Lippincott’s Illustrated Reviews: Biochemistr, Sixth Edition (2014)
UNIT I: Protein Structure and Function
Chapter 4. Fibrous Proteins
I. OVERVIEW
Collagen and elastin are examples of common, well-characterized fibrous proteins of the extracellular matrix that serve structural functions in the body. For example, collagen and elastin are found as components of skin, connective tissue, blood vessel walls, and the sclera and cornea of the eye. Each fibrous protein exhibits special mechanical properties, resulting from its unique structure, which are obtained by combining specific amino acids into regular, secondary structural elements. This is in contrast to globular proteins, whose shapes are the result of complex interactions between secondary, tertiary, and, sometimes, quaternary structural elements.
II. COLLAGEN
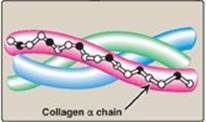
Collagen is the most abundant protein in the human body. A typical collagen molecule is a long, rigid structure in which three polypeptides (referred to as α chains) are wound around one another in a rope-like triple helix (Figure 4.1). Although these molecules are found throughout the body, their types and organization are dictated by the structural role collagen plays in a particular organ. In some tissues, collagen may be dispersed as a gel that gives support to the structure, as in the extracellular matrix or the vitreous humor of the eye. In other tissues, collagen may be bundled in tight, parallel fibers that provide great strength, as in tendons. In the cornea of the eye, collagen is stacked so as to transmit light with a minimum of scattering. Collagen of bone occurs as fibers arranged at an angle to each other so as to resist mechanical shear from any direction.
Figure 4.1 Triple-stranded helix of collagen.
A. Types
The collagen superfamily of proteins includes more than 25 collagen types as well as additional proteins that have collagen-like domains. The three polypeptide α chains are held together by interchain hydrogen bonds. Variations in the amino acid sequence of the α chains result in structural components that are about the same size (approximately 1,000 amino acids long) but with slightly different properties. These α chains are combined to form the various types of collagen found in the tissues. For example, the most common collagen, type I, contains two chains called α1 and one chain called α2 (α12α2), whereas type II collagen contains three α1 chains (α13). The collagens can be organized into three groups, based on their location and functions in the body (Figure 4.2).
Figure 4.2 The most abundant types of collagen. *Known as FACITs: fibril-associated collagens with interrupted triple helices.

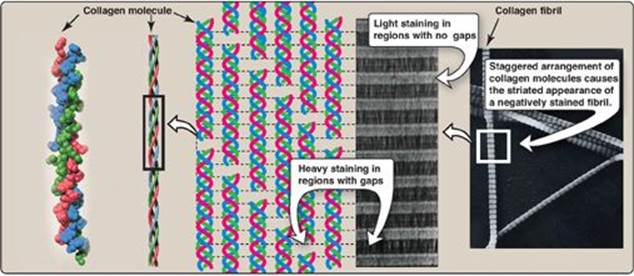
1. Fibril-forming collagens: Types I, II, and III are the fibrillar collagens and have the rope-like structure described above for a typical collagen molecule. In the electron microscope, these linear polymers of fibrils have characteristic banding patterns, reflecting the regular staggered packing of the individual collagen molecules in the fibril (Figure 4.3). Type I collagen fibers (composed of collagen fibrils) are found in supporting elements of high tensile strength (for example, tendon and cornea), whereas fibers formed from type II collagen molecules are restricted to cartilaginous structures. The fibers derived from type III collagen are prevalent in more distensible tissues such as blood vessels.
2. Network-forming collagens: Types IV and VIII form a three-dimensional mesh, rather than distinct fibrils (Figure 4.4). For example, type IV molecules assemble into a sheet or meshwork that constitutes a major part of basement membranes.
Basement membranes are thin, sheet-like structures that provide mechanical support for adjacent cells and function as a semipermeable filtration barrier to macromolecules in organs such as the kidney and the lung.
3. Fibril-associated collagens: Types IX and XII bind to the surface of collagen fibrils, linking these fibrils to one another and to other components in the extracellular matrix (see Figure 4.2).
Figure 4.3 Collagen fibrils at right have a characteristic banding pattern, reflecting the regularly staggered packing of the individual collagen molecules in the fibril.
