Lippincott’s Illustrated Reviews: Biochemistr, Sixth Edition (2014)
UNIT II: Bioenergetics and Carbohydrate Metabolism
Chapter 12. Metabolism of Monosaccharides and Disaccharides
I. OVERVIEW
Glucose is the most common monosaccharide consumed by humans, and its metabolism has already been discussed. However, two other monosaccharides, fructose and galactose, occur in significant amounts in the diet (primarily in disaccharides) and make important contributions to energy metabolism. In addition, galactose is an important component of structural carbohydrates. Figure 12.1 shows the metabolism of fructose and galactose as part of the essential pathways of energy metabolism.
Figure 12.1 Galactose and fructose metabolism as part of the essential pathways of energy metabolism (see Figure 8.2, p. 92, for a more detailed view of the overall reactions of metabolism). UDP = uridine diphosphate; P = phosphate.

II. FRUCTOSE METABOLISM
About 10% of the calories comprising the Western diet are supplied by fructose (approximately 55 g/day). The major source of fructose is the disaccharide sucrose, which, when cleaved in the intestine, releases equimolar amounts of fructose and glucose. Fructose is also found as a free monosaccharide in many fruits, in honey, and in high-fructose corn syrup (typically, 55% fructose/45% glucose), which is used to sweeten soft drinks and many foods. Fructose transport into cells is not insulin dependent (unlike that of glucose into certain tissues; see p. 97), and, in contrast to glucose, fructose does not promote the secretion of insulin.
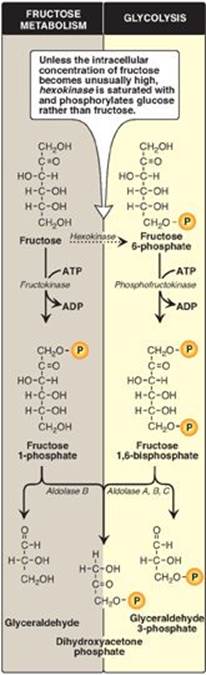
A. Phosphorylation of fructose
For fructose to enter the pathways of intermediary metabolism, it must first be phosphorylated (Figure 12.2). This can be accomplished by either hexokinase or fructokinase. Hexokinase phosphorylates glucose in most cells of the body (see p. 98), and several additional hexoses can serve as substrates for this enzyme. However, it has a low affinity (that is, a high Michaelis constant [Km]; see p. 59) for fructose. Therefore, unless the intracellular concentration of fructose becomes unusually high, the normal presence of saturating concentrations of glucose means that little fructose is phosphorylated by hexokinase. Fructokinase provides the primary mechanism for fructose phosphorylation (see Figure 12.2). The enzyme has a low Km for fructose and a high Vmax (or, maximal velocity; see p. 59). It is found in the liver (which processes most of the dietary fructose), kidney, and the small intestinal mucosa and converts fructose to fructose 1-phosphate, using adenosine triphosphate (ATP) as the phosphate donor. [Note: These three tissues also contain aldolase B, discussed in section B.]
B. Cleavage of fructose 1-phosphate
Fructose 1-phosphate is not phosphorylated to fructose 1,6-bisphos-phate as is fructose 6-phosphate (see p. 99) but is cleaved by aldolase B (also called fructose 1-phosphate aldolase) to dihydroxyacetone phosphate (DHAP) and glyceraldehyde. [Note: Humans express three aldolases, A, B and C, the products of three different genes. Aldolase A (found in most tissues), aldolase B (in liver, kidney, and small intestine), and aldolase C (in brain) all cleave fructose 1,6-bisphosphate produced during glycolysis to DHAP and glyceraldehyde 3-phosphate (see p. 100), but only aldolase B cleaves fructose 1-phosphate.] DHAP can directly enter glycolysis or gluconeogenesis, whereas glyceraldehyde can be metabolized by a number of pathways, as illustrated in Figure 12.3.
Figure 12.2 Phosphorylation products of fructose and their cleavage. P = phosphate; ADP = adenosine diphosphate.
C. Kinetics of fructose metabolism
The rate of fructose metabolism is more rapid than that of glucose because the trioses formed from fructose 1-phosphate bypass phosphofructokinase-1, the major rate-limiting step in glycolysis (see p. 99).
