MCAT Biology Review
Chapter 6: The Respiratory System
Introduction
Coughing. Fever. Shortness of breath. Hypoxia. All are symptoms of a number of pulmonary diseases, from a chronic obstructive pulmonary disease (COPD) flare to Streptococcus pneumoniae (pneumococcal) pneumonia to a type of hypersensitivity pneumonitis also known as extrinsic allergic alveolitis (EAA). This last example is a bit more esoteric, and can be brought on by hypersensitivity to anything from dried grass to rat urine to mold that grows in hot tubs—what is sometimes called hot tub lung. Not all cases of hot tub lung are severe, but certainly none are enjoyable. They’re often misdiagnosed as asthma or bronchitis, and may be treated with steroids, which quell the immune system and reduce the inflammation associated with this illness. Because hot tub lung can potentially go away by itself, antibiotic therapy is not always recommended. As a physician, you may end up simply having to tell your patients that the best way to avoid hot tub lung is to make sure that the tub is cleaned properly and routinely before use.
The lesson here isn’t to avoid hot tubs. It’s that the lungs are essential, sensitive organs with delicate membranes that must be protected. Many types of stressors (pathogens, particles, or chemicals) can irritate them and cause respiratory distress. In this chapter, we’ll look at the structure of the lungs and the microanatomy of respiration. We’ll also talk about the mechanics of breathing as well as the overall function of the lungs.
6.1 Anatomy and Mechanism of Breathing
The lungs are located in the thoracic cavity, the structure of which is specially designed to perform breathing.
ANATOMY
The anatomy of the respiratory system is summarized in Figure 6.1. Gas exchange occurs in the lungs. Air enters the respiratory tract through the external nares of the nose and then passes through the nasal cavity, where it is filtered through mucous membranes and nasal hairs (vibrissae).
KEY CONCEPT
The nose and mouth serve several important purposes in breathing by removing dirt and particulate matter from the air and warming and humidifying it before it reaches the lungs.
Next, air passes into the pharynx and the larynx. The pharynx resides behind the nasal cavity and at the back of the mouth; it is a common pathway for both air destined for the lungs and food destined for the esophagus. In contrast, the larynx lies below the pharynx and is only a pathway for air. To keep food out of the respiratory tract, the opening of the larynx (glottis) is covered by the epiglottis during swallowing. The larynx contains two vocal cords that are maneuvered using skeletal muscle and cartilage. From the larynx, air passes into the cartilaginous trachea and then into one of the two mainstem bronchi. The bronchi and trachea contain ciliated epithelial cells to catch material that has made it past the mucous membranes in the nose and mouth.
In the lungs, the bronchi continue to divide into smaller structures known as bronchioles, which divide further until they end in the tiny balloon-like structures in which gas exchange occurs (alveoli). Each alveolus is coated with surfactant, a detergent that lowers surface tension and prevents the alveolus from collapsing on itself. A network of capillaries surrounds each alveolus to carry oxygen and carbon dioxide. The branching and minute size of the alveoli allow for an exceptionally large surface area for gas exchange—approximately 100 m2.