B. Structure
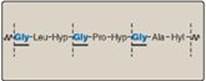
1. Amino acid sequence: Collagen is rich in proline and glycine, both of which are important in the formation of the triple-stranded helix. Proline facilitates the formation of the helical conformation of each α chain because its ring structure causes “kinks” in the peptide chain. [Note: The presence of proline dictates that the helical conformation of the α chain cannot be an α helix (see p. 16).] Glycine, the smallest amino acid, is found in every third position of the polypeptide chain. It fits into the restricted spaces where the three chains of the helix come together. The glycine residues are part of a repeating sequence, –Gly–X–Y–, where X is frequently proline, and Y is often hydroxyproline (but can be hydroxylysine, Figure 4.5). Thus, most of the α chain can be regarded as a polytripeptide whose sequence can be represented as (–Gly–Pro–Hyp–)333.
2. Triple-helical structure: Unlike most globular proteins that are folded into compact structures, collagen, a fibrous protein, has an elongated, triple-helical structure that is stabilized by interchain hydrogen bonds.
Figure 4.4 Electron micrograph of a polygonal network formed by association of collagen type IV monomers.

3. Hydroxyproline and hydroxylysine: Collagen contains hydroxyproline and hydroxylysine, which are not present in most other proteins. These residues result from the hydroxylation of some of the proline and lysine residues after their incorporation into polypeptide chains (Figure 4.6). The hydroxylation is, thus, an example of posttranslational modification (see p. 443). [Note: Generation of hydroxyproline maximizes formation of interchain hydrogen bonds that stabilize the triple-helical structure.]
4. Glycosylation: The hydroxyl group of the hydroxylysine residues of collagen may be enzymatically glycosylated. Most commonly, glucose and galactose are sequentially attached to the polypeptide chain prior to triple-helix formation (Figure 4.7).
Figure 4.5 Amino acid sequence of a portion of the α1 chain of collagen. [Note: Hyp is hydroxyproline, and Hyl is hydroxylysine.]
C. Biosynthesis
The polypeptide precursors of the collagen molecule are synthesized in fibroblasts (or in the related osteoblasts of bone and chondroblasts of cartilage). They are enzymically modified and form the triple helix, which gets secreted into the extracellular matrix. After additional enzymic modification, the mature extracellular collagen monomers aggregate and become cross-linked to form collagen fibers.
1. Formation of pro-α chains: Collagen is one of many proteins that normally function outside of cells. Like most proteins produced for export, the newly synthesized polypeptide precursors of α chains (prepro-α chains) contain a special amino acid sequence at their N-terminal ends. This sequence acts as a signal that, in the absence of additional signals, targets the polypeptide being synthesized for secretion from the cell. The signal sequence facilitates the binding of ribosomes to the rough endoplasmic reticulum (RER), and directs the passage of the prepro-α chain into the lumen of the RER. The signal sequence is rapidly cleaved in the RER to yield a precursor of collagen called a pro-α chain (see Figure 4.7).
Figure 4.6 Hydroxylation of proline residues of pro-α chains of collagen by prolyl hydroxylase.
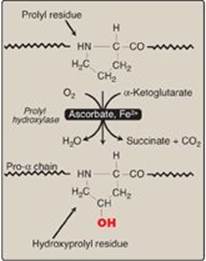
Figure 4.7 Synthesis of collagen. RER = rough endoplasmic reticulum; mRNA = messenger RNA. Synthesis of collagen.

2. Hydroxylation: The pro-α chains are processed by a number of enzymic steps within the lumen of the RER while the polypeptides are still being synthesized (see Figure 4.7). Proline and lysine residues found in the Y-position of the –Gly–X–Y– sequence can be hydroxylated to form hydroxyproline and hydroxylysine residues. These hydroxylation reactions require molecular oxygen, Fe2+, and the reducing agent vitamin C (ascorbic acid, see p. 377), without which the hydroxylating enzymes, prolyl hydroxylase and lysyl hydroxylase, are unable to function (see Figure 4.6). In the case of ascorbic acid deficiency (and, therefore, a lack of proline and lysine hydroxylation), interchain H-bond formation is impaired, as is formation of a stable triple helix. Additionally, collagen fibrils cannot be cross-linked (see below), greatly decreasing the tensile strength of the assembled fiber. The resulting deficiency disease is known as scurvy. Patients with ascorbic acid deficiency also often show bruises on the limbs as a result of subcutaneous extravasation (leakage) of blood due to capillary fragility (Figure 4.8).