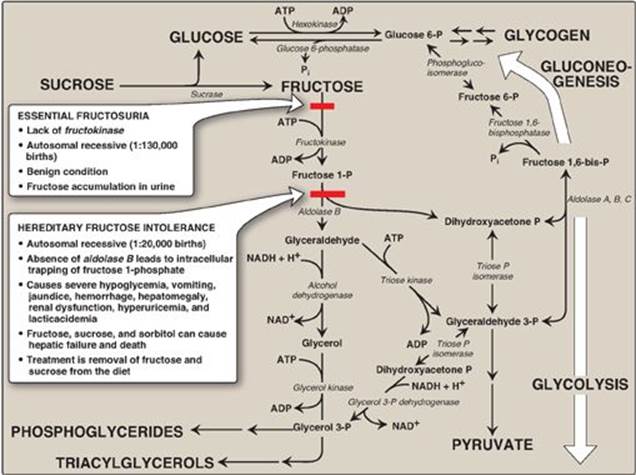
D. Disorders of fructose metabolism
A deficiency of one of the key enzymes required for the entry of fructose into metabolic pathways can result in either a benign condition as a result of fructokinase deficiency (essential fructosuria) or a severe disturbance of liver and kidney metabolism as a result of aldolase B deficiency (hereditary fructose intolerance [HFI]), which is estimated to occur in 1:20,000 live births (see Figure 12.3). The first symptoms of HFI appear when a baby is weaned from milk (see p. 142) and begins to be fed food containing sucrose or fructose. Fructose 1-phosphate accumulates, resulting in a drop in the level of inorganic phosphate (Pi) and, therefore, of ATP production. As ATP falls, adenosine monophosphate (AMP) rises. The AMP is degraded, causing hyperuricemia (and lactic acidosis; see p. 299). The decreased availability of hepatic ATP affects gluconeogenesis (causing hypoglycemia with vomiting) and protein synthesis (causing a decrease in blood clotting factors and other essential proteins). Kidney function may also be affected. [Note: The drop in Pi also inhibits glycogenolysis (see p. 128).] Diagnosis of HFI can be made on the basis of fructose in the urine, enzyme assay using liver cells, or by DNA-based testing (see Chapter 33). Aldolase B deficiency is part of the newborn screening panel. With HFI, sucrose, as well as fructose, must be removed from the diet to prevent liver failure and possible death. Individuals with HFI display an aversion to sweets and, consequently, have an absence of dental caries.
E. Conversion of mannose to fructose 6-phosphate
Mannose, the C-2 epimer of glucose (see p. 84), is an important component of glycoproteins (see p. 166). Hexokinase phosphorylates mannose, producing mannose 6-phosphate, which, in turn, is reversibly isomerized to fructose 6-phosphate by phosphomannose isomerase. [Note: There is little mannose in dietary carbohydrates. Most intracellular mannose is synthesized from fructose or is preexisting mannose produced by the degradation of structural carbohydrates and salvaged by hexokinase.]
Figure 12.3 Summary of fructose metabolism. P = phosphate; Pi = inorganic phosphate; NAD(H) = nicotinamide adenine dinucleotide; ADP = adenosine diphosphate.
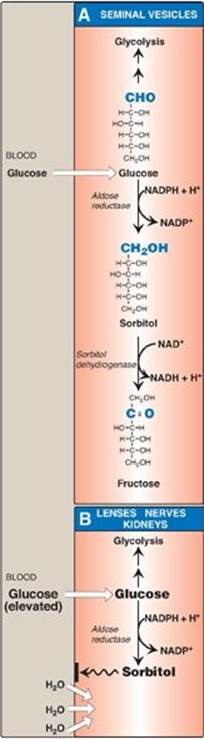
F. Conversion of glucose to fructose via sorbitol
Most sugars are rapidly phosphorylated following their entry into cells. Therefore, they are trapped within the cells, because organic phosphates cannot freely cross membranes without specific transporters. An alternate mechanism for metabolizing a monosaccharide is to convert it to a polyol (sugar alcohol) by the reduction of an aldehyde group, thereby producing an additional hydroxyl group.
1. Synthesis of sorbitol: Aldose reductase reduces glucose, producing sorbitol (glucitol; Figure 12.4). This enzyme is found in many tissues, including the lens, retina, Schwann cells of peripheral nerves, liver, kidney, placenta, red blood cells, and cells of the ovaries and seminal vesicles. In cells of the liver, ovaries, and seminal vesicles, there is a second enzyme, sorbitol dehydrogenase, which can oxidize the sorbitol to produce fructose (see Figure 12.4). The two-reaction pathway from glucose to fructose in the seminal vesicles benefits sperm cells, which use fructose as a major carbohydrate energy source. The pathway from sorbitol to fructose in the liver provides a mechanism by which any available sorbitol is converted into a substrate that can enter glycolysis or gluconeogenesis.
