MCAT Biology Review
Chapter 9: The Digestive System
9.2 Ingestion and Digestion
To supply the body with nutrients, we must ingest (eat) food. Several hormones are involved with feeding behavior, including antidiuretic hormone (ADH or vasopressin), aldosterone, glucagon, ghrelin, leptin, and cholecystokinin. ADH and aldosterone trigger the sensation of thirst, encouraging the behavior of fluid consumption. Glucagon, secreted by the pancreas, and ghrelin, secreted by the stomach and pancreas, stimulate feelings of hunger. Leptin and cholecystokinin do the opposite, stimulating feelings of satiety. Digestion begins in the oral cavity and continues in the stomach and the first part of the small intestine, known as the duodenum.
ORAL CAVITY
The oral cavity plays a role in both mechanical and chemical digestion of food. Mechanical digestion in the mouth involves the breaking up of large food particles into smaller particles by using the teeth, tongue, and lips. This process is called mastication (chewing). Chewing helps to increase the surface-area-to-volume ratio of the food, allowing for more surface area for enzymatic digestion as it passes through the gut tube. It also moderates the size of food particles entering the lumen of the alimentary canal; food particles that are too large create an obstructive risk in the tract.
KEY CONCEPT
The chemical digestion of carbohydrates is initiated in the mouth, but is completed in the small intestine. Salivary amylase (active in the mouth) and pancreatic amylase (active in the small intestine) have the same function.
Chemical digestion begins the breakdown of chemical bonds in the macromolecules that make up food. This relies on enzymes from saliva produced by the three pairs of salivary glands. Saliva also aids mechanical digestion by moistening and lubricating food. The salivary glands, like all glands of the digestive tract, are innervated by the parasympathetic nervous system. The presence of food in the oral cavity triggers a neural circuit that ultimately leads to increased parasympathetic stimulation of these glands. Salivation can also be triggered by signals that food is near, such as smell or sight. Saliva contains salivary amylase, also known as ptyalin, and lipase. Salivary amylase is capable of hydrolyzing starch into smaller sugars (maltose and dextrins), while lipase catalyzes the hydrolysis of lipids. The amount of chemical digestion that occurs in the mouth is minimal, though, because the food does not stay in the mouth for long. Our muscular tongue forms the food into a bolus, which is forced back to the pharynx and swallowed.
REAL WORLD
There are three pairs of major salivary glands, called the parotid, submandibular, and sublingual glands. Other microscopic salivary glands are scattered throughout the upper digestive system. While the parasympathetic nervous system is responsible for promoting salivation, the sympathetic nervous system has some input into the glands as well. The sympathetic nervous system increases the viscosity of saliva, which is why dry mouth and even a tacky sensation in the mouth occurs during a fight-or-flight response.
PHARYNX
The pharynx is the cavity that leads from the mouth and posterior nasal cavity to the esophagus. The pharynx connects not only to the esophagus, but also to the larynx, which is a part of the respiratory tract. The pharynx can be divided into three parts: the nasopharynx (behind the nasal cavity), the oropharynx (at the back of the mouth), and the laryngopharynx (above the vocal cords). Food is prevented from entering the larynx during swallowing by the epiglottis, a cartilaginous structure that folds down to cover the laryngeal inlet. Failure of this mechanism can lead to aspiration of food and choking.
ESOPHAGUS
The esophagus is a muscular tube that connects the pharynx to the stomach. The top third of the esophagus is composed of skeletal muscle, the bottom third is composed of smooth muscle, and the middle third is a mix of both. What does this mean in terms of nervous control? While the top of the esophagus is under somatic (voluntary) motor control, the bottom—and most of the rest of the gastrointestinal tract, for that matter—is under autonomic (involuntary) nervous control. The rhythmic contraction of smooth muscle that propels food toward the stomach is calledperistalsis. Under normal circumstances, peristalsis proceeds down the digestive tract. However, certain conditions, such as exposure to chemicals, infectious agents, physical stimulation in the posterior pharynx, and even cognitive stimulation, can lead to reversal of peristalsis in the process of emesis (vomiting).
Swallowing is initiated in the muscles of the oropharynx, which constitute the upper esophageal sphincter. Peristalsis squeezes, pushes, and propels the bolus toward the stomach. As the bolus approaches the stomach, a muscular ring known as the lower esophageal sphincter (cardiac sphincter) relaxes and opens to allow the passage of food.
REAL WORLD
Weakness in the lower esophageal sphincter is a key feature of gastroesophageal reflux disease (GERD), which causes classic heartburn symptoms after eating. As food and acid reflux into the lower esophagus, they irritate the less-protected mucosa, stimulating pain receptors. These receptors localize pain poorly, so a general burning sensation is felt in the lower chest—leading to the common term heartburn.