3. Glycosylation: Some hydroxylysine residues are modified by glycosylation with glucose or glucosyl-galactose (see Figure 4.7).
4. Assembly and secretion: After hydroxylation and glycosylation, three pro-α chains form procollagen, a precursor of collagen that has a central region of triple helix flanked by the nonhelical amino- and carboxyl-terminal extensions called propeptides (see Figure 4.7). The formation of procollagen begins with formation of interchain disulfide bonds between the C-terminal extensions of the pro-α chains. This brings the three α chains into an alignment favorable for helix formation. The procollagen molecules move through the Golgi apparatus, where they are packaged in secretory vesicles. The vesicles fuse with the cell membrane, causing the release of procollagen molecules into the extracellular space.
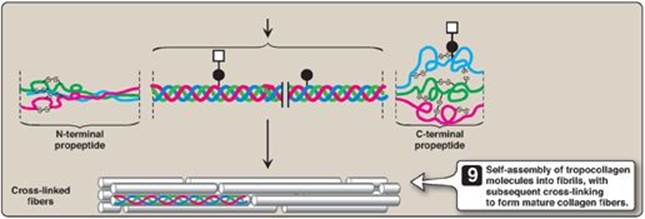
5. Extracellular cleavage of procollagen molecules: After their release, the procollagen molecules are cleaved by N- and C-procollagen peptidases, which remove the terminal propeptides, releasing triple-helical tropocollagen molecules.
Figure 4.8 The legs of a 46-year-old man with scurvy.

6. Formation of collagen fibrils: Tropocollagen molecules spontaneously associate to form collagen fibrils. They form an ordered, overlapping, parallel array, with adjacent collagen molecules arranged in a staggered pattern, each overlapping its neighbor by a length approximately three-quarters of a molecule (see Figure 4.7).
7. Cross-link formation: The fibrillar array of collagen molecules serves as a substrate for lysyl oxidase. This Cu2+-containing extracellular enzyme oxidatively deaminates some of the lysine and hydroxylysine residues in collagen. The reactive aldehydes that result (allysine and hydroxyallysine) can condense with lysine or hydroxylysine residues in neighboring collagen molecules to form covalent cross-links and, thus, mature collagen fibers (Figure 4.9).
Figure 4.9 Formation of cross-links in collagen. [Note: Lysyl oxidase is irreversibly inhibited by a toxin from plants in the genus Lathyrus, leading to a condition known as lathyrism.]
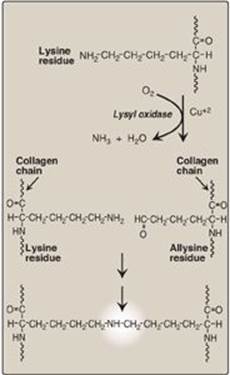
Lysyl oxidase is one of several copper-containing enzymes. Others include cytochrome oxidase (see p. 76), dopamine hydroxylase (see p. 286), superoxide dismutase (see p.148), and tyrosinase (see p. 273). Disruption in copper homeostasis causes copper deficiency (X-linked Menkes disease) or overload (Wilson disease).
D. Degradation
Normal collagens are highly stable molecules, having half-lives as long as several years. However, connective tissue is dynamic and is constantly being remodeled, often in response to growth or injury of the tissue. Breakdown of collagen fibers is dependent on the proteolytic action of collagenases, which are part of a large family of matrix metalloproteinases. For type I collagen, the cleavage site is specific, generating three-quarter and one-quarter length fragments. These fragments are further degraded by other matrix proteinases.
E. Collagen diseases: Collagenopathies
Defects in any one of the many steps in collagen fiber synthesis can result in a genetic disease involving an inability of collagen to form fibers properly and, therefore, an inability to provide tissues with the needed tensile strength normally provided by collagen. More than 1,000 mutations have been identified in 23 genes coding for 13 of the collagen types. The following are examples of diseases that are the result of defective collagen synthesis.
Figure 4.10 Stretchy skin of classic Ehlers-Danlos syndrome.

