Case Files Biochemistry, 3rd Edition (2015)
SECTION II. Clinical Cases
CASE 30
A 48-year-old man presents to the clinic because of concerns about heart disease. He reports that his father died from a heart attack at 46 years of age, and his older brother has also had a heart attack at 46 years of age but survived and is on medications for elevated cholesterol. The patient reports chest pain occasionally with ambulation around his house and is not able to climb stairs without significant chest pain and shortness of breath. The physical examination findings are normal, and the physician orders electrocardiography (ECG), an exercise stress test, and blood work. The patient’s cholesterol level comes back as 350 mg/dL (normal 200). The physician prescribes medication, which he states is directed at the rate-limiting step of cholesterol biosynthesis.
![]() What is the rate-limiting step of cholesterol metabolism?
What is the rate-limiting step of cholesterol metabolism?
![]() What is the class of medication prescribed?
What is the class of medication prescribed?
ANSWERS TO CASE 30:
Hypercholesterolemia
Summary: A 48-year-old man with strong family history of heart disease and now angina and exertional dyspnea presents with a significantly elevated cholesterol level. A medication is prescribed that is directed at the rate-limiting step of cholesterol biosynthesis.
• Rate-limiting step: The enzyme hydroxymethylglutaryl-CoA reductase (HMG-CoA reductase) catalyzes an early rate-limiting step in cholesterol biosynthesis.
• Likely medication: HMG-CoA reductase inhibitor, otherwise known as “statin” medications.
CLINICAL CORRELATION
Hyperlipidemia is one of the most treatable risk factors of atherosclerotic vascular disease. In particular, the level of the low-density lipoprotein (LDL) cholesterol correlates with the pathogenesis of atherosclerosis. Exercise, dietary adjustments, and weight loss are the initial therapy of hyperlipidemia. If these are not sufficient, then pharmacologic therapy is required. The exact LDL targets depend on the patient’s risk of cardiovascular disease. For example, if an individual has had a cardiovascular event previously (heart attack or stroke), then the LDL target is 100 mg/dL; 1 to 2 risk factors without prior events = 130 mg/dL; and no risk factors = 160 mg/dL.
APPROACH TO:
Lipid Metabolism
OBJECTIVES
1. Describe cholesterol metabolism.
2. Explain the role of serum lipoproteins.
3. List the types of hereditary hyperlipidemias.
4. Explain why the LDL cholesterol level is increased with familial hypercholesterolemia.
DEFINITIONS
APOLIPOPROTEIN: The protein component of a lipoprotein; in addition to being a structural component of a lipoprotein, apolipoproteins also serve as activators of enzymes and ligands for receptors.
CHYLOMICRON: A lipoprotein synthesized by the intestine to transport dietary lipids to peripheral tissues and the liver.
HDL: High-density lipoprotein; synthesized in the liver, the HDL serves as a source of apolipoproteins for other lipoproteins, as the site of action for the conversion of cholesterol to cholesterol ester in the plasma by the enzyme lecithin-cholesterol acyltransferase (LCAT), and delivers cholesterol esters derived from peripheral membranes to the liver. It is commonly called the “good cholesterol.”
LDL: Low-density lipoprotein; a product of the degradation of very-low-density lipoproteins (VLDLs) by the action of lipoprotein lipase. LDLs are taken up by a receptor-mediated endocytosis by both peripheral tissues and the liver. It is commonly called the “bad cholesterol.”
LIPOPROTEIN: A macromolecular particle composed of varying quantities of protein, triacylglycerol, phospholipids, cholesterol, and cholesterol esters. The lipoprotein structure has a phospholipid and free cholesterol skin surrounding a core composed of triacylglycerol and cholesterol esters, with the proteins imbedded on the surface. They serve as carriers of lipid in the circulation.
VLDL: Very-low-density lipoprotein; synthesized by the liver to transport triacylglycerol from the liver to peripheral tissues.
DISCUSSION
Although cholesterol can be synthesized in almost all cells, the liver, intestine, and the steroidogenic tissues such as the adrenal glands and reproductive tissues are the primary sites. In the liver, cholesterol is synthesized in the endoplasmic reticulum along with phospholipids, triacylglycerides, and apoproteins. Prelipoprotein particles are assembled in the endoplasmic reticulum and then transferred to the Golgi. Further processing and addition of cholesterol esters occur in the Golgi, culminating in the formation of secretory granules containing lipoprotein particles. These vesicles then fuse with the plasma membrane and export cholesterol from the cell via exocytosis in the form of VLDLs (see below), which then enter the circulation. As the lipoprotein complexes are transported through the bloodstream they are converted from VLDL to intermediate density lipoproteins (IDL) to LDL by the removal of triacylglycerides by lipoprotein lipase, which is located on the surface of capillary epithelial cells.
