Medical Microbiology
Section 1 The adversaries – microbes
4 The fungi
Introduction
Fungi are eukaryotes, but are quite distinct from plants and animals. Characteristically, they are multinucleate or multicellular organisms with a thick carbohydrate cell wall containing chitin, glucans, mannans and glycoproteins. They may grow as thread-like filaments (hyphae), but many other growth forms occur. Of these, the single-celled yeasts and the mushroom are most familiar. Fungi are ubiquitous as free-living organisms and are of enormous importance commercially in baking, brewing and in pharmaceuticals. Some form part of the body’s normal flora, and others are common causes of local infections on skin and hair. A number of fungi are associated with significant disease and many of these are acquired from the external environment. Pathogenic species invade tissues and digest material externally by releasing enzymes; they also take up nutrients directly from host tissues. In recent years, invasive fungal disease has assumed much greater prominence in clinical practice as a result of the rise in number of severely immunocompromised patients. The study of fungi is known as mycology and fungal infections are known as mycoses.
Major groups of disease-causing fungi
Importance of fungi in causing disease
There are more than 70 000 species of fungi but only about 300 are identified as pathogens in humans and animals. Some of these are cosmopolitan, others are found mainly in tropical regions. Some, those that infect superficially, cause only minor health problems but those that invade deeper tissues can be life threatening. These systemic forms have become much more serious problems as medical advances have taken place, e.g. immunosuppressive and antibiotic therapies, transplantation, invasive procedures and AIDS, such that opportunistic infections are now significant components of hospital-acquired infection.
Fungal pathogens can be classified on the basis of their growth forms or the type of infection they cause
Fungi were reclassified down to the level of order in 2007 following advances in fungal molecular taxonomy. Whilst this has no immediate effect on the practice of clinical microbiology, it will lead to greater understanding of the biology of the Kingdom Fungi and the diseases its members may cause.
Fungal pathogens may exist as branched filamentous forms or as yeasts (Fig. 4.1); some show both growth forms in their cycle and are known as dimorphic fungi. In filamentous forms (e.g. Trichophyton), the mass of hyphae forms a mycelium. Asexual reproduction results in the formation of sporangia, which are sacs that contain and then liberate the spores by which the fungus is dispersed; spores are a common cause of infection after inhalation. In yeast-like forms (e.g. Cryptococcus) the characteristic form is the single cell, which reproduces by division. Budding may also occur, with the bud remaining attached, forming pseudohyphae. Dimorphic forms (e.g. Histoplasma) form hyphae at environmental temperatures, but occur as yeast cells in the body, the switch being temperature-induced. Candida is an important exception in the dimorphic group, showing the reverse and forming hyphae within the body.
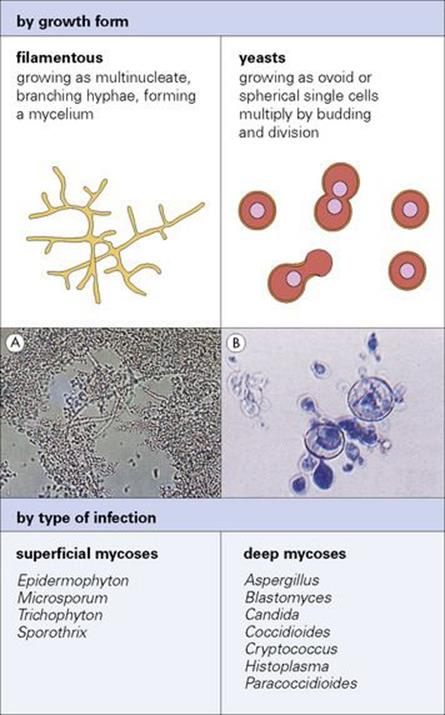
Figure 4.1 Two ways to classify fungi that cause disease: by growth form and by type of infection. (A) Hyphae in skin scraping from ringworm lesion.
(Courtesy of D.K. Banerjee.) (B) Spherical yeasts of Histoplasma. (Courtesy of Y. Clayton and G. Midgley.)
Three types of infection (mycoses) are recognized:
• Superficial mycoses where the fungus grows on body surfaces (skin, hair, nails, mouth, vagina). Examples are tinea pedis (athlete’s foot) and vaginal candidiasis (thrush).
• Subcutaneous mycoses where nails and deeper layers of the skin are involved. Examples are mycetoma (Madura foot) and sporotrichosis.
• Systemic or deep mycoses with involvement of internal organs. This category includes fungi capable of infecting individuals with normal immunity and the opportunistic fungi that cause disease in patients with compromised immune systems. Examples are histoplasmosis and systemic candidiasis.
The superficial mycoses are spread by person-to-person contact or from animal-to-human contact (e.g. from cats and dogs); the subcutaneous mycoses infect humans via the skin (e.g. following skin penetration in the case of mycetoma); the deep mycoses often result from the opportunistic growth of fungi in individuals with impaired immune competence and are primarily acquired via the respiratory tract (see Ch. 30), with intravenous lines an important portal of entry for Candida. Free-living fungi can also cause disease. This occurs indirectly when toxins produced by fungi are present in items used as food (e.g. aflatoxin, a carcinogen produced by Aspergillus flavus) or when their spores are inhaled, an immune response occurs and a hypersensitivity pneumonitis develops (allergic bronchopulmonary aspergillosis).