2. Effect of hyperglycemia on sorbitol metabolism: Because insulin is not required for the entry of glucose into the cells listed in the previous paragraph, large amounts of glucose may enter these cells during times of hyperglycemia (for example, in uncontrolled diabetes). Elevated intracellular glucose concentrations and an adequate supply of reduced nicotinamide adenine dinucleotide phosphate (NADPH) cause aldose reductase to produce a significant increase in the amount of sorbitol, which cannot pass efficiently through cell membranes and, in turn, remains trapped inside the cell (see Figure 12.4). This is exacerbated when sorbitol dehydrogenase is low or absent (for example, in retina, lens, kidney, and nerve cells). As a result, sorbitol accumulates in these cells, causing strong osmotic effects and, therefore, cell swelling as a result of water retention. Some of the pathologic alterations associated with diabetes can be attributed, in part, to this phenomenon, including cataract formation, peripheral neuropathy, and microvascular problems leading to nephropathy and retinopathy. (See p. 344 for a discussion of the complications of diabetes.) [Note: Use of NADPH in the aldose reductase reaction decreases the generation of reduced glutathione, an important antioxidant (see p. 148), and may be related to diabetic complications.]
Figure 12.4 Sorbitol metabolism. NAD(H) = nicotinamide adenine dinucleotide; NADP(H) = nicotinamide adenine dinucleotide phosphate.
III. GALACTOSE METABOLISM
The major dietary source of galactose is lactose (galactosyl β-1,4-glucose) obtained from milk and milk products. [Note: The digestion of lactose by β-galactosidase (lactase) of the intestinal mucosal cell membrane was discussed on p. 87.] Some galactose can also be obtained by lysosomal degradation of complex carbohydrates, such as glycoproteins and glycolipids, which are important membrane components. Like fructose, the transport of galactose into cells is not insulin dependent.
A. Phosphorylation of galactose
Like fructose, galactose must be phosphorylated before it can be further metabolized. Most tissues have a specific enzyme for this purpose, galactokinase, which produces galactose 1-phosphate (Figure 12.5). As with other kinases, ATP is the phosphate donor.
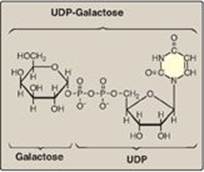
B. Formation of uridine diphosphate-galactose
Galactose 1-phosphate cannot enter the glycolytic pathway unless it is first converted to uridine diphosphate (UDP)-galactose (Figure 12.6). This occurs in an exchange reaction, in which UDP-glucose reacts with galactose 1-phosphate, producing UDP-galactose and glucose 1-phosphate (see Figure 12.5). The enzyme that catalyzes this reaction is galactose 1-phosphate uridylyltransferase (GALT).
C. Use of uridine diphosphate-galactose as a carbon source for glycolysis or gluconeogenesis
For UDP-galactose to enter the mainstream of glucose metabolism, it must first be converted to its C-4 epimer, UDP-glucose, by UDP-hexose 4-epimerase. This “new” UDP-glucose (produced from the original UDP-galactose) can then participate in many biosynthetic reactions as well as being used in the GALT reaction described above. (See Figure 12.5 for a summary of this interconversion.)
Figure 12.5 Metabolism of galactose. UDP = uridine diphosphate; UTP = uridine triphosphate; P = phosphate; PPi = pyrophosphate; NADP(H) = nicotinamide adenine dinucleotide phosphate; ADP = adenosine diphosphate.
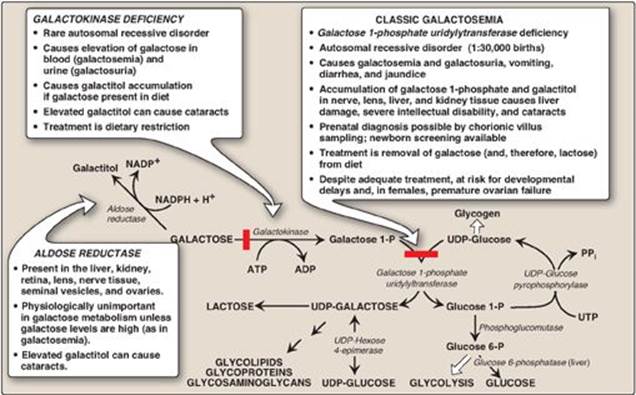
D. Role of uridine diphosphate-galactose in biosynthetic reactions
UDP-galactose can serve as the donor of galactose units in a number of synthetic pathways, including synthesis of lactose (see below), glycoproteins (see p. 166), glycolipids (see p. 210), and glycosaminoglycans (see p. 158). [Note: If galactose is not provided by the diet (for example, when it cannot be released from lactose as a result of a lack of β-galactosidase in people who are lactose intolerant), all tissue requirements for UDP-galactose can be met by the action of UDP-hexose 4-epimerase on UDP-glucose, which is efficiently produced from glucose 1-phosphate (see Figure 12.5).]