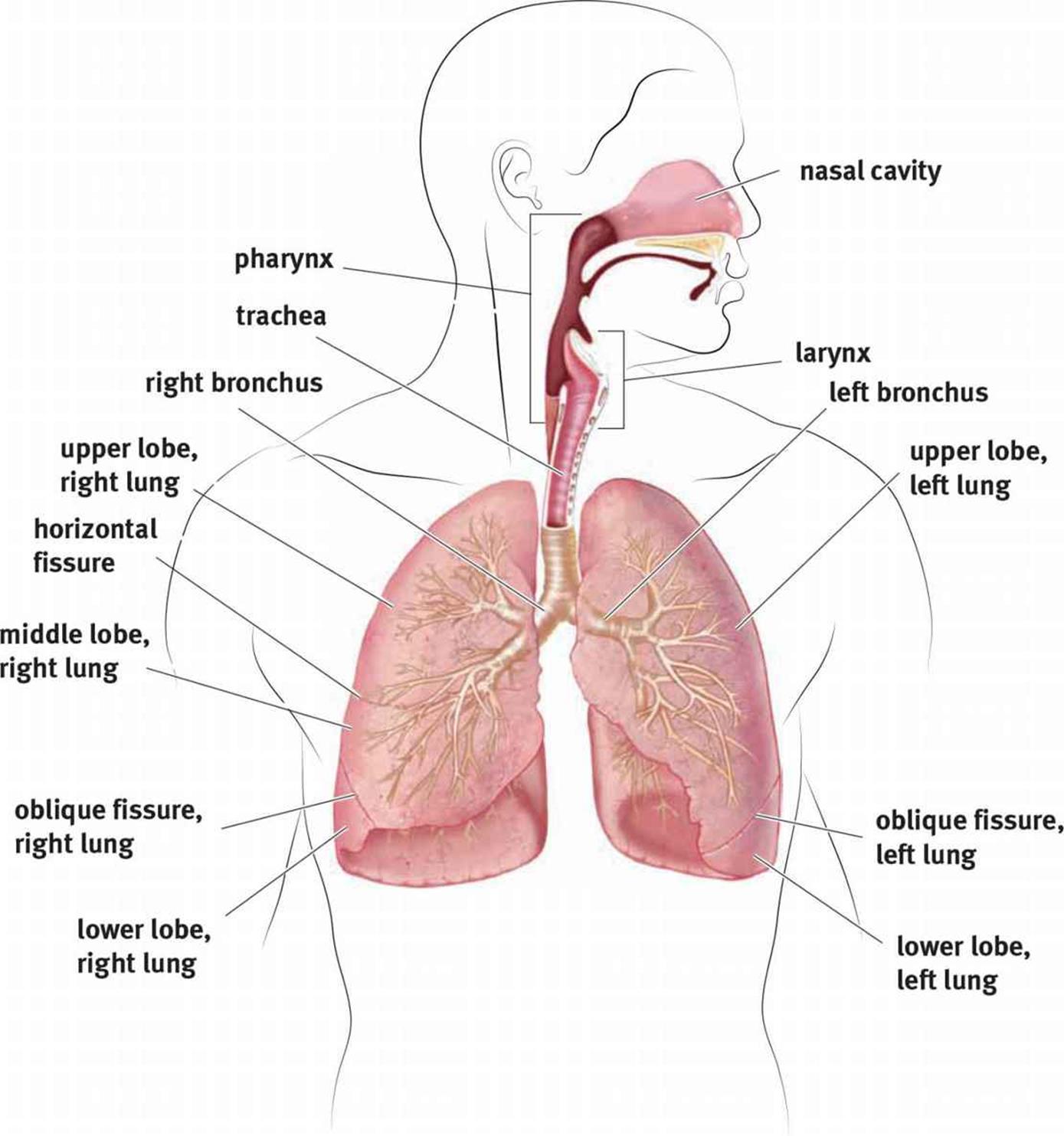 Figure 6.1. Anatomy of the Respiratory System
Figure 6.1. Anatomy of the Respiratory System
REAL WORLD
The left lung has a small indentation, making it slightly smaller than the right lung. It also contains only two lobes, while the right lung contains three. Why might this be? It is due to the position of the heart in the thoracic cavity.
The lungs themselves are contained in the thoracic cavity, which also contains the heart. The chest wall forms the outside of the thoracic cavity. Membranes known as pleurae surround each lung, as shown in Figure 6.2. The pleura forms a closed sac against which the lung expands. The surface adjacent to the lung is the visceral pleura, and the outer part is the parietal pleura.
