Medical Microbiology
Introduction
Microbes and parasites
The conventional distinction between “microbes” and “parasites” is essentially arbitrary
Microbiology is sometimes defined as the biology of microscopic organisms, its subject being the “microbes”. Traditionally, clinical microbiology has been concerned with those organisms responsible for the major infectious diseases of humans and whose size makes them invisible to the naked eye. Thus, it is not surprising that the organisms included have reflected those causing diseases that have been (or continue to be) of greatest importance in those countries where the scientific and clinical discipline of microbiology developed, notably Europe and the USA. The term “microbes” has usually been applied in a restricted fashion, primarily to viruses and bacteria. Fungi and protozoan parasites are included as relatively minor contributors, but in general they have been treated as the subjects of other disciplines (mycology and parasitology).
Although there can be no argument that viruses and bacteria are, globally, the most important pathogens, the conventional distinction between these as “microbes” and the other infectious agents (fungi, protozoan, worm and arthropod parasites) is essentially arbitrary, not least because the criterion of microscopic visibility cannot be applied rigidly (Fig. Intro.1). Perhaps we should remember that the first “microbe” to be associated with a specific clinical condition was a parasitic worm – the nematode Trichinella spiralis – whose larval stages are just visible to the naked eye (though microscopy is needed for certain identification). T. spiralis was first identified in 1835 and causally related to the disease trichinellosis in the 1860 s. Equally, viruses and bacteria comprise only just over half of all human pathogen species (Table Intro.1).
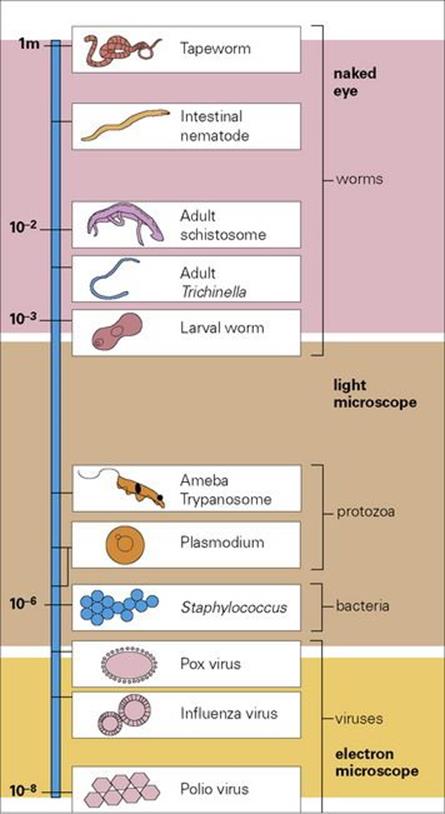
Figure Intro.1 Relative sizes of the organisms covered in this book.
Table Intro.1 Distribution of 1407 human pathogen species among the major groups of organisms (excluding arthropods)
|
Group |
% of total |
|
Viruses and prions |
14–15 |
|
Bacteria |
38–41 |
|
Fungi |
22–23 |
|
Protozoa |
4–5 |
|
Helminths |
20 |
Data from average of multiple studies summarized by Smith, K.F. and Guegan, J-F, (2010) Changing geographic distributions of human pathogens. Ann. Rev. Ecol. Evol. 41:231–250.
The context for contemporary medical microbiology
Many microbiology texts deal with infectious organisms as agents of disease in isolation, isolated both from other infectious organisms and from the biologic context in which they live and in which disease is caused. It is certainly convenient to list and deal with organisms group by group, to summarize the diseases they cause, and to review the forms of control available, but this approach produces a static picture of what is a dynamic relationship between the organism and its host.
Host response is the outcome of the complex interplay between host and parasite
Host response can be discussed in terms of pathologic signs and symptoms and in terms of immune control, but it is better treated as the outcome of the complex interplay between two organisms – host and parasite; without this dimension a distorted view of infectious disease results. It simply is not true that “microbe + host = disease”, and clinicians are well aware of this. Understanding why it is that most host–microbe contacts do not result in disease, and what changes so that disease does arise, is as important as the identification of infectious organisms and a knowledge of the ways in which they can be controlled.