STOMACH
There are three main energy sources: carbohydrates, fats, and proteins. As mentioned earlier, the chemical digestion of carbohydrates and fats is initiated in the mouth. No mechanical or chemical digestion takes place in the esophagus, except for the continued enzymatic activity initiated in the mouth by salivary enzymes. Thus, digestion that occurs prior to the entrance of the bolus into the stomach is minimal compared to the digestion that occurs in the stomach and small intestine.
The stomach is a highly muscular organ with a capacity of approximately two liters. In humans, the stomach is located in the upper left quadrant of the abdominal cavity, under the diaphragm. This organ uses hydrochloric acid and enzymes to digest food, creating a fairly harsh environment, and its mucosa is quite thick to prevent autodigestion. The stomach can be divided into four main anatomical divisions, as shown in Figure 9.2: the fundus and body, which contain mostly gastric glands, and the antrum and pylorus, which contain mostly pyloric glands. The internal curvature of the stomach is called the lesser curvature; the external curvature is called the greater curvature. The lining of the stomach is thrown into folds called rugae.
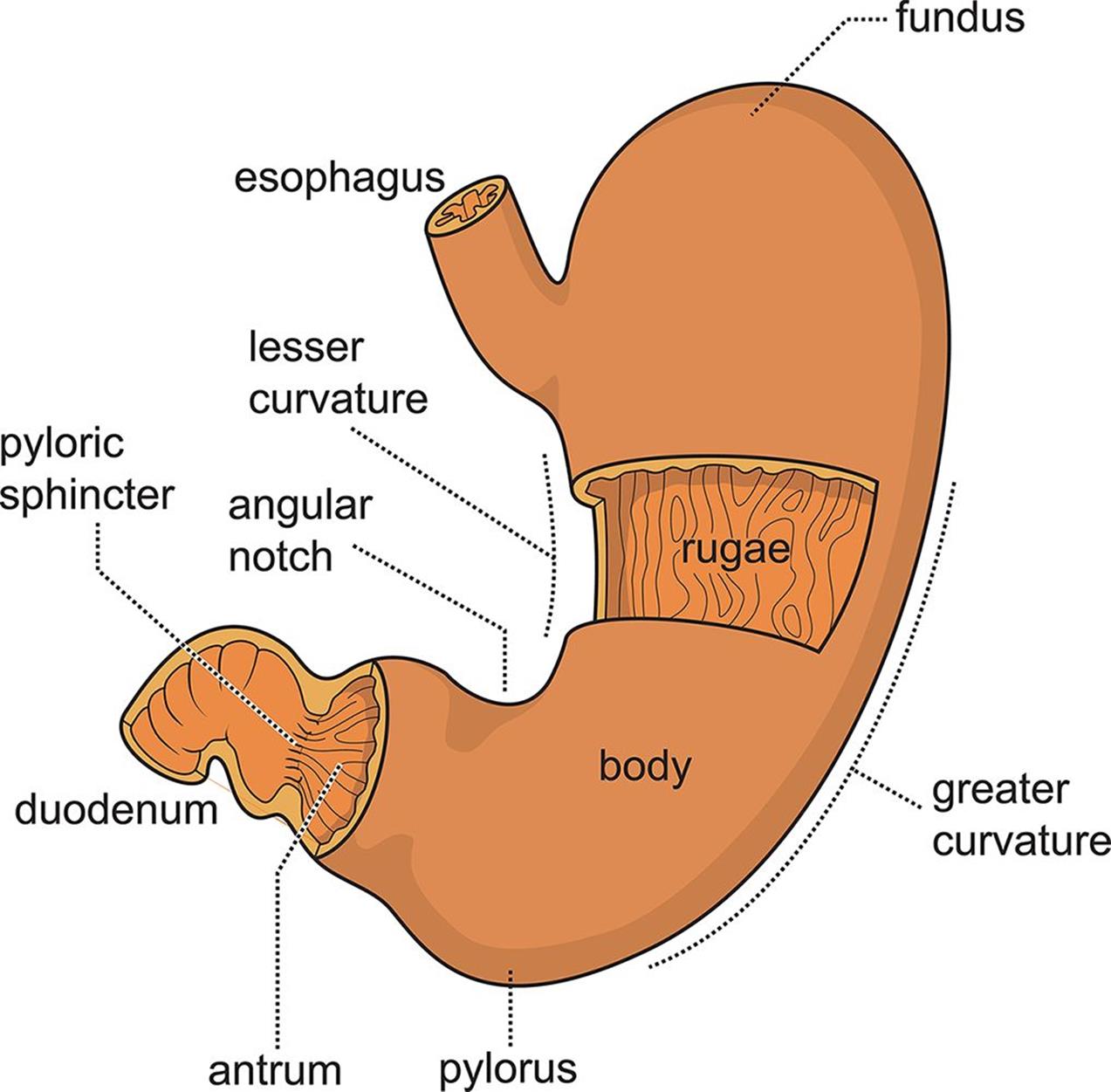 Figure 9.2. Anatomy of the Stomach
Figure 9.2. Anatomy of the Stomach
The mucosa of the stomach contains gastric glands and pyloric glands. The gastric glands respond to signals from the vagus nerve of the parasympathetic nervous system, which is activated by the brain in response to the sight, taste, and smell of food. Gastric glands have three different cell types: mucous cells, chief cells, and parietal cells. Mucous cells produce the bicarbonate-rich mucus that protects the muscular wall from the harshly acidic (pH = 2) and proteolytic environment of the stomach.
