THE LIVING WORLD
Unit Six. Animal Life
31. Reproduction and Development
31.8. Contraception and Sexually Transmitted Diseases
Contraception
Not all couples want to initiate a pregnancy every time they have sex, yet sexual intercourse may be a necessary and important part of their emotional lives together. The solution to this dilemma is to find a way to avoid reproduction without avoiding sexual intercourse, an approach that is commonly called birth control, or contraception.
Abstinence. The simplest and most reliable way to avoid pregnancy is not to have sex at all. Of all methods of birth control, this is the most certain—and the most limiting, because it denies a couple the emotional support of a sexual relationship. A variant of this approach is to avoid sex only on the days when successful fertilization is likely to occur. The rest of the sexual cycle is considered relatively “safe” for intercourse. This approach, called the rhythm method, or natural family planning, when other indicators are also monitored, is satisfactory in principle but difficult in application because ovulation is not easy to predict and may occur unexpectedly. Failure rate can be as high as 20% to 30%.
Prevention of Egg Maturation A widespread form of birth control in the United States has been the daily ingestion of hormones, or birth control pills. These pills contain estrogen and progesterone, which shut down production of the pituitary hormones FSH and LH. The ovarian follicles do not ripen in the absence of FSH, and ovulation does not occur in the absence of LH. Other methods of hormone delivery include medroxy progesterone (Depo-Provera), which is injected every one to three months, the seven-day birth control patch, which releases the hormones through the skin, and surgically implanted capsules that release hormones. Failure rates of these methods are less than 2%.
Emergency contraception, called Plan B, is a high-dose progesterone pill that can block ovulation if taken soon after unprotected sex. Its failure rate varies and should not be used as a primary method of birth control.
Prevention of Embryo Implantation. The insertion of a coil or other irregularly shaped object into the uterus is an effective means of birth control. The irritation in the uterus prevents the implantation of the descending embryo within the uterine wall. Such intrauterine devices (IUDs) are very effective because once they are inserted, they can be forgotten. They have a failure rate of less than 2%,
A chemical means of preventing embryo implantation or ending an early pregnancy is RU-486. This pill blocks the action of progesterone, causing the endometrium to slough off. RU-486 must be administered under a doctor’s care because of potentially serious side effects.
Sperm Blockage. Fertilization cannot occur without sperm. One way to prevent the delivery of sperm is to encase the penis within a thin rubber bag, or condom. In principle, this method is easy to apply and foolproof, but in practice, it proves to be less effective than you might expect, with a failure rate of up to 15%. A second way to prevent the entry of sperm is to cover the cervix with a rubber dome called a diaphragm, inserted immediately before intercourse. Because the dimensions of individual cervices vary, diaphragms must be fitted by a physician. Failure rates average 20%.
Sperm Destruction. A third general approach to birth control is to destroy the sperm within the vagina. Sperm can be destroyed with spermicidal jellies, suppositories, and foams applied immediately before intercourse. The failure rate varies widely, from 3% to 22%.
Sexually Transmitted Diseases
Sexually transmitted diseases (STDs) are diseases that spread from one person to another through sexual contact. AIDS, discussed in chapter 27, is a deadly viral STD. Other significant sexually transmitted diseases include:
Gonorrhea. The primary symptom of this disease, which is caused by the bacterium Neisseria gonorrhoeae, is discharge from the penis or vagina. It can be treated with antibiotics. If left untreated in women, gonorrhea can cause pelvic inflammatory disease (PID), a condition in which the fallopian tubes become scarred and blocked. PID can eventually lead to sterility.
Chlamydia. Caused by the bacterium Chlamydia trachomatis, this disease is sometimes called the “silent STD” because women usually experience no symptoms until after the infection has become established. Like gonorrhea, chlamydia can cause PID in women if left untreated.
Syphilis. Caused by the bacterium Treponema pallidum, this disease is one of the most potentially devastating STDs. Left untreated, the disease progresses to heart disease, mental deficiency, and nerve damage that may include loss of motor function or blindness.
Genital herpes. Caused by the herpes simplex virus type 2 (HSV-2), this disease is the most common STD in the United States. The virus causes red blisters on the penis or on the labia, vagina, or cervix that scab over. Cervical cancer. About 70% of cervical cancer is caused by HPV (human papillomavirus), a sexually transmitted virus. Gardasil, a newly developed vaccine that blocks HPV in women not yet exposed to the virus, could cut worldwide deaths (about 290,000 women each year) by two-thirds.
Key Learning Outcome 31.8. A variety of birth control methods are available, many of them quite effective. Sexually transmitted diseases are spread through sexual contact.
Inquiry & Analisys
Why Do STDs Vary in Frequency?
