Case Files Biochemistry, 3rd Edition (2015)
SECTION II. Clinical Cases
CASE 49
A 36-year-old man presents to the clinic with concerns about increasing weakness and fatigue. He reports that his symptoms are present at all times, but at times of stress, the weakness is much worse. He has had some nausea, vomiting, and nonspecific abdominal pain, resulting in involuntary weight loss. His skin coloration has changed similar to a tan and is all over his body. On exam, he is in no distress with normal vitals other than a slightly low blood pressure. His skin is bronze in color with darkening in elbows and creases of the hand, although he states that he avoids the sun. The remainder of the examination is normal.
![]() What is the likely diagnosis?
What is the likely diagnosis?
![]() What is the underlying molecular disorder?
What is the underlying molecular disorder?
ANSWERS TO CASE 49:
Addison Disease
Summary: A 36-year-old man presents with fatigue, weakness, nonspecific gastrointestinal symptoms, hypotension, and darkening skin coloration despite being away from sunlight.
• Diagnosis: Addison disease
• Underlying problem: Adrenal insufficiency with lack of mineralocorticoids and cortisol
CLINICAL CORRELATION
This 36-year-old man has the clinical stigmata of Addison disease, or adrenocorticoid deficiency. Symptoms of weakness, fatigue, and hypotension are caused by decreased levels of cortisol as well as mineralocorticoids. The darkening of the skin is a result of increased melanocyte-stimulating hormone, metabolized from adrenocorticotropin hormone (ACTH), which is elevated because of the low levels of the adrenal hormones. This is a potentially fatal disorder and requires prompt clinical recognition. Serum electrolytes give a clue to the disorder, because the patient would likely have hyponatremia and hyperkalemia. An ACTH stimulation test revealing low levels of adrenal corticoid response is confirmatory. The treatment includes hydrocortisone (cortisol) to replace glucocorticoid deficiency and a mineralocorticoid supplementation. The most common cause of adrenal insufficiency on a chronic basis is autoimmune destruction of the adrenal gland. Other autoimmune diseases should be sought and tested for, such as diabetes mellitus and systemic lupus erythematosus. Adrenal insufficiency may occur acutely when the adrenal gland is not able to generate high levels of steroids in times of stress, such as surgery or infection; the most common reason in these cases is chronic corticosteroid therapy leading to relative adrenal suppression. These situations can be avoided by the administration of a “stress dose” hydrocortisone intravenously around the time of anticipated physiologic stress.
APPROACH TO:
Adrenal Hormones
OBJECTIVES
1. Describe the clinical manifestations of mineralocorticoid deficiency.
2. Describe the regulation of ACTH and cortisol.
DEFINITIONS
α-MELANOCYTE-STIMULATING HORMONE (α-MSH): A polypeptide hormone derived from the breakdown of ACTH (the N-terminal 13-amino acid residues). Released from the anterior pituitary, it acts on skin cells to cause skin darkening by the dispersion of melanin.
ACTH: Adrenocorticotropin, adrenocorticotropic hormone; a polypeptide hormone released from the anterior pituitary into the bloodstream in response to the binding of corticotropin-releasing hormone (CRH). ACTH binds to receptors in the adrenal cortex, causing the synthesis and release of cortisol.
CRH: Corticotropin-releasing hormone; a polypeptide hormone consisting of 41 amino acids that is released from the hypothalamus and travels to the adrenal cortex in a closed portal system. It binds to receptors in the adrenal cortex causing the release of ACTH and β-lipotropin.
CORTISOL: Hydrocortisone; a glucocorticoid steroid hormone synthesized by the adrenal gland in response to binding of ACTH. Cortisol binds to cytosolic or nuclear receptors that act as transcription factors for glucocorticoid-responsive genes. In general, cortisol is a catabolic hormone that promotes the breakdown of proteins.
CORTICOSTEROID: A class of steroid hormones that include the glucocorticoids (eg, cortisol) and mineralocorticoids (eg, aldosterone). Glucocorticoids are involved in the maintenance of normal blood glucose levels, whereas mineralocorticoids are involved in mineral balance.
HYPOADRENOCORTICISM: A failure of the adrenal cortex to produce glucocorticoid (and in some cases mineralocorticoid) hormones.