REAL WORLD
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen, and aspirin, are very common drugs. However, these drugs are not without side effects. One such side effect is the disruption of mucus production within the stomach. This leaves the mucosa of the stomach unprotected, and irritation results. This irritation can be in the form of gastritis, inflammation of the mucosa of the stomach, or gastric ulcers, deep wounds in the surface of the stomach.
Gastric juice is a combination of secretions from the other two cell types in the gastric glands. The chief cells secrete pepsinogen. This is the inactive, zymogen form of pepsin, a proteolytic enzyme. Hydrogen ions in the stomach, secreted by parietal cells as hydrochloric acid, cleave pepsinogen to pepsin. Pepsin digests proteins by cleaving peptide bonds near aromatic amino acids, resulting in short peptide fragments. Because pepsin is activated by the acidic environment, it follows that pepsin is most active at a low pH. This is a unique characteristic among human enzymes, as most human enzymes are most active at physiological pH. Stomach acid also kills most harmful bacteria (with the exception of Helicobacter pylori, infection with which is usually asymptomatic but can cause inflammation, ulcers, and even certain gastric cancers). The acidic environment also helps to denature proteins and can break down some intramolecular bonds that hold food together. In addition to HCl, parietal cells secrete intrinsic factor, a glycoprotein involved in the proper absorption of vitamin B12.
KEY CONCEPT
The stomach secretes six products:
1. HCl (kills microbes, denatures proteins, and converts pepsinogen into pepsin)
2. Pepsinogen (cleaved to pepsin in the stomach; an enzyme that partially digests proteins)
3. Mucus (protects mucosa)
4. Bicarbonate (protects mucosa)
5. Water (dissolves and dilutes ingested material)
6. Intrinsic factor (required for normal absorption of vitamin B12)
The pyloric glands contain G cells that secrete gastrin, a peptide hormone. Gastrin induces the parietal cells in the stomach to secrete more HCl and signals the stomach to contract, mixing its contents. The digestion of solid food in the stomach results in an acidic, semifluid mixture known as chyme. The combined mechanical and chemical digestive activities of the stomach result in a significant increase in the surface area of the now unrecognizable food particles, so when the chyme reaches the intestines, the absorption of nutrients from it can be maximized. There are a few substances that are absorbed directly from the stomach (such as alcohol and aspirin), but the stomach is mainly an organ of digestion.
REAL WORLD
Zollinger–Ellison syndrome is a rare disease resulting from a gastrin-secreting tumor (gastrinoma). Typically, this tumor is found in the pancreas. The excess gastrin leads to excessive HCl production by parietal cells. Not surprisingly, one of the most common signs of Zollinger–Ellison syndrome is the presence of intractable ulcer disease.
DUODENUM
The small intestine consists of three segments: the duodenum, the jejunum, and the ileum. The small intestine is quite long, up to seven meters. The duodenum is responsible for the majority of chemical digestion and has some minor involvement in absorption. However, most of the absorption in the small intestine takes place in the jejunum and ileum.
Food leaves the stomach through the pyloric sphincter and enters the duodenum. The presence of chyme in the duodenum causes the release of brush-border enzymes like disaccharidases (maltase, isomaltase, lactase, and sucrase) and peptidases (including dipeptidase). Brush-border enzymes are present on the luminal surface of cells lining the duodenum and break down dimers and trimers of biomolecules into absorbable monomers. The duodenum also secretes enteropeptidase, which is involved in the activation of other digestive enzymes from the accessory organs of digestion. Finally, it secretes hormones like secretin and cholecystokinin (CCK) into the bloodstream.