We therefore continue to believe that our approach to microbiology, both in terms of the organisms that might usefully be considered within a textbook and also in terms of the contexts in which they and the diseases they cause are discussed, provides a more informative and more interesting picture of these dynamic interrelationships. There are many reasons for having reached this conclusion, the most important being the following:
• A comprehensive understanding now exists at the molecular level of the biology of infectious agents and of the host–parasite interactions that lead to infection and disease. It is important for students to be aware of this understanding so that they can grasp the connections between infection and disease within both individuals and communities and be able to use this knowledge in novel and changing clinical situations.
• It is now realized that the host”s response to infection is a coordinated and subtle interplay involving the mechanisms of both innate and acquired resistance, and that these mechanisms are expressed regardless of the nature and identity of the pathogen involved. Our present understanding of the ways in which these mechanisms are stimulated and the ways in which they act is very sophisticated. We can now see that infection is a conflict between two organisms, with the outcome (resistance or disease) being critically dependent upon molecular interactions. Again, it is essential to understand the basis of this host–pathogen interplay if the processes of disease and disease control are to be interpreted correctly.
Emerging or re-emerging diseases continue to pose new microbiologic problems
Three other factors have helped to mould our opinion that a broader view of microbiology is needed to provide a firm basis for clinical and scientific practice:
• There is an increasing prevalence of a wide variety of opportunistic infections in patients who are hospitalized or immunosuppressed. Immunosuppressive therapies are now more common, as are diseases in which the immune system is compromised – notably, of course, AIDS.
• Newly emerging disease agents continue to be identified, and old diseases, previously thought to be under control, re-emerge as causes of concern. Of the 1407 species identified as pathogenic for humans, 183 are regarded as emerging or re-emerging pathogens, almost half being viruses, some of animal origin (see Table Intro.1).
• Tropical infections are now of much greater interest. Clinicians see many tourists who have been exposed to the quite different spectrum of infectious agents found in tropical countries (at least 80 million people travel from resource-rich to resource-poor countries each year), and practicing microbiologists may be called upon to identify and advise on these organisms. There is also greater awareness of the health problems of the resource-poor world.
Thus, a broader view of microbiology is necessary; one that builds on the approaches of the past, but addresses the problems of the present and of the future.
Microbiology past, present and future
The demonstration in the nineteenth century that diseases were caused by infectious agents founded the discipline of microbiology. Although these early discoveries involved tropical parasitic infections as well as the bacterial infections common in Europe and the USA, microbiologists increasingly focused on the latter, later extending their interests to the newly discovered viral infections. The development of antimicrobial agents and vaccines revolutionized treatment of these diseases and raised hopes for the eventual elimination of many of the diseases that had plagued the human race for centuries. Those in the resource-rich world learned not to fear infectious disease and believed such infections would disappear in their lifetime. To an extent, this was realized; through vaccination, many familiar childhood diseases became uncommon, and those of bacterial origin were easily controlled by antibiotics. Encouraged by the eradication of smallpox during the 1970s, and the success of polio vaccines, the United Nations in 1978 announced programmes to obtain “Health for All” by 2000. However, this optimistic picture has had to be re-evaluated.
Infectious diseases are still killers in the resource-rich world
Globally, infectious diseases cause more than 20% of all deaths and kill an increasing number in both the resource-rich and the resource-poor world. In the USA (and the picture is similar in Europe):
• deaths from HIV peaked at 50 000 in 1995, but still exceed 15 000 each year
• influenza with underlying respiratory and circulatory issues results in 15 000 deaths each year and affects millions
• some 3 to 4 million people carry hepatitis C virus, and ca. 12 000 develop life-threatening chronic liver disease
• drug-resistant tuberculosis (TB) is a major cause of concern, as are food-borne infections and healthcare-associated infections.