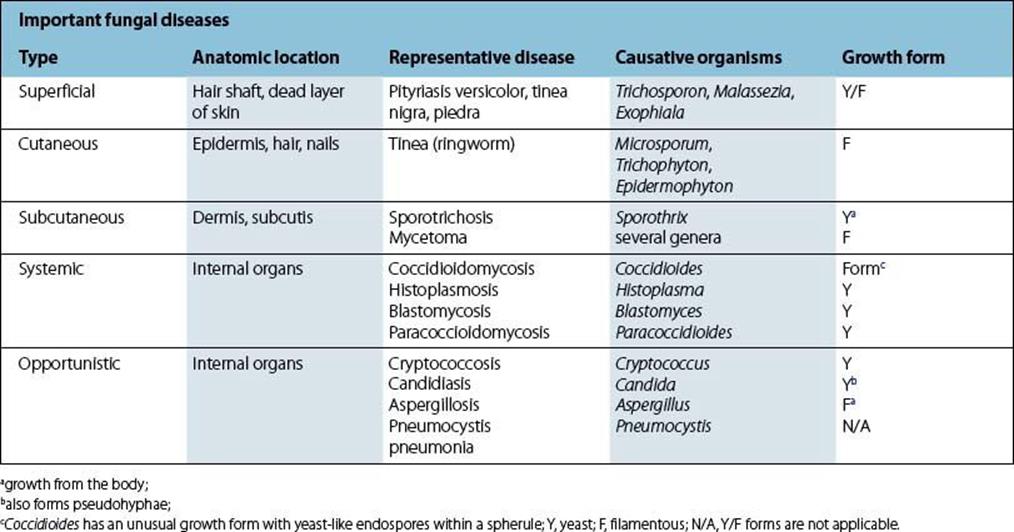
Many of the fungi that cause disease are normally free-living in the environment, but can survive in the body if acquired by inhalation or by entry through wounds. Some fungi are part of the normal flora (e.g. Candida) and are innocuous unless the body’s defences are compromised, e.g. by underlying malignancy, diabetes mellitus or intravenous drug use. The filamentous forms grow extracellularly, but yeasts can survive and multiply within macrophages and neutrophils. Neutrophils can play a major role in controlling the establishment of invading fungi. Species that are too large for phagocytosis can be killed by extracellular factors released from phagocytes as well as by other components of the immune response. Some species, notably Cryptococcus neoformans, prevent phagocytic uptake because they are surrounded by a polysaccharide capsule (see Chs 24and 30). Until, recently, Pneumocystis, an important opportunistic infection in AIDS patients, was classified as a protozoan, but it is now regarded as an atypical fungus. It attaches to lung cells (pneumocytes) and can give rise to a fatal pneumonia. Other pathogens previously thought to be protozoa may also turn out to be fungi, e.g. the microsporidia. The major groups of fungi causing human disease are shown in Table 4.1.
Table 4.1 Summary of fungi that cause important human diseases
Control of fungal infection
The echinocandins inhibit glucan synthesis in the fungal cell wall. Below the fungal cell wall lies the plasma membrane or plasmalemma. Unlike human plasma membranes, where the dominant sterol is cholesterol, the fungal membrane is rich in ergosterol. Compounds that selectively bind to ergosterol can therefore be used as effective fungal agents. These include the polyenes nystatin and amphotericin B. The azoles (e.g. miconazole) and the allylamines (e.g. terbinafine) inhibit ergosterol synthesis. The pyrimidines (e.g. flucytosine) inhibit nucleic acid synthesis.
![]()
 Key Facts
Key Facts
• Fungi are distinct from plants and animals, have a thick chitin-containing cell wall, and grow as filaments (hyphae) or single-celled yeasts.
• Species causing disease may be acquired from the environment or occur as part of the normal flora.
• Infections may be located superficially, in cutaneous and subcutaneous sites, or in deep tissues.
• Infections are most serious in immunocompromised individuals.
![]()
![]()
 Conflicts
Conflicts
Fungi are versatile; the same species can be both free-living in the external environment and cause disease. Thus there is always a plentiful reservoir of infection. Fungi are physiologically versatile too, and can grow at a wide range of temperatures. Their reproductive stages (spores) are small, can be air-borne and easily inhaled. As they have a resistant chitinous coat, and may produce antiphagocytic factors, they can be difficult for innate defence systems to deal with. Once past the defences of the respiratory system many fungi change growth form and invade deeper tissues, often forming a network of elongate hyphae (e.g. in aspergillosis), which are even more difficult to defend against; indeed immunological responses may aggravate systemic pathology. The prevalence of infective stages in the environment and the ability of fungi to grow rapidly in the absence of effective defences makes fungal infection a major hazard for immunocompromised patients. The balance is further tipped in their favour by the difficulty in diagnosing deep-seated mycoses and by the toxicity to the host of some of the drugs used to treat them. Fortunately, immunologically competent individuals appear to deal well with what must be frequent exposure, although the potential for disease is always present.
![]()