1. Ehlers-Danlos syndrome: Ehlers-Danlos syndrome (EDS) is a heterogeneous group of connective tissue disorders that result from inheritable defects in the metabolism of fibrillar collagen molecules. EDS can be caused by a deficiency of collagen-processing enzymes (for example, lysyl hydroxylase or N-procollagen peptidase) or from mutations in the amino acid sequences of collagen types I, III, or V. The classic form of EDS, caused by defects in type V collagen, is characterized by skin extensibility and fragility and joint hypermobility (Figure 4.10). The vascular form, due to defects in type III collagen, is the most serious form of EDS because it is associated with potentially lethal arterial rupture. [Note: The classic and vascular forms show autosomal dominant inheritance.] Collagen containing mutant chains may have altered structure, secretion, or distribution. It frequently is degraded. [Note: Incorporation of just one mutant chain may result in degradation of the triple helix. This is known as a dominant-negative effect.].
Figure 4.11 Lethal form (type II) of osteogenesis imperfecta in which the fractures appear in utero, as revealed by this radiograph of a stillborn fetus.

2. Osteogenesis imperfecta: This syndrome, known as brittle bone disease, is a genetic disorder of bone fragility characterized by bones that fracture easily, with minor or no trauma (Figure 4.11). Over 80% of cases of osteogenesis imperfecta (OI) are caused by dominant mutations to the genes that code for the α1 or α2 chains in type I collagen. The most common mutations cause the replacement of glycine (in –Gly–X–Y–) by amino acids with bulky side chains. The resultant structurally abnormal α chains prevent the formation of the required triple-helical conformation. Phenotypic severity ranges from mild to lethal. Type I OI, the most common form, is characterized by mild bone fragility, hearing loss, and blue sclerae. Type II, the most severe form, is typically lethal in the perinatal period as a result of pulmonary complications. In utero fractures are seen (see Figure 4.11). Type III is also a severe form. It is characterized by multiple fractures at birth, short stature, spinal curvature leading to a “humped-back” (kyphotic) appearance, and blue sclerae. Dentinogenesis imperfecta, a disorder of tooth development, may be seen in OI.
Figure 4.12 Desmosine cross-link in elastin.
III. ELASTIN
In contrast to collagen, which forms fibers that are tough and have high tensile strength, elastin is a connective tissue protein with rubber-like properties. Elastic fibers composed of elastin and glycoprotein microfibrils are found in the lungs, the walls of large arteries, and elastic ligaments. They can be stretched to several times their normal length but recoil to their original shape when the stretching force is relaxed.
A. Structure
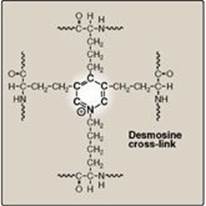
Elastin is an insoluble protein polymer synthesized from a precursor, tropoelastin, which is a linear polypeptide composed of about 700 amino acids that are primarily small and nonpolar (for example, glycine, alanine, and valine). Elastin is also rich in proline and lysine but contains scant hydroxyproline and hydroxylysine. Tropoelastin is secreted by the cell into the extracellular space. There, it interacts with specific glycoprotein microfibrils, such as fibrillin, which function as a scaffold onto which tropoelastin is deposited. Some of the lysyl side chains of the tropoelastin polypeptides are oxidatively deaminated by lysyl oxidase, forming allysine residues. Three of the allysyl side chains plus one unaltered lysyl side chain from the same or neighboring polypeptides form a desmosine cross-link (Figure 4.12). This produces elastin, an extensively interconnected, rubbery network that can stretch and bend in any direction when stressed, giving connective tissue elasticity (Figure 4.13). Mutations in the fibrillin-1 protein are responsible for Marfan syndrome, a connective tissue disorder characterized by impaired structural integrity in the skeleton, the eye, and the cardiovascular system. With this disease, abnormal fibrillin protein is incorporated into microfibrils along with normal fibrillin, inhibiting the formation of functional microfibrils. [Note: Patients with Marfan syndrome, OI, or EDS may have blue sclerae due to tissue thinning that allows underlying pigment to show through.]
Figure 4.13 Elastin fibers in relaxed and stretched conformations.