E. Disorders of galactose metabolism
GALT is deficient in individuals with classic galactosemia (see Figure 12.5). In this disorder, galactose 1-phosphate and, therefore, galactose accumulate. Physiologic consequences are similar to those found in hereditary fructose intolerance (see p. 138), but a broader spectrum of tissues is affected. The accumulated galactose is shunted into side pathways such as that of galactitol production. This reaction is catalyzed by aldose reductase, the same enzyme that converts glucose to sorbitol (see p. 139). Treatment requires removal of galactose and lactose from the diet. GALT deficiency is part of the newborn screening panel. [Note: A deficiency in galactokinase results in a less severe disorder of galactosemia metabolism, although cataracts are common (see Figure 12.5).]
Figure 12.6 Structure of UDP-galactose. UDP = uridine diphosphate.
IV. LACTOSE SYNTHESIS
Lactose is a disaccharide that consists of a molecule of β-galactose attached by a β(1→4) linkage to glucose. Therefore, lactose is galactosyl β(1→4)-glucose. Lactose, known as “milk sugar,” is made by lactating (milk-producing) mammary glands. Therefore, milk and other dairy products are the dietary sources of lactose. Lactose is synthesized in the Golgi by lactose synthase (UDP-galactose:glucose galactosyltransferase), which transfers galactose from UDP-galactose to glucose, releasing UDP (Figure 12.7). This enzyme is composed of two proteins, A and B. Protein A is a β-D-galactosyltransferase and is found in a number of body tissues. In tissues other than the lactating mammary gland, this enzyme transfers galactose from UDP-galactose to N-acetyl-D-glucosamine, forming the same β(1→4) linkage found in lactose, and producing N-acetyllactosamine, a component of the structurally important N-linked glycoproteins (see p. 167). In contrast, protein B is found only in lactating mammary glands. It is α-lactalbumin, and its synthesis is stimulated by the peptide hormone prolactin. Protein B forms a complex with the enzyme, protein A, changing the specificity of that transferase so that lactose, rather than N-acetyllactosamine, is produced (see Figure 12.7).
Figure 12.7 Lactose synthesis. UDP = uridine diphosphate.

V. CHAPTER SUMMARY
The major source of fructose is sucrose, which, when cleaved, releases equimolar amounts of fructose and glucose (Figure 12.8). Transport of fructose into cells is insulin independent. Fructose is first phosphorylated to fructose 1-phosphate by fructokinase and then cleaved by aldolase B to dihydroxyacetone phosphate and glyceraldehyde. These enzymes are found in the liver, kidney, and small intestinal mucosa. A deficiency of fructokinase causes a benign condition (essential fructosuria), but a deficiency of aldolase B causes hereditary fructose intolerance (HFI), in which severe hypoglycemia and liver failure lead to death if fructose (and sucrose) in the diet is not eliminated. Mannose, an important component of glycoproteins, is phosphorylated by hexokinase to mannose 6-phosphate, which is reversibly isomerized to fructose 6-phosphate by phosphomannose isomerase. Glucose can be reduced to sorbitol (glucitol) by aldose reductase in many tissues, including the lens, retina, Schwann cells, liver, kidney, ovaries, and seminal vesicles. In cells of the liver, ovaries, and seminal vesicles, a second enzyme, sorbitol dehydrogenase, can oxidize sorbitol to produce fructose. Hyperglycemia results in the accumulation of sorbitol in those cells lacking sorbitol dehydrogenase. The resulting osmotic events cause cell swelling and may contribute to the cataract formation, peripheral neuropathy, nephropathy, and retinopathy seen in diabetes. The major dietary source of galactose is lactose. The transport of galactose into cells is not insulin dependent. Galactose is first phosphorylated by galactokinase (a deficiency results in cataracts) to galactose 1-phosphate. This compound is converted to uridine diphosphate (UDP)-galactose by galactose 1-phosphate uridyltransferase (GALT), with the nucleotide supplied by UDP-glucose. A deficiency of this enzyme causes classic galactosemia. Galactose 1-phosphate accumulates, and excess galactose is converted to galactitol by aldose reductase. This causes liver damage, severe intellectual disability, and cataracts. Treatment requires removal of galactose (and lactose) from the diet. For UDP-galactose to enter the mainstream of glucose metabolism, it must first be converted to UDP-glucose by UDP-hexose 4-epimerase. This enzyme can also be used to produce UDP-galactose from UDP-glucose when the former is required for the synthesis of structural carbohydrates. Lactose is a disaccharide that consists of galactose and glucose. Milk and other dairy products are the dietary sources of lactose. Lactose is synthesized by lactose synthase from UDP-galactose and glucose in the lactating mammary gland. The enzyme has two subunits, protein A (which is a galactosyltransferase found in most cells where it synthesizes N-acetyllactosamine) and protein B (α-lactalbumin, which is found only in the lactating mammary glands, and whose synthesis is stimulated by the peptide hormone prolactin). When both subunits are present, the transferase produces lactose.