The disaccharidases digest disaccharides. Maltase digests maltose, isomaltase digests isomaltose, lactase digests lactose, and sucrase digests sucrose. Lack of a particular disaccharidase causes an inability to break down the corresponding disaccharide. Then bacteria in the intestines are able to hydrolyze that disaccharide, producing methane gas as a byproduct. In addition, undigested disaccharides can have an osmotic effect, pulling water into the stool and causing diarrhea. This is why people who are lactose intolerant have symptoms of bloating, flatulence, and possibly diarrhea after ingesting dairy products.
Peptidases break down proteins (or peptides, as the name implies). Aminopeptidase is a peptidase secreted by glands in the duodenum that removes the N-terminal amino acid from a peptide. Dipeptidases cleave the peptide bonds of dipeptides to release free amino acids. Unlike carbohydrates, which must be broken down into monosaccharides for absorption, di- and even tripeptides can be absorbed across the small intestine wall.
Enteropeptidase (formerly called enterokinase) is an enzyme critical for the activation of trypsinogen, a pancreatic protease, to trypsin. Trypsin then initiates an activation cascade, as described later in this chapter. Enteropeptidase can also activate procarboxypeptidases A and B to their active forms.
REAL WORLD
Celiac disease results from an immune reaction against gluten, a protein found in grains, especially wheat. In this condition, the immune system develops antibodies against certain components of gluten. These antibodies then cross-react with elements of the small intestine, causing damage to the mucosa. This results in diarrhea and discomfort. Sometimes, this condition also results in malabsorptive syndromes, including the inability to absorb fat and fat-soluble vitamins. Contrary to popular belief, celiac disease and gluten sensitivity are immune responses, but not true allergies.
Secretin is a peptide hormone that causes pancreatic enzymes to be released into the duodenum. It also regulates the pH of the digestive tract by reducing HCl secretion from parietal cells and increasing bicarbonate secretion from the pancreas. Secretin is also an enterogastrone, a hormone that slows motility through the digestive tract. Slowing of motility allows increased time for digestive enzymes to act on chyme—especially fats.
Finally, cholecystokinin (CCK) is secreted in response to the entry of chyme (specifically, amino acids and fat in the chyme) into the duodenum. This peptide hormone stimulates the release of both bile and pancreatic juices and also acts in the brain, where it promotes satiety. Bile is a complex fluid composed of bile salts, pigments, and cholesterol. Bile salts are derived from cholesterol. They are not enzymes and therefore do not directly perform chemical digestion (the enzymatic cleavage of chemical bonds). However, bile salts serve an important role in the mechanical digestion of fats and ultimately facilitate the chemical digestion of lipids. Bile salts have hydrophobic and hydrophilic regions, allowing them to serve as a bridge between aqueous and lipid environments. In fact, bile salts are much like the common soaps and detergents we use to wash our hands, clothes, and dishes. In the small intestine, bile salts emulsify fats and cholesterol into micelles. Without bile, fats would spontaneously separate out of the aqueous mixture in the duodenum and would not be accessible to pancreatic lipase, which is water-soluble. In addition, these micelles increase the surface area of the fats, increasing the rate at which lipase can act. Ultimately, proper fat digestion depends on both bile and lipase. Bile gets the fats into the solution and increases their surface area by placing them in micelles (mechanical digestion). Then, lipase can come in to hydrolyze the ester bonds holding the lipids together (chemical digestion).
CCK also promotes the secretion of pancreatic juices into the duodenum, as shown in Figure 9.3. Pancreatic juices are a complex mixture of several enzymes in a bicarbonate-rich alkaline solution. This bicarbonate helps to neutralize acidic chyme, as well as provide an ideal working environment for each of the digestive enzymes, which are most active around pH 8.5. Pancreatic juices contain enzymes that can digest all three types of nutrients: carbohydrates, fats, and proteins. The identities and functions of these enzymes will be discussed in the next section of this chapter.