B. Role of α1-antitrypsin in elastin degradation
1. α1-Antitrypsin: Blood and other body fluids contain a protein, α1-antitrypsin (AAT or A1AT), which inhibits a number of proteolytic enzymes (called proteases or proteinases) that hydrolyze and destroy proteins. [Note: The inhibitor was originally named α1-antitrypsin because it inhibits the activity of trypsin, a proteolytic enzyme synthesized as trypsinogen by the pancreas (see p. 248).] AAT has the important physiologic role of inhibiting neutrophil elastase, a powerful protease that is released into the extracellular space and degrades elastin of alveolar walls as well as other structural proteins in a variety of tissues (Figure 4.14). Most of the AAT found in plasma is synthesized and secreted by the liver. AAT comprises more than 90% of the α1-globulin fraction of normal plasma. Extrahepatic synthesis occurs in monocytes and alveolar macrophages, and may be important in the prevention of local tissue injury by elastase.
2. Role of α1-antitrypsin in the lungs: In the normal lung, the alveoli are chronically exposed to low levels of neutrophil elastase released from activated and degenerating neutrophils. The proteolytic activity of elastase can destroy the elastin in alveolar walls if unopposed by the action of AAT, the most important inhibitor of neutrophil elastase (see Figure 4.14). Because lung tissue cannot regenerate, the destruction of the connective tissue of alveolar walls results in emphysema.
3. Emphysema resulting from α1-antitrypsin deficiency: In the United States, approximately 2%–5% of patients with emphysema are predisposed to the disease by inherited defects in AAT. A number of different mutations in the gene for AAT are known to cause a deficiency of the protein, but one single purine base mutation (GAG to AAG, resulting in the substitution of lysine for glutamic acid at position 342 of the protein) is clinically the most widespread. The mutation causes the normally monomeric AAT to polymerize within the endoplasmic reticulum of hepatocytes, resulting in decreased secretion of AAT by the liver. Consequently, blood levels of AAT are reduced, decreasing the amount that gets to the alveoli. The polymer that accumulates in the liver may result in cirrhosis (scarring of the liver). In the United States, the AAT mutation is most common in Caucasians of Northern European ancestry. An individual must inherit two abnormal AAT alleles to be at risk for the development of emphysema. In a heterozygote, with one normal and one defective gene, the levels of AAT are sufficient to protect the alveoli from damage. [Note: Methionine 358 in AAT is required for the binding of the inhibitor to its target proteases. Smoking causes the oxidation and subsequent inactivation of the methionine, thereby rendering the inhibitor powerless to neutralize elastase. Smokers with AAT deficiency, therefore, have a considerably elevated rate of lung destruction and a poorer survival rate than nonsmokers with the deficiency.] The deficiency of elastase inhibitor can be treated by weekly augmentation therapy, that is, intravenous administration of AAT. The AAT diffuses from the blood into the lung, where it reaches therapeutic levels in the fluid surrounding the lung epithelial cells.
Figure 4.14 Destruction of alveolar tissue by elastase released from neutrophils activated as part of the immune response to airborne pathogens.
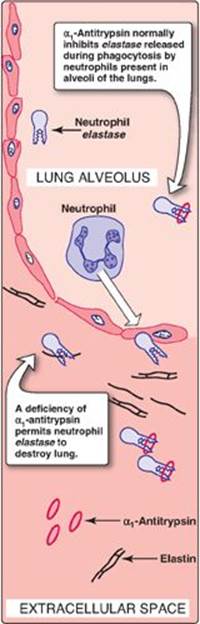
Figure 4.15 Key concept map for the fibrous proteins collagen and elastin.