Cholesterol and triacylglycerides (TAGs) are transported as complexes in the form of lipoprotein particles. These lipoprotein particles contain a core of TAGs and cholesteryl esters surrounded by a monolayer of phospholipids, cholesterol, and specific proteins called apoproteins. The apoproteins, specific to each type of lipoprotein, enable the hydrophobic lipids to be transported in the aqueous environment of the bloodstream. They also contain signals that target the lipoprotein particles to the cells or activate enzymes. The lipoprotein particles vary in density depending on the lipid/protein ratio and are named based on these densities. The higher the lipid–protein ratio, the lower the density of the particle.
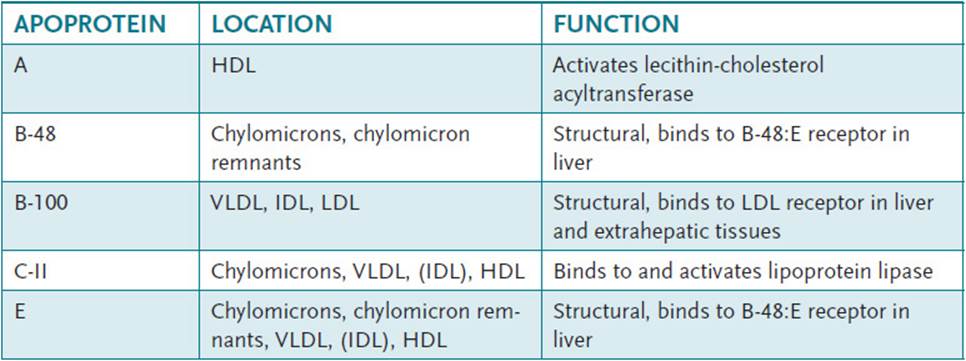
The major classes of lipoproteins (Table 30-1) and some of their properties are:
Table 30-1 • MAJOR APOPROTEINS INVOLVED IN LIPID TRANSPORT BY LIPOPROTEINS
• Chylomicrons
– Lowest density
– Transport dietary lipids from the intestine to target tissues
• VLDLs
– Produced by liver cells to transport endogenously synthesized lipids to target cells
– Production controlled by lipid availability
– Contain 5 different apoproteins
• IDLs
• LDLs
– Primarily cholesteryl esters
– Apoprotein B-100
• HDLs
– Secreted by liver and intestine
– Contains apoprotein A-1
– “Good cholesterol,” high levels associated with low incidence of atherosclerosis
The LDLs (containing cholesteryl esters) are taken up by cells by a process known as receptor-mediated endocytosis. The LDL receptor mediates this endocytosis and is important to cholesterol metabolism. LDLs bind to these receptors, which recognize apoprotein B-100. After LDL binding to the LDL receptor, the ligand-receptor complexes cluster on the plasma membrane in coated pits, which then invaginate, forming coated vesicles. These coated vesicles are internalized, and clathrin, the protein composing the lattice in membrane-coated pits, is removed. These vesicles are now called endosomes and these endosomes fuse with the lysosome. The LDL receptor–containing membrane buds off and is recycled to the plasma membrane. Fusion of the lysosome and endosome releases lysosomal proteases that degrade the apoproteins into amino acids. Lysosomal enzymes also hydrolyze the cholesteryl esters to free cholesterol and fatty acids. The free cholesterol is released into the cytoplasm of the cell, and this free cholesterol is then available to be used by the cell. Excess cholesterol is reesterified by acyl-CoA:cholesterol acyltransferase (ACAT), which uses fatty acyl-CoA as the source of activated fatty acid. Free cholesterol affects cholesterol metabolism by inhibiting cholesterol biosynthesis. Cholesterol inhibits the enzyme β-hydroxy-β-methylglutaryl-CoA reductase (HMG-CoA reductase), which catalyzes an early rate-limiting step in cholesterol biosynthesis. HMG-CoA reductase is the target of the statin drugs in wide use for treating patients with elevated cholesterol levels. In addition, free cholesterol inhibits the synthesis of the LDL receptor, thus limiting the amount of LDLs that are taken up by the cell.
