THE LIVING WORLD
Unit Six. Animal Life
31. Reproduction and Development
31.5. Hormones Coordinate the Reproductive Cycle
The female reproductive cycle, called a menstrual cycle, is composed of two distinct phases: the follicular phase, in which an egg reaches maturation and is ovulated, and the luteal phase, where the body continues to prepare for pregnancy. These phases are coordinated by a family of hormones. Hormones play many roles in human reproduction. Sexual development is initiated by hormones, released from the anterior pituitary and ovary, that coordinate simultaneous sexual development in many kinds of tissues. The production of gametes is another closely orchestrated process, involving a series of carefully timed developmental events. Successful fertilization initiates yet another developmental “program,” in which the female body continues its preparation for the many changes of pregnancy.
Production of the sex hormones that coordinate all these processes is coordinated by the hypothalamus, which sends releasing hormones to the pituitary, directing it to produce particular sex hormones. Negative feedback, discussed in chapter 30, plays a key role in regulating these activities of the hypothalamus. When target organs receive a pituitary hormone, they begin to produce a hormone of their own, which circulates back to the hypothalamus, shutting down production of the pituitary hormone. In addition, positive feedback mechanisms play a role too. In these cases, a hormone circulates back to the hypothalamus and increases the production of a pituitary hormone.
Triggering the Maturation of an Egg
The first phase of the menstrual cycle, the follicular phase, corresponds to days 0 through 14 in figure 31.18. During this time, several follicles (an oocyte and its surrounding tissue is called a follicle) are stimulated to develop. This development is carefully regulated by hormones. The anterior pituitary, after receiving a chemical signal (GnRH) from the hypothalamus, starts the cycle by secreting small amounts of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) 1. These hormones stimulate follicular growth 2 and the secretion of the female sex hormone estrogen 3, more technically known as estradiol, from the developing follicles. Several follicles are stimulated to grow under FSH stimulation.
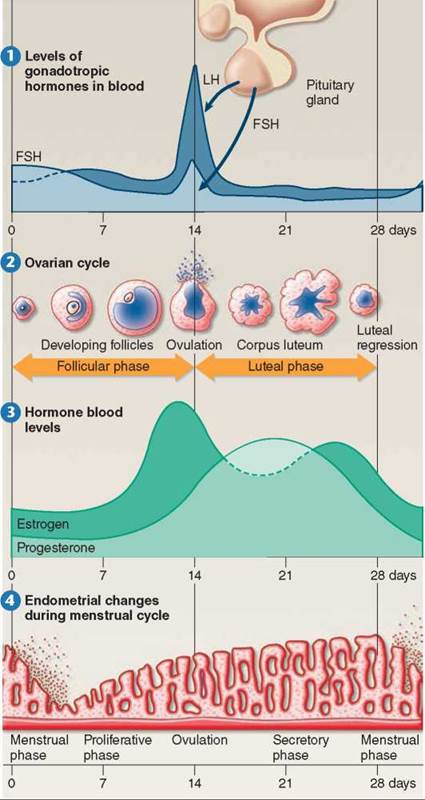
Figure 31.18. The human menstrual cycle.
Ovulation and the preparation of the uterine lining for implantation is controlled by a group of four hormones during the menstrual cycle.
Initially, the relatively low levels of estrogen have a negative-feedback effect on FSH and LH secretion. The low but rising levels of estrogen in the bloodstream feed back to the hypothalamus, which responds to the rising estrogen by commanding the anterior pituitary to decrease production of FSH and LH. As FSH levels fall, usually only one follicle achieves maturity. Late in the follicular phase, estrogen levels in the blood have increased drastically, and these higher levels of estrogen begin to have a positive-feedback effect on FSH and LH secretion. The rise in estrogen levels signals the completion of the follicular phase of the menstrual cycle.
Preparing the Body for Fertilization
The second phase of the cycle, the luteal phase (days 14 through 28), follows smoothly from the first. In a positive- feedback response to high levels of estrogen, the hypothalamus causes the anterior pituitary to rapidly secrete large amounts of LH and FSH (see day 14 in 1). The surge of LH is larger than the surge of FSH and can last up to 24 hours. The peak in LH secretion triggers ovulation: LH causes the wall of the follicle to burst, and the egg within the follicle is released into one of the fallopian tubes extending from the ovary to the uterus (see 1 in figure 31.19).
