THE LIVING WORLD
Unit Six. Animal Life
22. The Animal Body and How It Moves
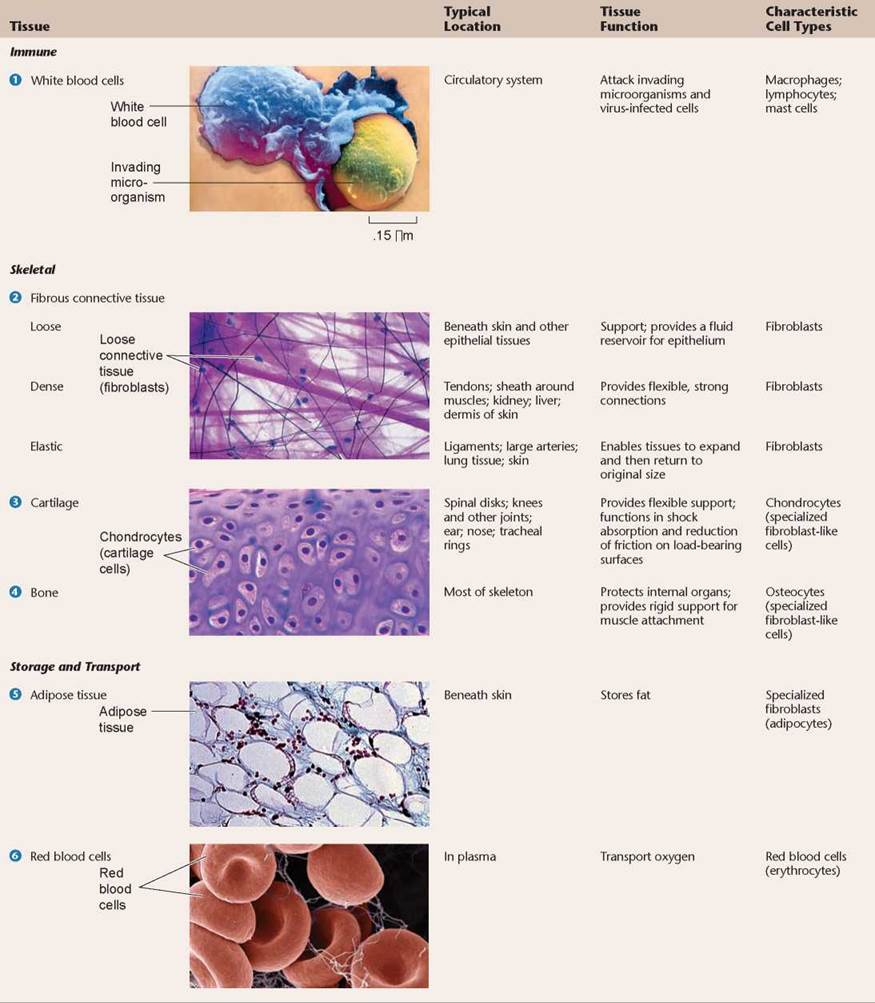
22.4. Connective Tissue Supports the Body
The cells of connective tissue provide the vertebrate body with its structural building blocks and also with its most potent defenses. Derived from the mesoderm, these cells are sometimes densely packed together, and sometimes widely dispersed, just as the soldiers of an army are sometimes massed together in a formation and sometimes widely scattered as guerrillas. Connective tissue cells fall into three functional categories: (1) the cells of the immune system, which act to defend the body; (2) the cells of the skeletal system, which support the body; and (3) the blood and fat cells, which store and distribute substances throughout the body. While grouping these diverse types of cells together may seem odd, all connective tissues share a common structural feature: They all have abundant extracellular “matrix” material between widely spaced cells.
Immune Connective Tissue
The cells of the immune system, the many kinds of so-called “white blood cells” (1 in table 22.3), roam the body within the bloodstream. They are mobile hunters of invading microorganisms and cancer cells. The two principal kinds of immune system cells are macrophages, which engulf and digest invading microorganisms (as shown in the photo in table 22.3), and lymphocytes, which make antibodies or attack virus-infected cells. Immune cells are carried through the body in a fluid matrix called plasma.