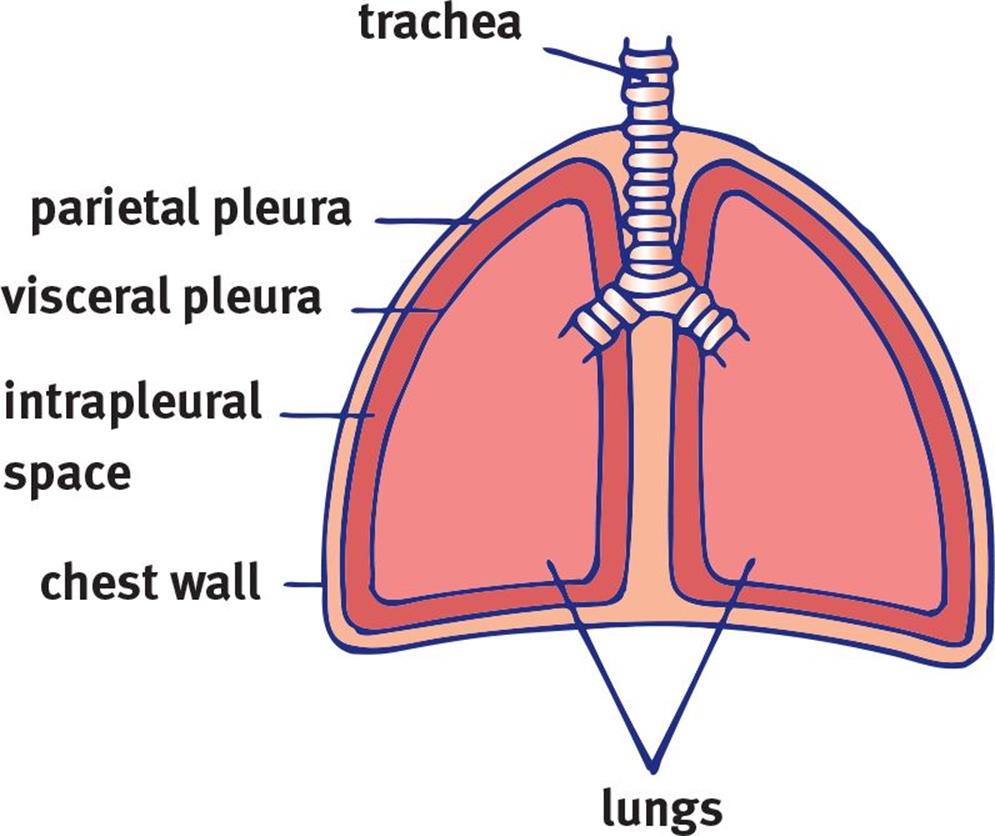 Figure 6.2. Lung Membranes
Figure 6.2. Lung Membranes
The lungs do not fill passively and require skeletal muscle to generate the negative pressure for expansion. The most important of these muscles is the diaphragm, a thin, muscular structure that divides the thoracic (chest) cavity from the abdominal cavity. The diaphragm is under somatic control, even though breathing itself is under autonomic control. In addition, muscles of the chest wall, abdomen, and neck may also participate in breathing, especially when breathing is labored due to a pathologic condition.
BREATHING
Before we discuss breathing itself, it is worth taking a closer look at the relationship between the pleura and the lungs. Imagine that you have a large, partially deflated balloon. Now, imagine taking your fist and pushing it against the balloon so that the balloon comes up and surrounds your hand. This is analogous to a lung and its pleura. Our fist is the lung, and the balloon represents both pleural layers. The side directly touching our fist is the visceral pleura, and the outer layer is the parietal pleura, which is associated with the chest wall in real life. The space within the sac is referred to as the intrapleural space, which contains a thin layer of fluid. This pleural fluid helps lubricate the two pleural surfaces. The pressure differentials that can be created across the pleura ultimately drive breathing, as we explore in the next section.
REAL WORLD
The intrapleural space is an example of a potential space—a space that is normally empty or collapsed. In some pathologic states, that potential space can be expanded by fluid or air that accumulates within the space. For example, in a pleural effusion, fluid accumulates in the intrapleural space. In a pneumothorax, air collects here. Each of these states disturbs the normal mechanics of the breathing apparatus and can cause atelectasis, or lung collapse.
Let’s turn to the mechanics of ventilation, which are grounded in physics. As discussed in Chapters 2 and 3 of MCAT Physics and Math Review, we can use pressure to do useful work in a system. Here, we use pressure differentials between the lungs and intrapleural space to drive air into the lungs.
Inhalation
Inhalation is an active process. We use our diaphragm as well as the external intercostal muscles (one of the layers of muscles between the ribs) to expand the thoracic cavity, as shown in Figure 6.3. As the diaphragm flattens and the chest wall expands outward, the intrathoracic volume(the volume of the chest cavity) increases. Specifically, because the intrapleural space most closely abuts the chest wall, its volume increases first. Can we predict what will happen to intrapleural pressure? From our understanding of Boyle’s law, an increase in intrapleural volume leads to a decrease in intrapleural pressure.
BRIDGE
Boyle’s law states that the pressure and volume of gases are inversely related. This is the principle underlying negative-pressure breathing: as the chest wall expands, the pressure in the lungs drops, and air is drawn into the lungs.