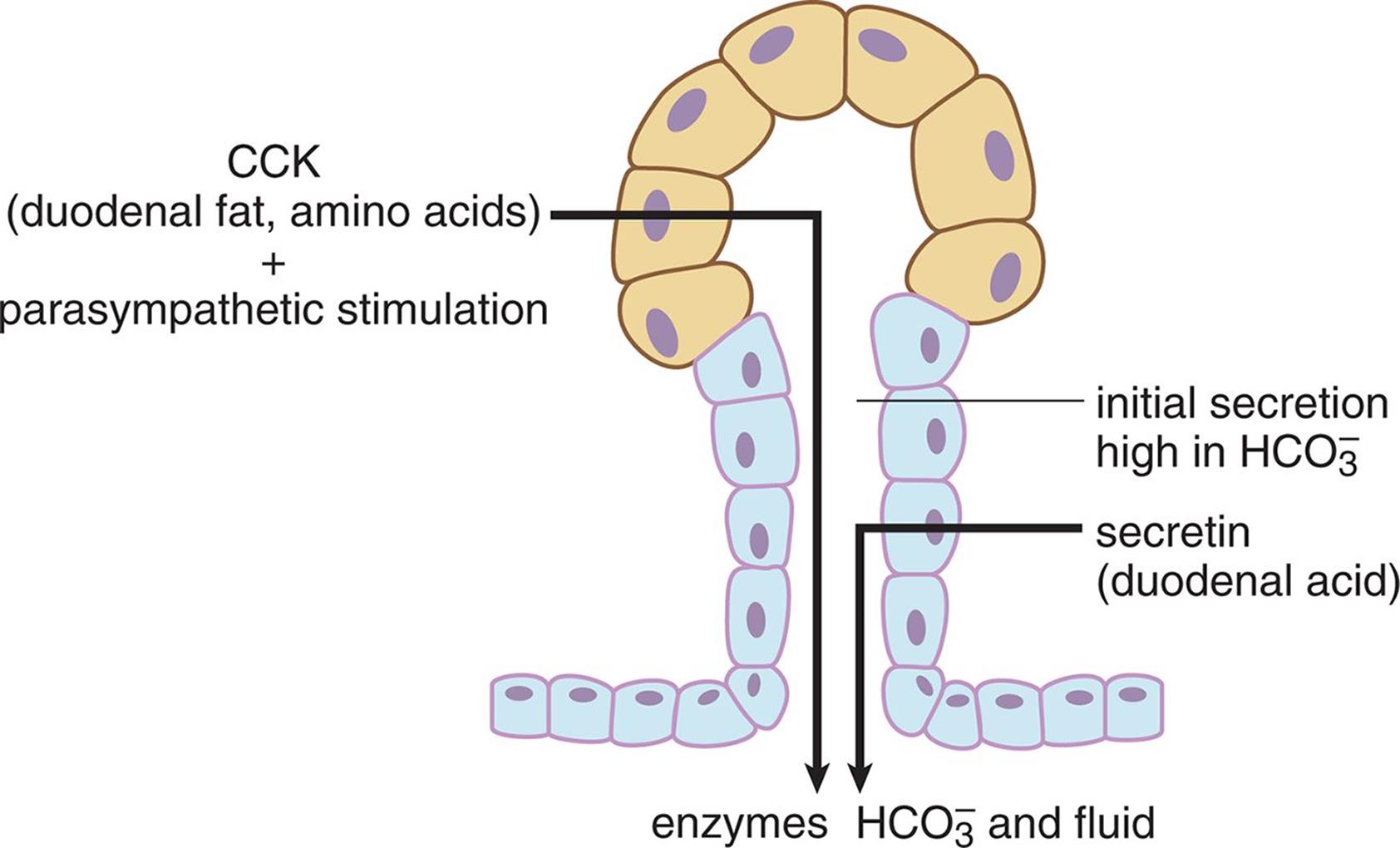 Figure 9.3. Hormonal Control of the Exocrine Pancreas
Figure 9.3. Hormonal Control of the Exocrine Pancreas
BRIDGE
The acidic environment of the stomach and basic environment of the duodenum point out the important correlation between pH and enzyme activity. Pepsin is active in the stomach and works best at pH 2. Pancreatic enzymes are active in the duodenum and work best at pH 8.5. pH, temperature, and salinity can all affect enzyme function, as highlighted in Chapter 2 of MCAT Biochemistry Review.
MCAT Concept Check 9.2:
Before you move on, assess your understanding of the material with these questions.
1. What two main enzymes are found in saliva? What do these enzymes do?
·
·
2. For each of the cell types below, list the major secretions of the cell and the functions of these secretions.
|
Cell |
Secretions |
Functions |
|
Mucous cell |
||
|
Chief cell |
||
|
Parietal cell |
||
|
G cell |
3. For each of the following substances, determine whether it is a digestive enzyme or a hormone and briefly summarize its functions.
|
Substance |
Enzyme or Hormone? |
Functions |
|
Sucrase |
||
|
Secretin |
||
|
Dipeptidase |
||
|
Cholecystokinin |
||
|
Enteropeptidase |
4. How do bile and pancreatic lipase work together to digest fats?