Figure 12.8 Key concept map for metabolism of fructose and galactose. GALT = galactose 1-phosphate uridylyltransferase; UDP = uridine diphosphate; P = phosphate.

Study Questions
Choose the ONE best answer.
12.1 A nursing female with classic galactosemia is on a galactose-free diet. She is able to produce lactose in breast milk because:
A. galactose can be produced from fructose by isomerization.
B. galactose can be produced from a glucose metabolite by epimerization.
C. hexokinase can efficiently phosphorylate galactose to galactose 1-phosphate.
D. the enzyme affected in galactosemia is activated by a hormone produced in the mammary gland.
Correct answer = B. Uridine diphosphate (UDP)-glucose is converted to UDP-galactose by UDP-hexose 4-epimerase, thereby providing the appropriate form of galactose for lactose synthesis. Isomerization of fructose to galactose does not occur in the human body. Galactose is not converted to galactose 1-phosphate by hexokinase. A galactose-free diet provides no galactose. Galactosemia is the result of an enzyme deficiency.
12.2 A 5-month-old boy is brought to his physician because of vomiting, night sweats, and tremors. History revealed that these symptoms began after fruit juices were introduced to his diet as he was being weaned off breast milk. The physical examination was remarkable for hepatomegaly. Tests on the baby’s urine were positive for reducing sugar but negative for glucose. The infant most likely suffers from a deficiency of:
A. aldolase B.
B. fructokinase.
C. galactokinase.
D. β-galactosidase.
Correct answer = A. The symptoms suggest hereditary fructose intolerance, a deficiency in aldolase B. Deficiencies in fructokinase or galactokinase result in relatively benign conditions characterized by elevated levels of fructose or galactose in the blood and urine. Deficiency in β-galactosidase (lactase) results in a decreased ability to degrade lactose (milk sugar). Congenital lactase deficiency is quite rare and would have presented much earlier in this baby (and with different symptoms). Typical lactase deficiency (adult hypolactasia) presents at a later age.
12.3 Lactose synthesis is essential in the production of milk by mammary glands. In lactose synthesis:
A. galactose from galactose 1-phosphate is transferred to glucose by galactosyltransferase (protein A), generating lactose.
B. protein A is used exclusively in the synthesis of lactose.
C. α-lactalbumin (protein B) regulates the specificity of protein A by increasing its Km for glucose.
D. protein B expression is stimulated by prolactin.
Correct answer = D. The expression of α-lactalbumin (protein B) is increased by the hormone prolactin. Uridine diphosphate–galactose is the form used by the galactosyltransferase (protein A). Protein A is also involved in the synthesis of the amino sugar, N-acetyllactosamine. Protein B increases the affinity of protein A for glucose and, so, decreases the Km.
12.4 A 3-month-old girl is developing cataracts. Other than not having a social smile or being able to track objects visually, all other aspects of the girl’s examination are normal. Tests on the baby’s urine are positive for reducing sugar but negative for glucose. Which enzyme is most likely deficient in this girl?
A. Aldolase B
B. Fructokinase
C. Galactokinase
D. Galactose 1-phosphate uridylyltransferase
Correct answer = C. The girl is deficient in galactokinase and is unable to appropriately phosphorylate galactose. Galactose accumulates in the blood (and urine). In the lens of the eye, galactose is reduced by aldose reductase to galactitol, a sugar alcohol, which causes osmotic effects that result in cataract formation. Deficiency of galactose 1-phosphate uridylyltransferase also results in cataracts but is characterized by liver damage and neurologic effects. Fructokinase deficiency is a benign condition. Aldolase B deficiency is severe, with affects on several tissues. Cataracts are not typically seen.