Skeletal Connective Tissue
Three kinds of connective tissue are the principal components of the skeletal system: fibrous connective tissue, cartilage, and bone. Although composed of similar cells, they differ in the nature of the matrix that is laid down between individual cells.
1. Fibrous connective tissue. The most common kind of connective tissue in the vertebrate body, fibrous connective tissue 2, is composed of flat, irregularly branching cells called fibroblasts that secrete structurally strong proteins into the spaces between the cells. The different types of proteins they contain give these tissues different strengths. Loose connective tissue, pictured in table 22.3, provides the least amount of strength. Dense connective tissue is very strong, while elastic connective tissue provides strength and the ability to stretch and recoil. The most commonly secreted protein, collagen, is the most abundant protein in the human body—in fact, one-quarter of all the protein in your body is collagen! Fibroblasts are also active in wound healing; scar tissue, for example, possesses a collagen matrix.
2. Cartilage. In cartilage 3, a collagen matrix between cartilage cells (technically called chondrocytes) forms in long parallel arrays along the lines of mechanical stress. What results is a firm and flexible tissue of great strength, just as strands of nylon molecules laid down in long, parallel arrays produce strong, flexible ropes. Cartilage makes up the entire skeletal system of the modern agnathans and cartilaginous fishes. In most adult vertebrates, however, cartilage is restricted to the articular (joint) surfaces of bones that form freely movable joints and to other specific locations.
3. Bone. Bone 4 is similar to cartilage, except that the collagen fibers are coated with a calcium phosphate salt, making the tissue rigid. The structure of bone and the way it is formed are discussed shortly.
Storage and Transport Connective Tissue
The third general class of connective tissue is made up of cells that are specialized to accumulate and transport particular molecules. They include the fat-accumulating cells of adipose tissue 5. The large, seemingly empty areas in the adipose tissue in table 22.3 are actually fat-containing vacuoles within the adipose cells. Red blood cells 6, called erythrocytes, also function in transport and storage. About 5 billion erythrocytes are present in every milliliter of your blood. Erythrocytes transport oxygen and carbon dioxide in blood. They are unusual in that during their maturation they lose most of their organelles, including the nucleus, mitochondria, and endoplasmic reticulum. Instead, occupying the interior of each erythrocyte are about 300 million molecules of hemoglobin, the protein that carries oxygen.
The fluid, or plasma, in which erythrocytes move is both the “banquet table” and the “refuse heap” of the vertebrate body. Practically every substance used by cells is dissolved in plasma, including inorganic salts like sodium and calcium, body wastes, and food molecules like sugars, lipids, and amino acids. Plasma also contains a wide variety of proteins, including antibodies and albumin, which gives the blood its viscosity.
TABLE 22.3. CONNECTIVE TISSUE
A Closer Look at Bone
The vertebrate endoskeleton is strong because of the structural nature of bone. Bone consists of living bone cells embedded within an inert matrix composed of the structural protein collagen and several minerals, including a calcium phosphate salt called hydroxyapatite. Bone is produced by coating collagen fibers with hydroxyapatite; the result is a material that is strong without being brittle. To understand how coating collagen fibers with calcium salts makes such an ideal structural material, consider fiberglass. Fiberglass is composed of glass fibers embedded in epoxy glue. The individual fibers are rigid, giving great strength, but they are also brittle. The epoxy glue, on the other hand, is flexible but weak. The composite, fiberglass, is both strong and flexible because when stress causes an individual fiber to break, the crack runs into glue before it reaches another fiber. The glue distorts and reduces the concentration of the stress—in effect, the glue spreads the stress over many fibers.
