MCAT Biology Review
Chapter 9: The Digestive System
Practice Questions
1. Which of the following associations correctly matches a gastric cell with a compound it secretes?
1. G cells—HCl
2. Chief cells—pepsinogen
3. Parietal cells—alkaline mucus
4. Mucous cells—intrinsic factor
2. Which of the following is NOT part of the small intestine?
1. Ileum
2. Cecum
3. Jejunum
4. Duodenum
3. In an experiment, enteropeptidase secretion was blocked. As a direct result, levels of all of the following active enzymes would likely be affected EXCEPT:
1. trypsin.
2. aminopeptidase.
3. chymotrypsin.
4. carboxypeptidase A.
4. Which of the following INCORRECTLY pairs a digestive hormone with its function?
1. Trypsin—hydrolyzes specific peptide bonds
2. Lactase—hydrolyzes lactose to glucose and galactose
3. Pancreatic amylase—hydrolyzes starch to maltose
4. Lipase—emulsifies fats
5. Which of the following correctly lists two organs in which proteins are digested?
1. Mouth and stomach
2. Stomach and large intestine
3. Stomach and small intestine
4. Small intestine and large intestine
6. Which of the following choices INCORRECTLY pairs a digestive enzyme with its site of secretion?
1. Sucrase—salivary glands
2. Carboxypeptidase—pancreas
3. Trypsin—pancreas
4. Lactase—duodenum
7. A two-week-old male infant is brought to the emergency room. His mother reports that he has been unable to keep any milk down; shortly after he nurses, he has sudden projectile vomiting. During exam, an olive-shaped mass can be felt in his upper abdomen. It is determined that there is a constriction in the digestive system that prevents food from reaching the small intestine from the stomach. Which structure is most likely the site of the problem?
1. Cardiac sphincter
2. Pyloric sphincter
3. Ileocecal valve
4. Internal anal sphincter
8. Many medications have anticholinergic side effects, which block the activity of parasympathetic neurons throughout the body. Older individuals may be on many such medications simultaneously, exacerbating the side effects. Which of the following would NOT be expected in an individual taking medications with anticholinergic activity?
1. Dry mouth
2. Diarrhea
3. Slow gastric emptying
4. Decreased gastric acid production
9. The two graphs below show the relative activities of two enzymes in solutions of varying pH. Which of the following choices correctly identifies the two enzymes?
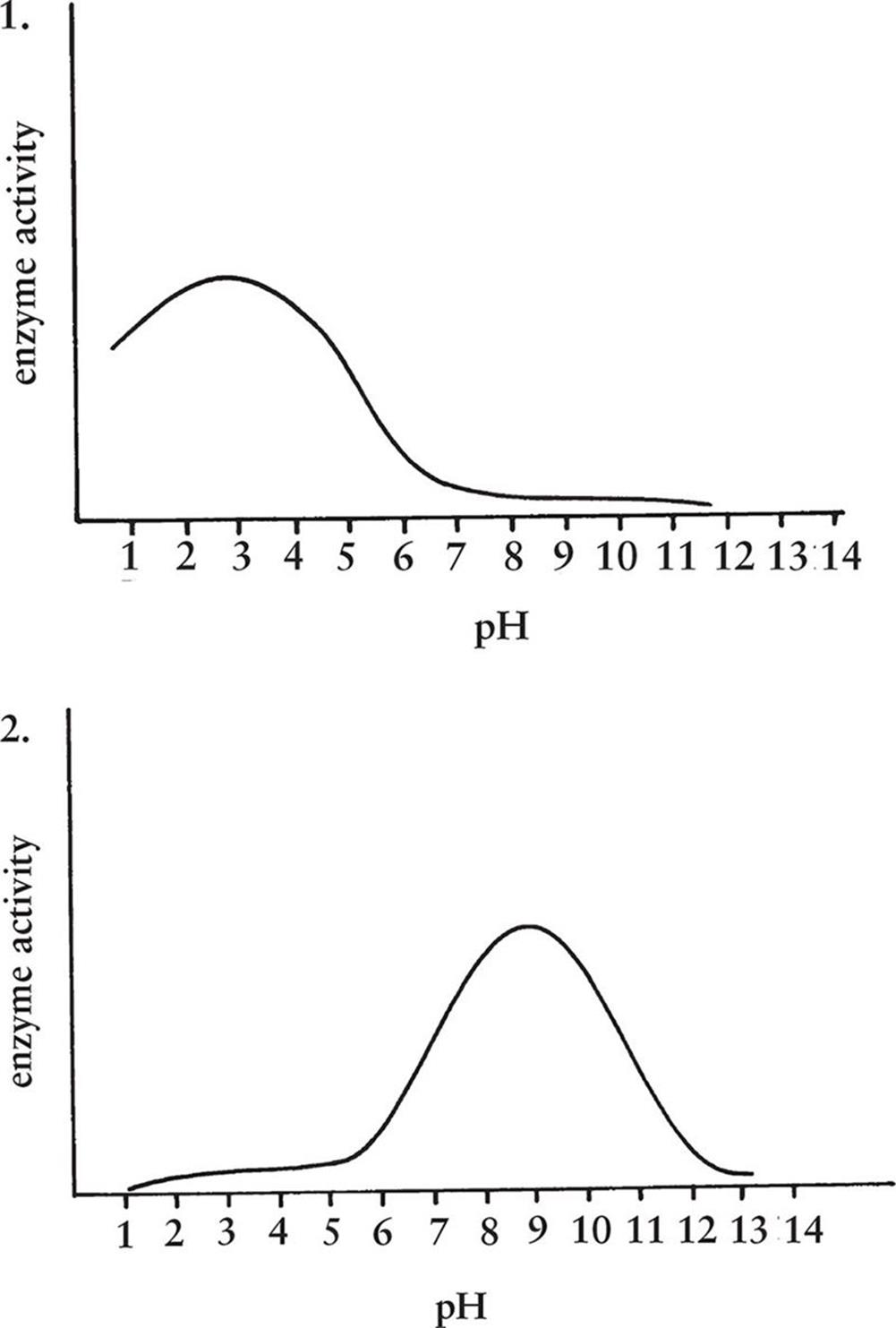
1. 1—chymotrypsin; 2—pepsin
2. 1—pepsin; 2—carboxypeptidase B
3. 1—lactase; 2—aminopeptidase
4. 1—enteropeptidase; 2—amylase
10.Which of the following would NOT likely lead to elevated levels of bilirubin in the blood?