Infectious diseases are a major problem in the resource-poor world, particularly in children
The burden of infectious disease in the resource-poor world is increasing at an alarming rate, particularly in sub-Saharan Africa and SE Asia. Although sub-Saharan Africa has only about 10% of the world”s population, it has 67% of AIDS infections and a majority of all AIDS-related deaths, the highest HIV-TB co-infection rates and most of the global malaria burden. TB and HIV-AIDS are of increasing importance in SE Asia and the Pacific, where drug-resistant malaria is also common. Children younger than 5 years are most at risk from infectious diseases. Of the 8.1 million deaths in this age group recorded by WHO for the year 2009, at least half were due to infection such as acute respiratory infection and diarrheal diseases. The overwhelming majority of these infection-related deaths occurred in Africa, SE Asia and the Eastern Mediterranean. It is obvious that the prevalence and importance of infectious diseases in the resource-poor world are directly linked to poverty. The infectious diseases of most importance globally are shown in Table Intro.2.
Table Intro.2 Major infectious disease-related deaths worldwide*
|
Cause |
Estimated number of deaths (millions) |
Percent of total deaths |
|
Lower respiratory tract infections |
4.18 |
7.1 |
|
Diarrheal diseases |
2.16 |
3.7 |
|
HIV/AIDS |
2.04 |
2.5 |
|
Tuberculosis |
1.46 |
2.5 |
* Data from WHO (2008).
Infections continue to emerge or re-emerge
On a world-wide basis, between 1940 and 2004, 335 infectious diseases emerged in the human population for the first time. Since the 1970s, some familiar diseases, including TB, malaria, hepatitis, cholera and dengue, have re-emerged as major infections and more recently a number of new infectious agents have been identified (Table Intro.3), of which HIV is the most important. For many new diseases, there is no effective treatment. The economic cost of these diseases is enormous. For example, the total lifetime cost, including loss of productivity, for Americans diagnosed with AIDS is estimated to be greater than US$30 billion and in high-prevalence countries malaria consumes approximately 40% of public health spending. Successful eradication could therefore save very large sums, for example, an estimated US$20 billion from eradicating smallpox.
Table Intro.3 Emerging diseases – examples of new infectious agents identified since the 1970s
|
Decade |
Organisms |
|
1980–1989 |
HTLV-1, HTLV-2, human herpes virus 6, HIV, hepatitis C, E. coli 0157, Borrelia burgdorferi, Helicobacter, toxin-producing Staph. aureus |
|
1990–1999 |
Hanta virus, human herpes virus 8, hepatitis E-G, vCJD, Hendra virus, Nipah virus, Vibrio cholerae 0139, Cryptosporidium, Cyclospora |
|
2000–present day |
SARS associated coronavirus, epizootic avian influenza H5N1, HTLV-3, HTLV-4, xenotropic MuLV-related virus |
HTLV, human T-cell lymphotropic virus; HIV, human immunodeficiency virus; vCJD, variant Creutzfeldt–Jakob disease; SARS, severe acute respiratory syndrome.
Modern lifestyles and technical developments facilitate transmission of disease
The reasons for the resurgence of infectious diseases are multiple. They include:
• New patterns of travel and trade (especially food commodities), new agricultural practices, altered sexual behaviour, medical interventions and overuse of antibiotics.
• The evolution of multi-drug resistant bacteria, such as MRSA, and their frequency in both healthcare and community settings have become major problems. The issue of antimicrobial resistance is compounded in resource-poor countries by inability or unwillingness to complete programmes of treatment, as seems to have happened with TB, and by the use of counterfeit drugs with, at best, partial action. The WHO estimates that globally 10% of antimicrobials (25% in resource-poor countries) are counterfeit, and a survey of seven African countries revealed that 20% to 90% of antimalarial drugs were substandard. In 2006, the WHO launched a new initiative to combat the lucrative business of counterfeit medical products including antibiotics and vaccines
• Breakdown of economic, social and political systems especially in the resource-poor world has weakened medical services and increased the effects of poverty and malnutrition.