The construction of bone is similar to that of fiberglass: Small, needle-shaped crystals of a calcium phosphate mineral, hydroxyapatite, surround and impregnate collagen fibers within bone. No crack can penetrate far into bone because any stress that breaks a hard hydroxyapatite crystal passes into the collagenous matrix, which dissipates the stress. The hydroxyapatite mineral provides rigidity, whereas the collagen “glue” provides flexibility.
Most of us think of bones as solid and rocklike. But actually, bone is a dynamic tissue that is constantly being reconstructed. The cross section through a bone in figure 22.4 shows that the outer layer of bone is very dense and compact and so is called compact bone. The interior is less compact, with a more open lattice structure, and is called spongy bone. Red blood cells form in the red marrow of spongy bone. New bone is formed in two stages: First, collagen is secreted by cells called osteoblasts, which lay down a matrix of fibers along lines of stress. Then calcium minerals impregnate the fibers. Bone is laid down in thin, concentric layers, like layers of paint on an old pipe. The layers form as a series of tubes around a narrow central channel called a central canal, also called a Haversian canal, which runs parallel to the length of the bone. The many central canals within a bone, all interconnected, contain blood vessels and nerves that provide a lifeline to its living, bone-forming cells.
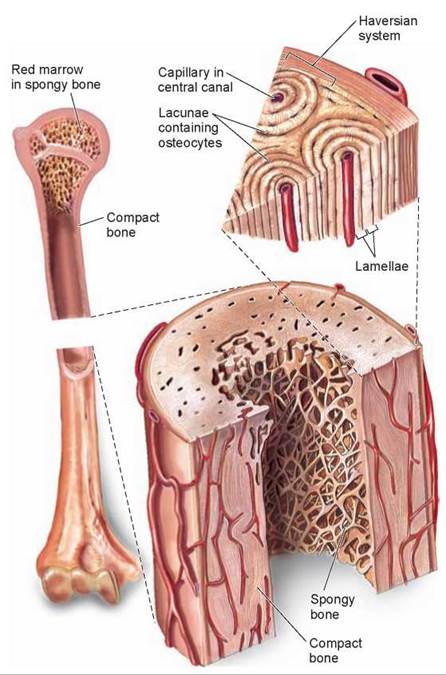
Figure 22.4. The structure of bone.
Some parts of bones are dense and compact, giving the bone strength. Other parts are spongy, with a more open lattice; red blood cells form in the bone marrow. Osteocytes, which are mature osteoblasts, lie in tight spaces called lacunae.
When bone is first formed in the embryo, osteoblasts use a cartilage skeleton as a template for bone formation. During childhood, bones grow actively. The total bone mass in a healthy young adult, by contrast, does not change much from one year to the next. This does not mean change is not occurring. Large amounts of calcium and thousands of osteocytes (mature osteoblasts) are constantly being removed and replaced, but total bone mass does not change because deposit and removal take place at about the same rate.
Two cell types are responsible for this dynamic bone “remodeling”: Osteoblasts deposit bone, and osteoclasts secrete enzymes that digest the organic matrix of bone, liberating calcium for reabsorption by the bloodstream (see figure 30.9). The dynamic remodeling of bone adjusts bone strength to workload, new bone being formed along lines of stress. When a bone is subjected to compression, mineral deposition by osteoblasts exceeds withdrawals by osteoclasts. That is why long-distance runners must slowly increase the distances they attempt, to allow their bones to strengthen along lines of stress; otherwise, stress fractures can cripple them.