Now we have low pressure in the intrapleural space. What about inside the lungs? The gas in the lungs is initially at atmospheric pressure, which is now higher than the pressure in the intrapleural space. The lungs will therefore expand into the intrapleural space, and the pressure in the lungs will drop. Air will then be sucked in from a higher-pressure environment—the outside world. This mechanism is referred to as negative-pressure breathing because the driving force is the lower (relatively negative) pressure in the intrapleural space compared with the lungs.
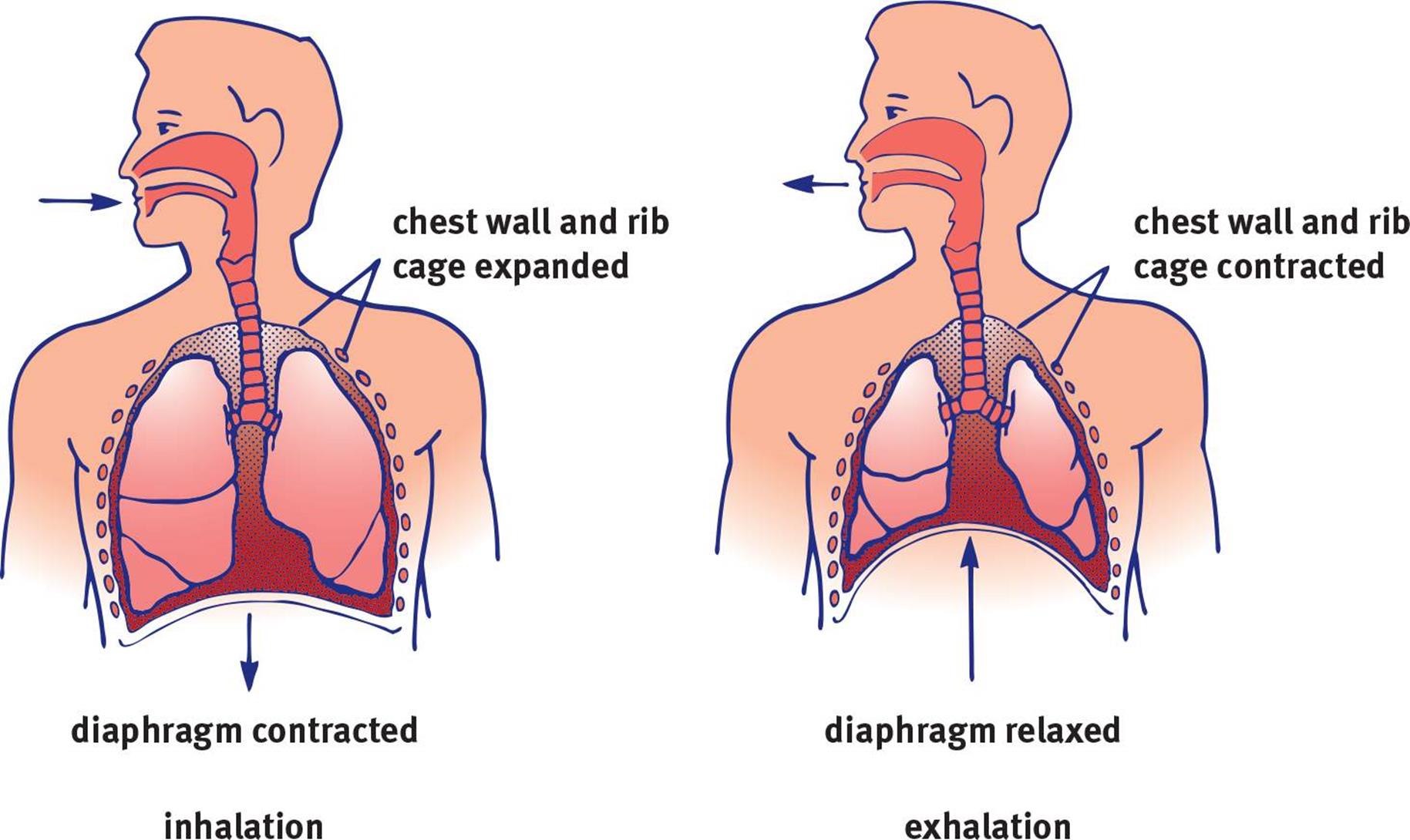 Figure 6.3. Stages of Ventilation The diaphragm contracts during inhalation and relaxes during exhalation.