Hyperlipidemia is defined as elevated lipoprotein levels in the plasma, which may be primary or secondary. Several different types of hereditary hyperlipidemias have been defined.
• Type 1: A relatively rare inherited deficiency of either lipoprotein lipase activity or the lipoprotein lipase-activating protein apo C-II. This results in the inability to effectively remove chylomicrons and VLDL triglycerides from the blood.
• Type 2: Includes familial hypercholesterolemia described in detail below.
• Type 3: Associated with abnormalities of apolipoprotein E (apo E) and defective conversion and removal of VLDL from the plasma.
• Type 4: A common disorder characterized by variable elevations of plasma triglycerides contained predominantly in VLDL. This leads to a possible predisposition to atherosclerosis and often has a familial distribution.
• Type 5: An uncommon disorder, sometimes familial, associated with defective clearance of exogenous and endogenous triglycerides and the risk of life-threatening pancreatitis.
The disease familial hypercholesterolemia results from a mutation in the LDL-receptor gene found on chromosome 19. The overall phenotype of the inability to internalize the LDL receptor can be caused by 3 different types of defects. In the first type, the LDL receptor is not produced. The second type is a result of a mutation in the terminal region of the receptor that results in an LDL receptor unable to bind LDL. The third type is caused by a mutation in the C-terminal region that prevents the LDL-receptor complex from undergoing endocytosis. In the absence of a functioning LDL receptor, LDL cholesterol levels are greatly elevated in individuals with this disease. This elevation results in premature atherosclerosis of the coronary arteries. Genetic defects in apoprotein B-100, the protein in the LDL recognized by the LDL receptor, also exist and lead to elevated LDL because the LDL complex is not recognized by the LDL receptor. A diet low in fat and cholesterol, an exercise regimen, and anticholesterol medications are used in the treatment of this disease.
COMPREHENSION QUESTIONS
30.1 A patient presents in your office with very high levels of serum cholesterol. After a series of tests, you conclude that the patient has high circulating levels of LDL cholesterol, but has normal levels of the liver LDL receptor. One possible explanation for this observation is which of the following?
A. The patient has a mutated form of apoprotein B-100
B. The inability to selectively remove cholesterol from the LDL complex
C. The absence of the enzyme lipoprotein lipase
D. Decreased levels of acyl-CoA: cholesterol acyltransferase
E. Altered phosphorylation of the LDL receptor
30.2 A patient with hereditary type 1 hyperlipidemia presents with elevated levels of chylomicrons and VLDL triglycerides in the blood. The main function of the chylomicrons in circulation is to do which of the following?
A. Transport lipids from the liver
B. Transport dietary lipids from the intestine to target tissues
C. Transport cholesterol from IDL to LDL
D. Act as a receptor for triacylglycerols in the liver
E. Bind cholesterol esters exclusively
30.3 Free cholesterol can affect cholesterol metabolism in the body by inhibiting cholesterol biosynthesis. The step at which free cholesterol inhibits its biosynthesis is by inhibiting which of the following processes?
A. Cyclizing of squalene to form lanosterol
B. Reduction of 7-dehydrocholesterol to form cholesterol
C. Formation of mevalonate from hydroxymethylglutaryl-CoA
D. Kinase that phosphorylates hydroxymethylglutaryl-CoA reductase
E. Condensation of acetyl-CoA and acetoacetyl-CoA to form hydroxymethylglutaryl-CoA
30.4 A patient presents in your office with very high levels of serum cholesterol. He states that he has tried to follow the diet and exercise regimen you gave him last year. You decide that this patient would benefit from a drug such as atorvastatin. This class of drugs is effective in treating hypercholesterolemia because it has what effect?
A. Stimulates phosphorylation of the β-hydroxy-β-methylglutaryl-CoA reductase enzyme
B. Decreases the stability of the β-hydroxy-β-methylglutaryl-CoA reductase protein
C. Binds cholesterol preventing it from being absorbed by the intestine
D. Directly prevents the deposition of cholesterol on artery walls
E. Inhibits the enzyme β-hydroxy-β-methylglutaryl-CoA reductase
ANSWERS
30.1 A. A common genetic mutation leading to high-circulating LDL cholesterol levels is caused by mutations in the LDL receptor. The lack of a functional receptor prevents the removal of LDL cholesterol from circulation. Apoprotein B-100 is found in the LDL-cholesterol complex and is the protein recognized by the LDL receptor. In this patient, the LDL receptor is normal so it is reasonable to conclude that the reason that the LDL cholesterol remains in circulation is because it is not recognized by the normal LDL receptor. A mutation in the apoprotein B-100 such that it is not recognized by the receptor would lead to elevated LDL-cholesterol levels.
