness, which can prompt the victim to interpret the symptoms as an upset stomach. Oddly, persons who experience severe pain may be the lucky ones, because they are more likely to realize they are having a heart attack and seek immediate help. Doubt about the cause of the symptoms is unfortunate because it often delays treatment, and treatment within the first few hours after a heart attack can make the difference between life and death.
If a large enough section of heart muscle is damaged by a heart attack, the heart may not be able to continue pumping blood to the lungs and the rest of the body at an adequate rate. A condition in which the heart is no longer an efficient pump is known as heart failure. Symptoms of heart failure include shortness of breath, fatigue, weakness, and fluid accumulation in the lungs or limbs. Although the heart can never be restored to its former health, the symptoms of heart failure can be treated with drugs. For instance, digitalis can increase the strength of heart contractions, and diuretics reduce fluid accumulation, thus lessening the heart's workload. Other drugs relax constricted arteries, thereby reducing resistance to blood flow and lowering the blood pressure. Together, these drugs help a weakened heart pump more efficiently.
Sometimes, drugs and bypass surgery cannot halt progressive heart failure. In this case, heart transplant surgery may provide hope for some patients, but generally only for those younger than 80 years of age. First, a donor heart must be found whose tissue is an acceptable match with that of the recipient. During transplant surgery, a heart-lung machine takes over the circulation while the weakened heart is removed, and the new heart is sewn in place. The patient is then treated with drugs that lessen the chances of organ rejection (discussed in Chapter 13).
Cardiovascular Disease and Cigarette Smoking
When we think about the hazards of tobacco smoke, lung cancer generally leaps to mind. But the increased risk of cardiovascular (heart and blood vessel) disease is even more significant. Each year, cardiovascular disease kills many more people than does lung cancer, and smokers have a twofold to threefold increase in the risk of heart disease (Figure 12a.6). The American Heart Association estimates that about 25% of all fatal heart attacks are caused by cigarette smoke. This translates to roughly 200,000 heart attacks a year in the United States that could have been prevented by not smoking.
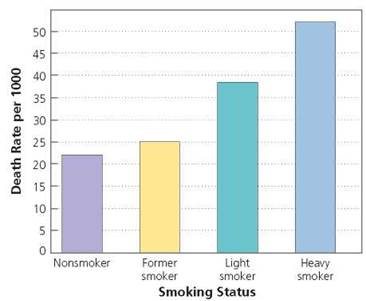
FIGURE 12a.6. Death rates due to heart disease among nonsmokers and smokers. Notice that the death rate from heart disease increases with the number of cigarettes smoked per day. People who smoke over a pack per day (heavy smokers) have more than twice the risk of death due to heart disease than do people who have never smoked. In any case, a smoker who successfully quits is much less likely to die of heart disease than if the smoking habit continues.
Nicotine and carbon monoxide in cigarette smoke stress the heart and blood vessels in many ways. Nicotine makes the heart beat faster and constricts blood vessels, raising blood pressure. In addition, nicotine makes platelets, the cell fragments responsible for blood clotting, stick together, increasing the risk of forming abnormal blood clots. The resulting clots may break loose from the site where they form and travel through the bloodstream until they lodge in a small vessel and block the blood flow. These blockages may result in a heart attack or stroke.
The amount of carbon monoxide in cigarette smoke is 1600 ppm (parts per million), which greatly exceeds the 10 ppm considered dangerous in industry. Furthermore, carbon monoxide from smoking a cigarette lingers in the bloodstream for up to 6 hours. You may recall from Chapter 11 that carbon monoxide is a poison that prevents red blood cells from transporting oxygen. In fact, carbon monoxide from smoking a cigarette lowers the oxygen-carrying capacity of the blood by about 12%, reducing oxygen delivery to every part of the body, including the brain and heart. Thus, the heart must work harder to deliver oxygen to the cells. The diminished oxygen supply to the brain can impair judgment, vision, and attentiveness to sounds. For these reasons, smoking can be hazardous for drivers.
A less immediate but no less important way that smoking leads to cardiovascular disease is by increasing the risk of developing atherosclerosis. Smoking influences atherosclerosis in two ways. One is by decreasing the levels of protective cholesterol-transport particles, called HDLs, that carry cholesterol to the liver, perhaps even removing cholesterol from cells, so that it can be eliminated from the body. With fewer HDLs, more cholesterol begins to clog the arteries. A second way that smoking promotes cholesterol deposits is by raising blood pressure. The elevated blood pressure causes rapid, turbulent blood flow that damages the walls of the arteries, making them more susceptible to cholesterol deposit. The cholesterol deposits cause inflammation, which leads to atherosclerosis. The narrowing of blood vessels caused by atherosclerosis leads to starvation of tissue downstream and an increase in blood pressure. When atherosclerotic deposits form in the arteries that supply blood to the heart, as they often do, the blood supply to the heart may be reduced or shut down completely, causing heart cells to die.
The cardiovascular system benefits from quitting smoking within 5 years. In regard to heart disease, 61% of the full benefit of quitting smoking is gained within 5 years. And, 42% of the full benefit of reduced risk of stroke is gained within 5 years.
Looking ahead
In this chapter, we learned about cardiovascular disease. In the next chapter, we will consider how the body defends itself against infectious disease.