Figure 6.3. Stages of Ventilation The diaphragm contracts during inhalation and relaxes during exhalation.
Exhalation
Unlike inhalation, exhalation does not have to be an active process. Simple relaxation of the external intercostal muscles will reverse the processes we discussed in the last paragraph. As the diaphragm and external intercostals relax, the chest cavity decreases in volume. What will happen to pressure in the intrapleural space? It will go up, again explained by Boyle’s law. Now pressure in the intrapleural space is higher than in the lungs, which is still at atmospheric pressure. Thus, air will be pushed out, resulting in exhalation. During active tasks, we can speed this process up by using the internal intercostal muscles and abdominal muscles, which oppose the external intercostals and pull the rib cage down. This actively decreases the volume of the thoracic cavity. Finally, recall that surfactant prevents the complete collapse of the alveoli during exhalation by reducing surface tension at the alveolar surface.
KEY CONCEPT
Inhalation and exhalation require different amounts of energy expenditure. Muscle contraction is required to create the negative pressure in the thoracic cavity that forces air into the lungs during inspiration. Expiration during calm states is entirely due to elastic recoil of the lungs and the musculature. During more active states, the muscles can be used to force air out and speed up the process of ventilation.
Remember the balloon analogy from before. The lungs have an elastic quality and are attached via the pleurae to the chest wall. The chest wall expands on inhalation, pulling the lungs with it and creating the pressure differential required for inhalation. As the chest wall relaxes, the lungs recoil and accentuate the relaxation process. When the lungs recoil, their volume becomes smaller, and the pressure increases. Now the pressure inside the lungs is higher than the outside pressure, and exhalation occurs. Note that the indirect connection of the lungs to the chest wall also prevents them from collapsing completely on recoil, like surfactant.
REAL WORLD
Emphysema is a disease characterized by the destruction of the alveolar walls. This results in reduced elastic recoil of the lungs, making the process of exhalation extremely difficult. Most cases of emphysema are caused by cigarette smoking.
LUNG CAPACITIES AND VOLUMES
In pulmonology (the medical field associated with the lungs and breathing), we frequently must assess lung capacities and volumes—but we don’t have the luxury of removing an individual’s lungs to do so. One instrument used to measure these quantities is a spirometer. While a spirometer cannot measure the amount of air remaining in the lung after complete exhalation (residual volume), it provides a number of measures that are useful in clinical medicine.
Commonly tested lung volumes include:
· Total lung capacity (TLC): The maximum volume of air in the lungs when one inhales completely; usually around 6 to 7 liters
· Residual volume (RV): The minimum volume of air in the lungs when one exhales completely
· Vital capacity (VC): The difference between the minimum and maximum volume of air in the lungs (TLC – RV)
· Tidal volume (TV): The volume of air inhaled or exhaled in a normal breath
· Expiratory reserve volume (ERV): The volume of additional air that can be forcibly exhaled after a normal exhalation
· Inspiratory reserve volume (IRV): The volume of additional air that can be forcibly inhaled after a normal inhalation
These different lung volumes and capacities can be seen in Figure 6.4.