30.2 B. The liver and intestine are the main sources of circulating lipids. Chylomicrons carry triacylglycerides and cholesterol esters from the intestine to other target tissues. VLDLs carry lipids from the liver into circulation. Lipoproteins are a mix of lipids and specific proteins and these complexes are classified based on their lipid–protein ratio. Lipoprotein lipases degrade the triacylglycerides in the chylomicrons and VLDLs with a concurrent release of apoproteins. This is a gradual process that converts the VLDLs into IDLs and then LDLs.
30.3 C. The major regulatory enzyme of cholesterol metabolism, β-hydroxy-β-methylglutaryl-CoA reductase, is regulated by 3 distinct mechanisms. The first is phosphorylation by a cAMP-dependent protein kinase. Phosphorylation of β-hydroxy-β-methylglutaryl-CoA reductase inactivates the enzyme. The other 2 mechanisms involve the levels of cholesterol. The degradation of the enzyme is controlled by cholesterol levels. The half-life of β-hydroxy-β-methylglutaryl-CoA reductase is regulated by cholesterol levels with high concentrations of cholesterol leading to a shorter half-life. The final regulatory mechanism involves control of the expression of the β-hydroxy-β-methylglutaryl-CoA reductase gene. High levels of cholesterol lead to a decrease in the mRNA levels coding for β-hydroxy-β-methylglutaryl-CoA reductase.
30.4 E. The statin class of drugs—atorvastatin, lovastatin, and simvastatin—is used to treat hypercholesterolemia. This class of drugs lowers cholesterol levels by inhibiting the biosynthesis of cholesterol. Specifically, these drugs inhibit the enzyme β-hydroxy-β-methylglutaryl-CoA (HMG-CoA) reductase, which catalyzes the reaction that converts HMG-CoA to mevalonate. This is the rate-limiting step of cholesterol biosynthesis.
In addition to the statin drugs, which inhibit HMG-CoA reductase, numerous other drugs are used to lower cholesterol levels. The first are resins, which are also referred to as bile acid sequestrants such as cholestyramine. The resins work by binding to the bile acids followed by excretion of the resin–bile complex. To make up for the loss of the bile acids the body converts cholesterol into bile acids, thus reducing the cholesterol levels.
Another type of drug used is the fibrates such as gemfibrozil. These compounds work by lowering the levels of triglycerides and increasing the levels of the “good” HDLs. Niacin is also effective in lowering cholesterol levels when used in large doses (more than that required for niacin as a vitamin). Niacin acts to lower levels of triglycerides and LDLs and increasing the levels of the “good” HDLs.
Drugs, such as ezetimibe, which inhibits the absorption of cholesterol in the intestine, are effective in lowering cholesterol levels. This drug is often given in combination with a statin and this combination therapy is very effective in lowering cholesterol levels.
BIOCHEMISTRY PEARLS
![]() Cholesterol can be synthesized in almost all cells, but the liver, intestine, and steroidogenic tissues, such as the adrenal glands and reproductive tissues, are the primary sites.
Cholesterol can be synthesized in almost all cells, but the liver, intestine, and steroidogenic tissues, such as the adrenal glands and reproductive tissues, are the primary sites.
![]() The major classes of lipoproteins are chylomicrons (lowest density), VLDLs, IDLs, LDLs, and HDLs (considered the “good cholesterol”).
The major classes of lipoproteins are chylomicrons (lowest density), VLDLs, IDLs, LDLs, and HDLs (considered the “good cholesterol”).
![]() Familial hyperlipidemia is subdivided into 5 types, with type 5 being most common, characterized by variable elevations of plasma triglycerides contained predominantly in VLDL.
Familial hyperlipidemia is subdivided into 5 types, with type 5 being most common, characterized by variable elevations of plasma triglycerides contained predominantly in VLDL.
![]() The rate-limiting step in cholesterol biosynthesis is the enzyme HMG-CoA reductase, which is the target of the statin drugs.
The rate-limiting step in cholesterol biosynthesis is the enzyme HMG-CoA reductase, which is the target of the statin drugs.
REFERENCES
Berg JM, Tymoczko JL, Stryer L. Biochemistry. 5th ed. New York: Freeman; 2002:722-731.
Devlin TM, ed. Textbook of Biochemistry with Clinical Correlations. 7th ed. New York: Wiley-Liss; 2010.