1. Cholangiocarcinoma, a cancer of the bile ducts that can ultimately lead to full occlusion of the duct lumen
2. Autoimmune hemolytic anemia, a disease in which the red blood cells are attacked by antibodies and are lysed
3. Ménétrier’s disease, in which rugae thicken and overlying glands lose secretory ability
4. Acetaminophen (Tylenol) overdose, in which the accumulation of toxic metabolites can cause rapid liver failure
11.Which of the following correctly pairs the molecule with its primary site of absorption?
1. Chylomicrons—lacteals
2. Amino acids—large intestine
3. Vitamins A and E—stomach
4. Cholesterol—ascending colon
12.Starch is hydrolyzed into maltose by enzymes from the:
1. salivary glands.
2. brush border.
3. pancreas.
1. I only
2. I and III only
3. II and III only
4. I, II, and III
13.Which of the following biomolecules does NOT drain to the liver before arriving at the right side of the heart?
1. Cholecalciferol (Vitamin D)
2. Threonine (an amino acid)
3. Fructose (a monosaccharide)
4. Pantothenic acid (vitamin B5)
14.Which of the following hormones increases feeding behavior?
1. Leptin
2. Cholecystokinin
3. Ghrelin
4. Gastrin
15.Which of the following is likely to be seen in a patient with liver failure?
1. High concentrations of urea in the blood
2. High concentrations of albumin in the blood
3. Low concentrations of ammonia in the blood
4. Low concentrations of clotting factors in the blood
PRACTICE QUESTIONS
Answers and Explanations
1. BChief cells secrete pepsinogen, a protease secreted as a zymogen that is activated by the acidic environment of the stomach. G cells secrete gastrin, parietal cells secrete hydrochloric acid and intrinsic factor, and mucous cells secrete alkaline mucus, eliminating the other answer choices.
2. BThe small intestine is divided into three sections: the duodenum, the jejunum, and the ileum. The cecum is part of the large intestine, making choice (B) the correct answer.
3. BAminopeptidase is a brush-border peptidase secreted by the cells lining the duodenum; it does not require enteropeptidase for activation. Both trypsinogen and procarboxypeptidases A and B are activated by enteropeptidase, eliminating choices (A) and (D). Once activated, trypsin can activate chymotrypsinogen; if trypsinogen cannot be activated, then chymotrypsinogen will not be activated either, eliminating choice (C).
4. DLipase is involved in the digestion of fats, but its function is not to emulsify fats—this is the job of bile. Rather, lipase chemically digests fats in the duodenum, allowing them to be brought into duodenal cells and packaged into chylomicrons. The other associations given here are all correct.