PROOPIOMELANOCORTIN: A precursor protein synthesized in the anterior pituitary from which are generated several polypeptide hormones. It gives rise to ACTH, β-lipotropin, γ-lipotropin, α-MSH, γ-MSH, corticotropin-like intermediary peptide (CLIP), and β-endorphin (and potentially enkephalins and β-MSH).
DISCUSSION
Cortisol is a member of the glucocorticoid steroid hormone family. It acts on almost every organ and tissue in the body in carrying out its vital role in the body’s response to stress. Among its crucial functions, it helps maintain blood pressure and cardiovascular function; acts as an antiinflammatory; modulates insulin effects on glucose utilization; and regulates metabolism of protein, carbohydrates, and lipids. In all of its actions, cortisol interacts with intracellular receptors to trigger their binding to specific response elements in the promoters of target genes to influence transcription of their messenger RNAs.
Cortisol is produced by the adrenal gland under the precise control of the hypothalamus and pituitary. The hypothalamus secretes CRH in response to stress. CRH acts on plasma membrane receptors in corticotrophic cells in the anterior pituitary to stimulate their release of ACTH. Secretion is also under circadian regulation. Vasopressin and angiotensin II augment this positive response but by themselves do not initiate it. ACTH is derived from the precursor polypeptide proopiomelanocortin after cleavage in the pituitary to release ACTH plus β-lipotropin, an endorphin precursor with melanocyte-stimulating activity. ACTH binds to plasma membrane receptors in the adrenal gland to stimulate production of cortisol, a signaling response mediated by adenylate cyclase (Figure 49-1). Increased blood cortisol levels exert feedback inhibition of ACTH secretion, a feedback loop acting at multiple levels including the hypothalamus, the pituitary and the central nervous system. Under separate positive control by norepinephrine, the intermediate pituitary converts ACTH to melanocyte-stimulating hormone (β-MSH) plus CLIP.
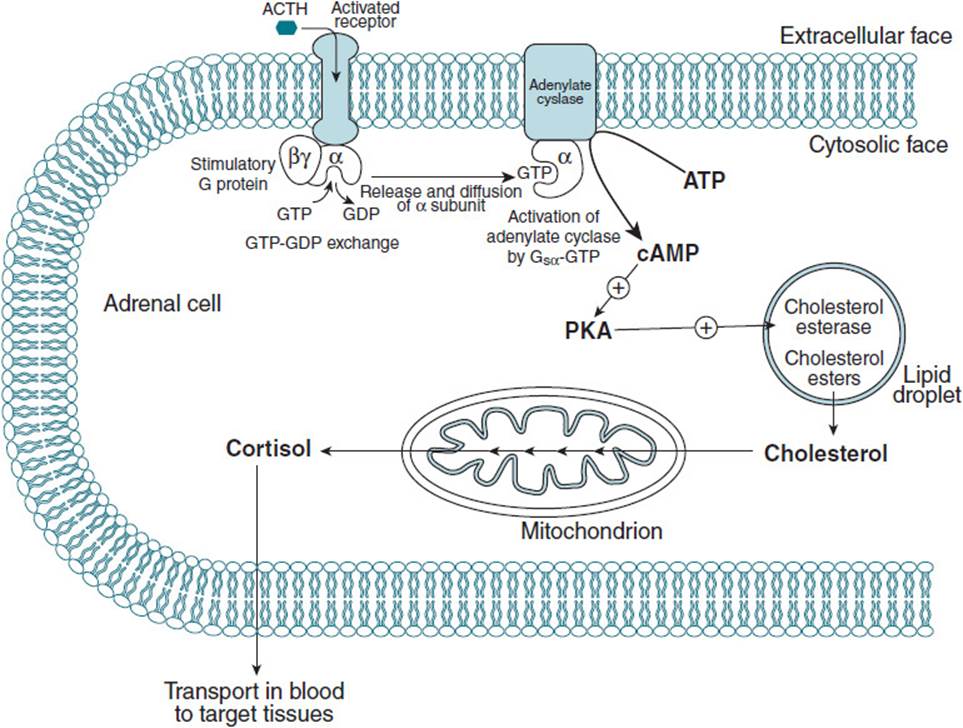
Figure 49-1. The sequence of events leading to the release of cortisol from the adrenal gland. Binding of ACTH to cell surface receptors activates adenylate cyclase to produce cAMP, which in turn activates protein kinase A. This causes phosphorylation events to occur that cause cholesterol to be released from cholesterol ester droplets in the cell. This initiates the conversion of cholesterol to cortisol, which is then released into the bloodstream.