• The dramatic increase in air travel over the last few decades has facilitated the spread of infection and increased the threat of new pandemics. The Spanish influenza pandemic in 1918 spread along railway and sea links. Modern air travel moves larger numbers of people more rapidly and more extensively and makes it possible for microbes to cross geographical barriers. The potential for spread of the SARS virus from Asia to Europe and North America provided a salutary reminder of these dangers.
What of the future?
Predictions based on data from the United Nations and the World Health Organization give a choice of optimistic, stable or pessimistic scenarios. Optimistically, the aging population, coupled with socioeconomic and medical advances, should see a fall in the problems posed by infectious disease, and a decrease in deaths from these causes from 34% of the global total in 1990 to 15% in 2020; HIV and TB would, however, still be responsible for a majority of deaths from infection. In 2009, 1.7 million people died of TB, 24% of whom were HIV positive, and 22% of the 1.8 million deaths in HIV-positive individuals were due to TB. The pessimistic view is that population growth in resource-poor countries, especially in urban populations, the increasing gap between rich and poor countries, and continuing changes in lifestyle will result in surges of infectious disease. Even in resource-rich countries, increasing drug resistance and a slowing of developments in new antimicrobials and vaccines will create problems in control. Added to these are three additional factors. These are:
• the emergence of new human infections such as a novel strain of influenza virus, or a new infection of wildlife origin
• climate change, with increased temperatures and altered rainfall adding to the incidence of vector-borne infection
• the threat of bioterrorism, with the possible deliberate spread of viral and bacterial infections.
The deliberate spread of anthrax through the US mail system in 2002 raised the frightening possibility that previously rare but potentially deadly infections might be deliberately spread to human populations with no acquired immunity or no history of vaccination. The range of organisms that could be used in this way includes exotic viruses (e.g. those causing haemorrhagic fevers and encephalitis), genetically modified organisms, or organisms such as smallpox, thought now to be extinct.
One thing is certain: whether optimistic or pessimistic scenarios prove true, microbiology will remain a critical medical discipline for the foreseeable future.
The approach adopted in this book
The factors outlined above indicate the need for a text with a dual function:
1. It should provide an inclusive treatment of the organisms responsible for infectious disease.
2. The purely clinical/laboratory approach to microbiology should be replaced with an approach that will stress the biologic context in which clinical/laboratory studies are to be undertaken.
The approach we have adopted in this book is to look at microbiology from the viewpoint of the conflicts inherent in all host–pathogen relationships. We first describe the adversaries: the infectious organisms on the one hand, and the innate and adaptive defence mechanisms of the host on the other. The outcome of the conflicts between the two is then amplified and discussed system by system. Rather than taking each organism or each disease manifestation in turn, we look at the major environments available for infectious organisms in the human body, such as the respiratory system, the gut, the urinary tract, the blood and the central nervous system. The organisms that invade and establish in each of these are examined in terms of the pathologic responses they provoke. Finally, we look at how the conflicts we have described can be controlled or eliminated, both at the level of the individual patient and at the level of the community. We hope that such an approach will provide readers with a dynamic view of host–pathogen interactions and allow them to develop a more creative understanding of infection and disease.
![]()
 Key Facts
Key Facts
• Our approach is to provide a comprehensive account of the organisms that cause infectious disease in humans, from the viruses to the worms, and to cover the biologic bases of infection, disease, host–pathogen interactions, disease control and epidemiology.
• The diseases caused by microbial pathogens will be placed in the context of the conflict that exists between them and the innate and adaptive defences of their hosts.
• Infections will be described and discussed in terms of the major body systems, treating these as environments in which microbes can establish themselves, flourish and give rise to pathologic changes.