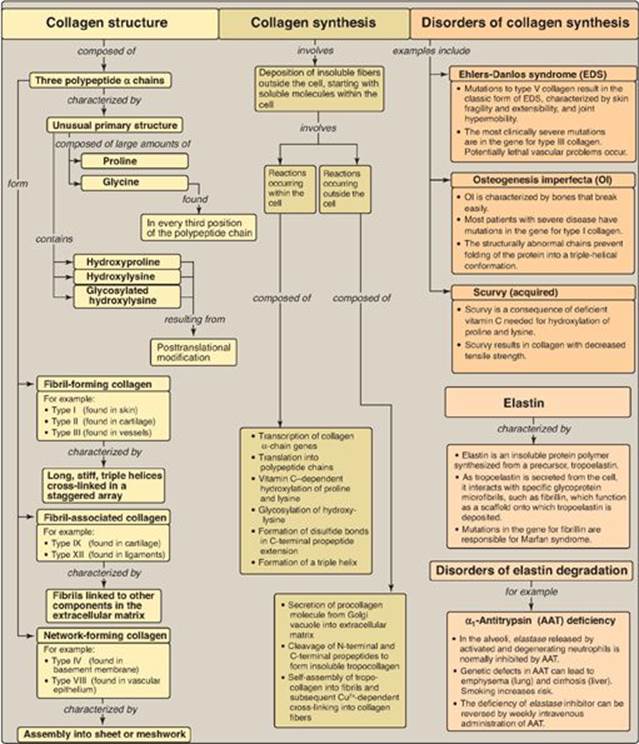
IV. CHAPTER SUMMARY
Collagen and elastin are fibrous proteins (Figure 4.15). Collagen molecules contain an abundance of proline, lysine, and glycine, the latter occurring at every third position in the primary structure. Collagen also contains hydroxyproline, hydroxylysine, and glycosylated hydroxylysine, each formed by posttranslational modification. Collagen molecules typically form fibrils containing a long, stiff, triple-stranded helical structure, in which three collagen polypeptide chains are wound around one another in a rope-like superhelix (triple helix). Other types of collagen form mesh-like networks. Elastin is a connective tissue protein with rubber-like properties in tissues such as the lung. α1-Antitrypsin (AAT), produced primarily by the liver but also by monocytes and alveolar macrophages, prevents elastase-catalyzed degradation of elastin in the alveolar walls. A deficiency of AAT can cause emphysema and, in some cases, cirrhosis of the liver.
Study Questions
Choose the ONE best answer.
4.1 A 30-year-old woman of Northern European ancestry presents with progressive dyspnea (shortness of breath). She denies the use of cigarettes. Family history reveals that her sister also has problems with her lungs. Which one of the following etiologies most likely explains this patient’s pulmonary symptoms?
A. Deficiency in dietary vitamin C
B. Deficiency of α1-antitrypsin
C. Deficiency of prolyl hydroxylase
D Decreased elastase activity
E. Increased collagenase activity
Correct answer = B. α1-Antitrypsin (AAT) deficiency is a genetic disorder that can cause pulmonary damage and emphysema even in the absence of cigarette use. A deficiency of AAT permits increased elastase activity to destroy elastin in the alveolar walls. AAT deficiency should be suspected when chronic obstructive pulmonary disease develops in a patient younger than age 45 years who does not have a history of chronic bronchitis or tobacco use or when multiple family members develop obstructive lung disease at an early age. Choices A, C, and E refer to collagen, not elastin.
4.2 What is the differential basis of the liver and lung pathology seen in α1-antitrypsin deficiency?
With α1-antitrypsin (AAT) deficiency, the cirrhosis that can result is due to polymerization and retention of AAT in the liver, its site of synthesis. The alveolar damage is due to the retention-based deficiency of AAT (a protease inhibitor) in the lung such that elastase (a protease) is unopposed.
4.3 A 7-month-old child “fell over” while crawling and now presents with a swollen leg. Imaging reveals a fracture of a bowed femur, secondary to minor trauma, and thin bones (see x-ray at right). Blue sclerae are also noted. At age 1 month, the infant had multiple fractures in various states of healing (right clavicle, right humerus, and right radius). A careful family history has ruled out nonaccidental trauma (child abuse) as a cause of the bone fractures. Which pairing of a defective (or deficient) molecule and the resulting pathology best fits this clinical description?

A. Elastin and emphysema
B. Fibrillin and Marfan disease
C. Type I collagen and osteogenesis imperfecta (OI)
D. Type V collagen and Ehlers-Danlos syndrome (EDS)
E. Vitamin C and scurvy
Correct answer = C. The child most likely has osteogenesis imperfecta. Most cases arise from a defect in the genes encoding type I collagen. Bones in affected patients are thin, osteoporotic, often bowed, and extremely prone to fracture. Pulmonary problems are not seen in this child. Individuals with Marfan syndrome have impaired structural integrity of the skeleton, eyes, and cardiovascular system. Defects in type V collagen cause the classic form of EDS characterized by skin extensibility and fragility and joint hypermobility. Vitamin C deficiency is characterized by capillary fragility.
4.4 How and why is proline hydroxylated in collagen?
Proline is hydroxlyated by prolyl hydroxylase, an enzyme of the rough endoplasmic reticulum that requires O2, Fe2+, and vitamin C. Hydroxylation increases interchain hydrogen bond formation, strengthening the triple helix of collagen. Vitamin C deficiency impairs hydroxylation.