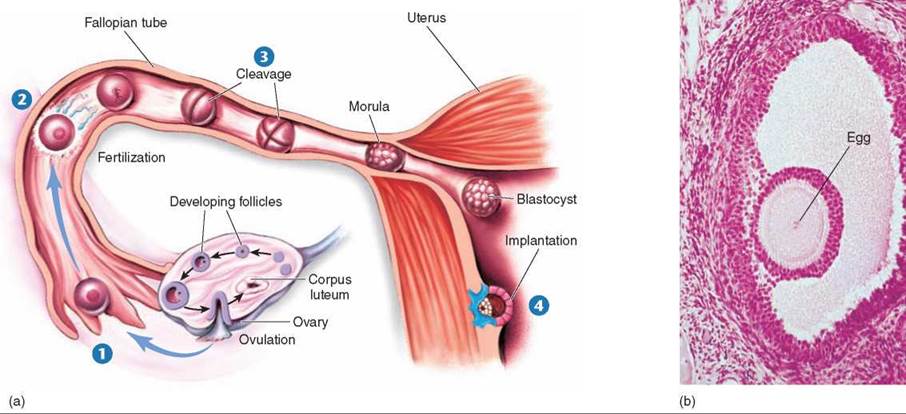
Figure 31.19. The journey of an ovum.
(a) Produced within a follicle and released at ovulation, an ovum is swept up into a fallopian tube 1 and carried down by waves of contraction of the tube walls. Fertilization occurs within the tube 2, by sperm journeying upward. Several mitotic divisions occur while the fertilized ovum undergoes cleavage and continues its journey down the fallopian tube 3, becoming first a morula then a blastocyst. The blastocyst implants itself within the wall of the uterus 4, where it continues its development. (b) A mature egg within an ovarian follicle. In each menstrual cycle, a few follicles are stimulated to grow under the influence of FSH and LH, but usually only one achieves full maturity and ovulation.
After the egg’s release and departure, estrogen levels decrease, and LH directs the repair of the ruptured follicle, which fills in and becomes yellowish. In this condition, it is called the corpus luteum, which is simply the Latin phrase for “yellow body.” The corpus luteum soon begins to secrete the hormone progesterone (the light green curve in figure 31.18 3), in addition to small levels of estrogen. Increased levels of progesterone and estrogen have a negative-feedback effect on the secretion of FSH and LH, preventing further ovulations. Progesterone completes the body’s preparation of the uterus for fertilization including the thickening of the endometrium (figure 31.18 4). If fertilization does not occur soon after ovulation, however, production of progesterone slows and eventually ceases, marking the end of the luteal phase. The decreasing levels of progesterone cause the thickened layer of blood-rich tissue to be sloughed off, a process that results in the bleeding associated with menstruation.Menstruation, or “having a period,” usually occurs about midway between successive ovulations (shown in figure 31.18 at 28 days), although its timing varies widely for individual females.
At the end of the luteal phase, neither estrogen nor progesterone is being produced. In their absence, the anterior pituitary can again initiate production of FSH and LH, thus starting another reproductive cycle. Each cycle begins immediately after the preceding one ends. A cycle usually occurs every 28 days, or a little more frequently than once a month, although this varies in individual cases. The Latin word for “month” is mens, which is why the reproductive cycle is called the menstrual cycle, or monthly cycle.
If fertilization does occur high in the fallopian tube (2 in figure 31.19), the zygote undergoes a series of cell divisions called cleavage 3, while traveling toward the uterus. At the blastocyst stage, it implants in the lining of the uterus 4. The tiny embryo secretes human chorionic gonadotropin (hCG), an LH-like hormone, which maintains the corpus luteum. By maintaining the corpus luteum, hCG keeps the levels of estrogen and progesterone high, thereby preventing menstruation, which would terminate the pregnancy. Because hCG comes from the embryo and not from the mother, it is hCG that is tested in all pregnancy tests.
Key Learning Outcome 31.5. Humans and apes have menstrual cycles driven by cyclic patterns of hormone secretion and ovulation. The cycle is composed of two distinct phases, follicular and luteal, coordinated by a family of hormones.