5. CProtein digestion begins in the stomach, where pepsin (secreted as pepsinogen) hydrolyzes specific peptide bonds. Protein digestion continues in the small intestine as trypsin (secreted as trypsinogen), chymotrypsin (secreted as chymotrypsinogen), carboxypeptidases (secreted as procarboxypeptidases), aminopeptidase, and dipeptidases hydrolyze specific parts of the peptide. No protein digestion occurs in the mouth or large intestine.
6. ASucrase is a brush-border enzyme found on duodenal cells and is not secreted by the salivary glands. This enzyme hydrolyzes sucrose (a disaccharide) to form glucose and fructose (monosaccharides). The other associations are all correct.
7. BThe question is basically asking us to identify the structure that lies between the stomach and the small intestine. This is the pyloric sphincter; the presentation given in the question is a classic example of what is called pyloric stenosis, in which the pyloric sphincter is thickened and cannot relax to permit chyme through. The cardiac sphincter, choice (A), lies between the esophagus and the stomach. The ileocecal valve, choice (C), lies between the ileum of the small intestine and the cecum of the large intestine. The internal anal sphincter, choice (D), lies at the end of the rectum.
8. BThe parasympathetic nervous system has many roles in the digestive system. It promotes motility of the gut tube and secretion from glands. Therefore, blocking the parasympathetic nervous system would likely result in dry mouth (from reduced secretion of saliva), slow gastric emptying (from decreased peristalsis), and decreased gastric acid production (from reduced HCl secretion from the parietal cells in the gastric glands), eliminating choices (A), (C), and (D). Choice (B) is the correct answer because we would be more likely to expect constipation in such an individual, not diarrhea: slowed motility through the colon would lead to increased water reabsorption, making the feces too firm and causing constipation.
9. BThe first graph shows maximal activity at a very acidic pH, implying that this is an enzyme acting in the stomach. The second graph shows maximal activity around pH 8.5, implying that this is an enzyme acting in the duodenum. The only choice that matches the first graph with a stomach enzyme (pepsin) and the second with a duodenal enzyme (carboxypeptidase B) is choice (B).
10.CElevated bilirubin implies a blockage to bile flow, increased production of bilirubin (from massive hemoglobin release), or an inability of the liver to produce bile. If the bile duct were occluded, as in choice (A), then bile would not be able to flow into the digestive tract and would build up, increasing bilirubin levels in the blood. If many red blood cells were lysed, as in choice (B), then bilirubin levels would rise in accordance with the increased hemoglobin release. If liver failure occurred, as in choice (D), then it would be unable to produce bile, and bilirubin would again build up. Choice (C) refers to a pathology in the stomach—the key word given here is rugae, which are the folds in the stomach wall. Lack of gastric function would have no effect on bilirubin levels, making this the correct choice.
11.AChylomicrons contain triacylglycerols, cholesteryl esters, and fat-soluble vitamins and are secreted by intestinal cells into lacteals. Amino acids, fat-soluble vitamins (like vitamins A and E), and cholesterol are all absorbed in the small intestine.
12.BStarch is hydrolyzed to maltose by two enzymes: salivary amylase (secreted by the salivary glands) in the mouth and pancreatic amylase (secreted by the pancreas) in the duodenum. Brush-border disaccharidases can further break down maltose, but do not break down starch.
13.AWhile the capillaries from the intestine come together to form the portal vein, which drains to the liver, the lacteals come together to form the thoracic duct, which drains directly into the left subclavian vein. Therefore, fat-soluble compounds do not pass through the liver before reaching the right heart. Only choice (A), vitamin D, is fat-soluble.
14.CGhrelin promotes a sensation of hunger, increasing feeding behavior. Both leptin and cholecystokinin promote satiety, decreasing feeding behavior—eliminating choices (A) and (B). Gastrin increases acid production and gastric motility, but does not have any significant relationship with feeding behavior, eliminating choice (D).
15.DThe liver serves many functions, including metabolic processes (glycogenesis and glycogenolysis, fat storage, and gluconeogenesis), detoxification or activation of medications, and synthesis of bile. Germane to this question are the roles of converting ammonia into urea through the urea cycle and synthesis of proteins, including albumin and clotting factors. A patient with liver failure would thus not be able to convert ammonia into urea and would have high concentrations of ammonia and low concentrations of urea in the blood, eliminating choices (A) and(C). With decreased synthetic activity, both albumin and clotting factor concentrations would be low, eliminating choice (B) and making choice (D) the correct answer.