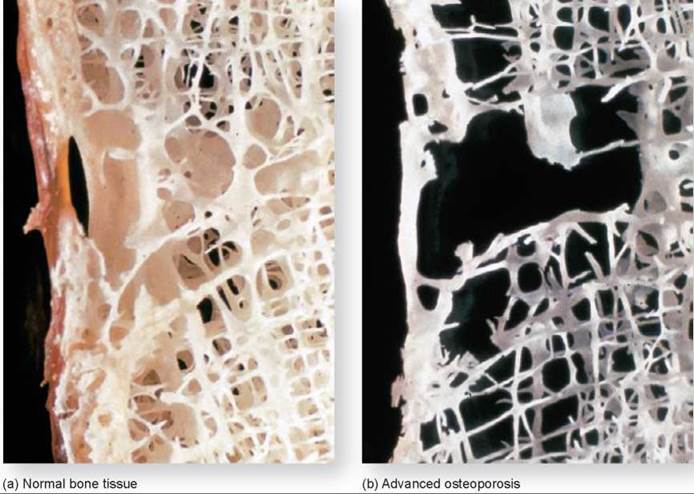
As a person ages, the backbone and other bones tend to decline in mass. Excessive bone loss is a condition called osteoporosis. After the onset of osteoporosis, the replacement of calcium and other minerals lags behind withdrawal, causing the bone tissue to gradually erode. Eventually the bones become brittle and easily broken. Figure 22.5 shows the effects of osteoporosis in both men and women. Women are more than twice as likely to develop osteoporosis compared to men.
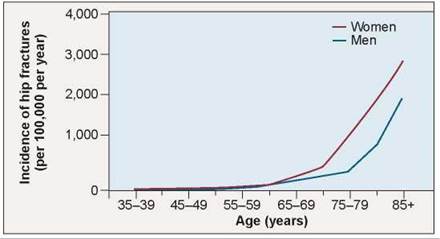
Figure 22.5. Osteoporosis.
More common in older women than in younger women or men, osteoporosis is a bone disorder in which bones progressively lose minerals. This graphs shows the incidence of osteoporotic hip fractures in men and women.
Key Learning Outcome 22.4. Connective tissues support the vertebrate body and consist of cells embedded in an extracellular matrix. They include cells of the immune system, cells of the skeletal system, and cells found throughout the body like blood and fat cells. Bone is a type of connective tissue.
Biology and Staying Healthy
Losing Bone: Osteoporosis
Running, jumping, swimming, flying, even squirming through the mud—all are things that animals do. A distinguishing characteristic of animals is this ability to move from place to place. Animals are the only true multicellular organisms capable of traveling around or through their environment. As you will discover later in this chapter, vertebrates like us accomplish this feat through the action of muscles pulling against an internal skeleton made of bone.
The bones that make up your skeleton are not lifeless, like the scaffolding of a building, but rather living tissue that continues to grow and change throughout your life. Just because you reach your full height does not mean that your bones stop growing. They stop elongating, but that is merely one aspect of bone growth. Every day of your life, your bones are adding new tissue and breaking down old tissue, reshaping your skeleton to meet the needs of your body. If you break a bone, your body heals the fracture by adding new bone tissue at the site of the break. However, when the process of forming new bone is impaired, the bone becomes weak and unable to heal itself.
A striking example of the impact of this failure of bone healing is exhibited by the little old lady that you might see walking down the street with a hunched back.
The bump on her back is caused by an imbalance in bone metabolism, rather than poor posture. As a person ages, the backbone, hips, and other bones tend to lose bone mass much faster than new bone mass is produced. Excessive bone loss is a condition called osteoporosis (also discussed on page 484). A section of normal bone is shown on the left below. A section of bone from a patient with osteoporosis is shown on the right below. You can see how much less bone tissue is present in the patient with osteoporosis.
Unfortunately for the person suffering from osteoporosis, even everyday activities such as bending or lifting can result in a broken bone. The little old lady with the humped back has already experienced multiple bone fractures in her spine. Although we often refer to it as the "backbone,” the spine is not one bone but rather a column of many smaller bones stacked one on top of the other, like building blocks. The spine holds the upper body erect, and in a person with osteoporosis, just the stress of the body's weight on the weakened bones causes small fractures up and down the spine. Multiple spine fractures can result in a curvature of the back and a stooped posture. A loss of height of an inch or more is often an early sign of osteoporosis.
How does a person know if he or she has osteoporosis? Unfortunately, a fractured bone is usually the primary warning sign of osteoporosis. There are diagnostic tests that can check a person's bone density, but they often aren't done unless a person experiences a fracture. A bone density test should be performed when a person over age 45 breaks a bone or in a person less than age 45 who has had several fractures.