As a general rule, the incidence of a sexually transmitted disease is expected to increase with increasing frequencies of unprotected sexual contact. With the emergence of AIDS, intense publicity and education has lessened such dangerous behavior. Both the number of sexual partners and the frequency of unprotected sex have fallen significantly in the United States in the last decade. It would follow, then, that the frequencies of sexually transmitted diseases (STDs) like syphilis, gonorrhea, and chlamydia should also be falling.
However, the level of one STD sometimes rises while another falls. What are we to make of this? The simplest explanation of such a difference is that the two STDs are occurring in different populations, and one population has rising levels of sexual activity, while the other has falling levels. However, nationwide statistics encompass all population subgroups, and there is no reason to expect subgroups to contain different STDs. Certainly each major subgroup contains all three major STDs mentioned above. So this would seem an unlikely explanation for the frequency of one STD to be rising while another falls.
A second possible explanation would be a change in the infectivity of one of the STDs. A less-infective STD would tend to fall in frequency in the population, for the simple reason that fewer sexual contacts result in infection.
To assess this possibility, we must examine the individual STDs more closely.
Syphilis is most infective in its initial stage, but this stage lasts only about a month. Most transmissions occur during the much longer second stage, marked by a pink rash and sores in the mouth. The bacteria can be transmitted at this stage by kissing or shared liquids. Any drop in infectivity of this STD would be expected to shorten this stage—but no such shortening has been observed.
Gonorrhea can be transmitted by various forms of sexual contact with an infected individual at any time during the infection. There has been no drop in infectivity per sexual contact reported.
Chlamydia offers the most interesting possibility of changes in infectivity, because of its unusual nature. Chlamydia trachomatis is genetically a bacterium but is an obligate intracellular parasite, much like a virus in this respect—it can reproduce only inside human cells. The red structures in the photo are chlamydia bacteria inside human cells. Like gonorrhea, chlamydia is transmitted through vaginal, anal, or oral intercourse with an infected person. With chlamydia, the person may show no symptoms. Because the disease agent lives inside cells, its infectivity would not be expected to change unless the number of cells of an infected individual to which his or her sex partner would be exposed during intercourse were to change, a very unlikely possibility.
So a drop in infectivity doesn't seem very likely. There is, however, a third possible explanation for why the frequency of one STD in a population might rise while the frequency of another STD in that same population falls. To grasp this third possible explanation, we will need to examine carefully the trends in the incidence in the United States of the gonorrhea, chlamydia, and syphilis. Detailed yearly statistics are reported in the graph above.
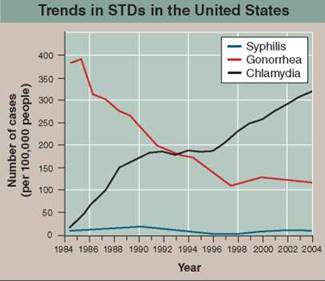
1. Applying Concepts. What is the dependent variable?
2. Making Inferences
a. Gonorrhea: What is the incidence in 1985? in 1995? Has the frequency declined or increased? In general, are individuals aware they are infected when they transmit the STD?
b. Chlamydia: What is the incidence in 1985? in 1995? Has the frequency declined or increased? In general, are individuals aware they are infected when they transmit the STD?
3. Drawing Conclusions. How might heightened public awareness explain why the trend in levels of gonorrhea differs from that of chlamydia?
1. If the offspring are not genetically identical to each other or the parent, then the organism reproduces through
a. fission.
b. sexual reproduction.
c. budding.
d. All of the above.
2. In mammals, the embryonic gonads will develop into ovaries
a. if the SRY gene is expressed.
b. if both sex chromosomes are X.
c. if the sex chromosomes are X and Y.
d. within the first 40 days.
3. Embryonic development in dogs is an example of
a. viviparity.
b. ovoviviparity.
c. oviparity.
d. parthenogenesis.
4. Temperature regulation of spermatogenesis in human males is controlled by the location of the
a. seminiferous tubules.
b. epididymis.
c. vas deferens.
d. scrotum.
5. Oocyte development in human females requires the hormones
a. estrogen and testosterone.
b. FSH and LH.
c. progesterone and testosterone.
d. oxytocin and prolactin.
6. When pregnancy occurs, the endometrium is maintained by the
a. embryo releasing hCG.
b. decrease in levels of progesterone.
c. hypothalamus releasing GnRH.
d. increasing levels of FSH.
7. A human embryo has formed the three germ layers from which all tissues form by the time
a. the blastula forms.
b. neurulation is complete.
c. the blastocyst forms.
d. gastrulation is complete.
8. In a developing human, the first tissues to begin forming are the
a. skeletal.
b. muscular.
c. neural.
d. digestive.
9. Contractions of the uterus during labor are stimulated by the hormone
a. estrogen.
b. prolactin.
c. oxytocin.
d. progesterone.
10. Which of the following is not a method of contraception?
a. destruction of the egg
b. prevention of egg maturation
c. sperm blockage
d. prevention of embryo implantation