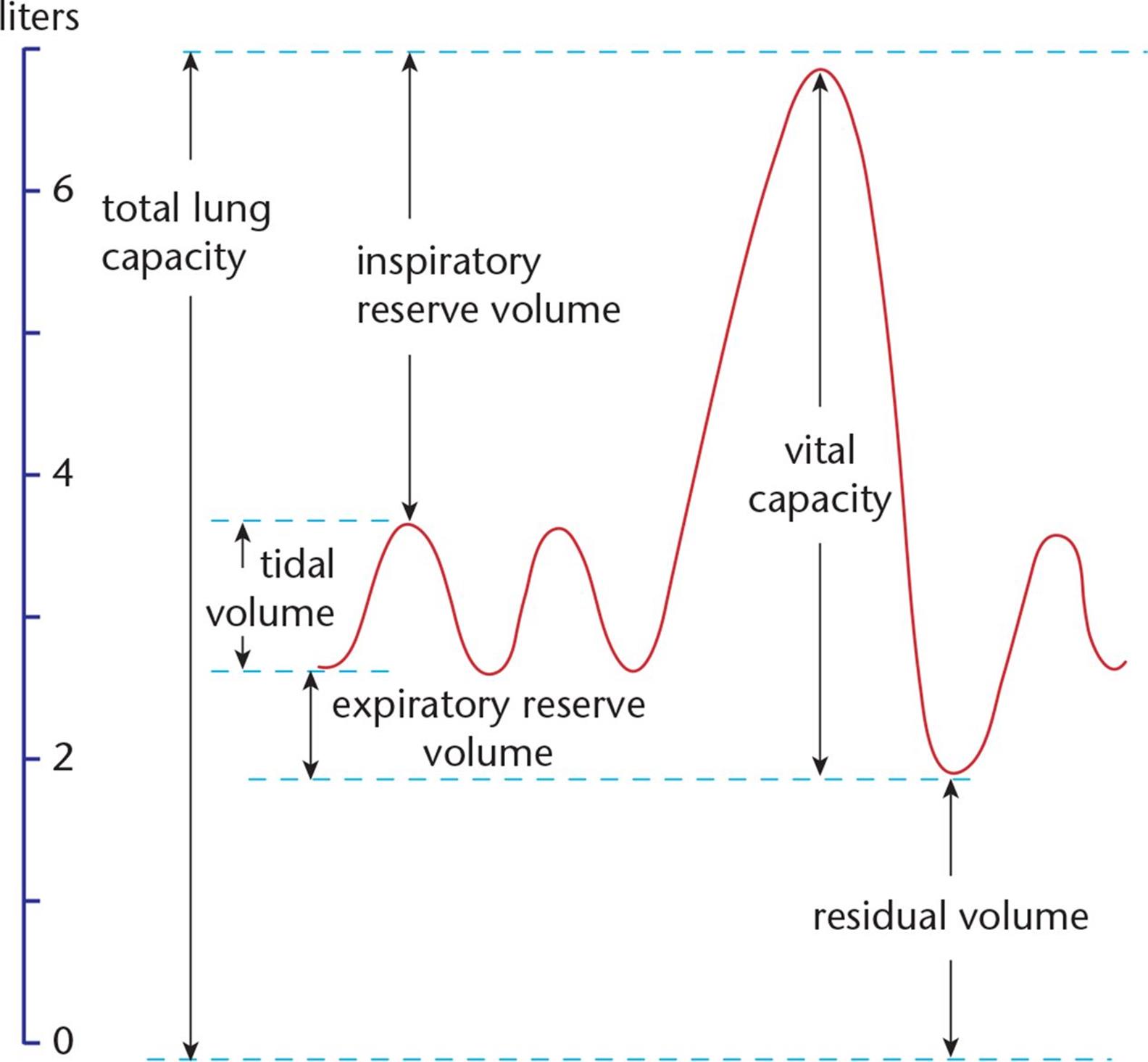 Figure 6.4. Lung Volumes
Figure 6.4. Lung Volumes
REGULATION OF BREATHING
Breathing requires input from our nervous control center. Ventilation is primarily regulated by a collection of neurons in the medulla oblongata called the ventilation center that fire rhythmically to cause regular contraction of respiratory muscles. These neurons contain chemoreceptors that are primarily sensitive to carbon dioxide concentration. As the partial pressure of carbon dioxide in the blood rises (hypercarbia or hypercapnia), the respiratory rate will increase so that more carbon dioxide is exhaled, and carbon dioxide levels in the blood will fall. These cells also respond to changes in oxygen concentration, although this tends to have significance only during periods of significant hypoxia (low oxygen concentration in the blood).
We can, to a limited extent, control our breathing through the cerebrum. We can choose to breathe more rapidly or slowly; however, extended periods of hypoventilation would lead to increased carbon dioxide levels and an override by the medulla oblongata (which would jump-start breathing). The opposite process (hyperventilation) would blow off too much carbon dioxide and ultimately inhibit ventilation.
MCAT Concept Check 6.1:
Before you move on, assess your understanding of the material with these questions.
1. List the structures in the respiratory pathway, from where air enters the nares to the alveoli.
2. Which muscle(s) are involved in inhalation? Exhalation?
· Inhalation:
· Exhalation:
3. What is the purpose of surfactant?
4. What is the mathematical relationship between vital capacity (VC), inspiratory reserve volume (IRV), expiratory reserve volume (ERV), and tidal volume (TV)?
5. If blood levels of CO2 become too low, how does the brain alter the respiratory rate to maintain homeostasis?