The test used to diagnose osteoporosis, a bone density test, measures the density, or mass, of the bones. The hips, spine, and wrists are often used for evaluation because these are the bones most commonly broken due to osteoporosis.
A bone density test called DXA, for dual X-ray absorptiometry, is considered the gold standard test for diagnosing osteoporosis and monitoring bone loss over time. The test is a noninvasive low-dose X-ray. Actually, two X-rays of different energy levels (or wavelengths) are used to differentiate between bone and soft tissue. This provides a very accurate measurement of bone density. The bone density of the patient is compared to that of a healthy 30-year- old, which is when bone density is highest in both male and females, and a number known as a T-score is assigned. A T-score of 1 or above is normal. A negative T-score indicates that some bone loss has occurred. A number between -2.5 and -1 suggests an increased risk of fractures with a 10% to 30% loss in bone density, while a value below -2.5 indicates osteoporosis.
Osteoporosis is often called a "silent disease” because symptoms usually aren't apparent until a fracture occurs. However, one out of every two women over 50 years of age experiences clinical bone loss to some degree. The incidence of osteoporosis is considerably less in men, with about one out of every four men experiencing bone loss. Over 10 million people in the United States have osteoporosis, with twice that many at risk. Osteoporosis causes about 1.5 million fractures a year in men and women, with spine and hip fractures making up the majority of these.
Of the 10 million Americans affected by osteoporosis, over 80% are older women. Osteoporosis is most prevalent in postmenopausal women over the age of 50. As you will discover in chapter 30, the process of building up bone and breaking it down is controlled by various hormones, chemical signals released into the bloodstream that control body functions. As a woman's body experiences changes in various hormone levels after menopause, some body functions, including the cyclic building up and breaking down of bone tissue, are altered. Other factors also contribute to osteoporosis including family history, inadequate sources of calcium and vitamin D in the diet, smoking, ethnicity (Caucasian and Asian women have a higher risk), and lack of exercise.

How to Avoid Osteoporosis
Is osteoporosis unavoidable? Not at all. Doctors are learning more and more about osteoporosis and how to treat it, and importantly, how to prevent it. Although it is a disease found most frequently in the elderly, it can be prevented by actions taken when a person is younger.
How can you avoid osteoporosis later in life? The "sculpting” of bone occurs throughout your lifetime, but it is in your childhood and teenage years when new bone is added at a faster rate than it is lost by the breakdown of bone tissue. This net addition of bone tissue continues until a person reaches about 30 years of age, when the balance begins to tip toward the direction of bone loss. Osteoporosis develops when the rate of bone loss exceeds the replacement of bone to the point when the bone becomes weak and brittle.
As discussed on page 480, bone forms when calcium phosphate hardens around collagen fibers, and so an adequate supply of calcium is important to healthy bone development. Because of this, it is important that children and teenagers have enough calcium in their diets to fulfill the needs of developing bone, as well as other body activities that require calcium.
Therefore, the best way to avoid osteoporosis in your elder years is to get ample amounts of calcium before you're 30. Building up strong, healthy, dense bones before age 30 means that you have a larger pool of calcium in your bones to offset bone loss in your older years. As people age, their bodies are less efficient at absorbing calcium and so people over age 50 actually need to increase their calcium intake to 1,200 mg per day. Foods high in calcium include low-fat dairy products, dark green leafy vegetables, and orange juice. Many people take calcium supplements to ensure that they get enough calcium.
Physical activity is also key to preventing osteoporosis, but it is important that the activity involves weight-bearing exercise such as walking or jogging. New bone tissue is added to areas of the bone that are stressed to make those areas stronger. Weight-bearing exercises, both in young and old, help to strengthen areas of the bone that might be most susceptible to fractures.
While successful treatments are available, it is important to remember that the best treatment for osteoporosis is to avoid getting it by building up your bones when you're young.