Most cases of Addison disease are a result of idiopathic atrophy of the adrenal cortex induced by autoimmune responses, although a number of other causes of adrenal cortex destruction have been described. Hypoadrenocorticism results in decreased production of cortisol and, in some cases, also results in decreased production of aldosterone, the other principal steroid hormone produced by this gland. If aldosterone levels are insufficient, characteristic electrolyte abnormalities are evident owing to increased excretion of Na+ and decreased excretion of K+ chiefly in urine but also in sweat, saliva, and the GI tract. This condition leads to isotonic urine and decreased blood levels of Na+ and Cl− with increased levels of K+. Left untreated, aldosterone insufficiency produces severe dehydration, plasma hypertonicity, acidosis, decreased circulatory volume, hypotension, and circulatory collapse.
Cortisol deficiency impacts carbohydrate, fat, and protein metabolism and produces severe insulin sensitivity. Gluconeogenesis and liver glycogen formation are impaired, and hypoglycemia results. As a consequence, hypotension, muscle weakness, fatigue, vulnerability to infection, and stress are early symptoms. A characteristic hyperpigmentation on both exposed and unexposed parts of the body is evident. Decreased blood levels of cortisol in Addison disease lead to increased blood levels of both ACTH and β-lipotropin reflecting decreased feedback inhibition by cortisol of their synthesis. β-Lipotropin has melanocyte-stimulating activity accounting for the increased pigmentation. The disease is progressive, with the risk of a potentially fatal adrenal crisis triggered by infection or other trauma.
Secondary adrenal insufficiency may result from lesions in the hypothalamus or pituitary, leading to impaired release of ACTH. This condition does not exhibit hyperpigmentation because release of feedback inhibition of ACTH production by low cortisol levels cannot overcome the primary defect in ACTH production. Usually, aldosterone secretion is normal.
By contrast, Cushing syndrome results from cortisol overproduction and most commonly is caused by a tumor in either the adrenal gland or pituitary.
COMPREHENSION QUESTIONS
49.1 A 29-year-old woman exhibited a rounded face, hirsutism, upper body obesity, easily bruised skin, severe fatigue, muscle weakness, and anxiety. She also complained of irregular periods. As a woman with long-term asthma, she had been prescribed prednisone for the last 2 years. Findings on examination revealed high fasting blood glucose levels and high blood pressure. Cortisol levels were below normal.
Which one of the following is the most likely explanation to account for the patient’s symptoms?
A. Decreased levels of insulin
B. Increased levels of testosterone
C. Decreased secretion of ACTH
D. Excess exogenous glucocorticoid hormone
E. Increased hepatic metabolism of steroid hormones
49.2 A patient suffering from weakness, fatigue, nausea, and vomiting was found to have low blood concentrations of Na+ and Cl− and high levels of serum K+. Physical examination revealed a deep tanning of both exposed and unexposed parts of the body and dark pigmentation inside the mouth. The hyperpigmentation in this patient most likely resulted from which of the following?
A. Increased secretion of ACTH
B. Prolonged exposure of the patient to ultraviolet radiation
C. Excessive ingestion of β-carotene–containing foods
D. Activation of melanocytes caused by medication adverse events
E. Inhibition of plasma membrane Na+, K+-ATPase
49.3 Metyrapone is used to block the mitochondrial 11β-hydroxylase in the corticosteroid synthetic pathway and is administered to evaluate hypothalamic-pituitary-adrenal axis function. Which of the following results is most likely from this overnight diagnostic test in a healthy individual?
A. Feedback inhibition of cortisol biosynthesis
B. Increase in the levels of cortisol precursors
C. Decrease in ACTH levels
D. Inhibition of adenylate cyclase activity in adrenal cortical cells
E. Inhibition of pituitary function
ANSWERS
49.1 D. Prednisone acts as a glucocorticoid hormone analog, giving rise to Cushing syndrome symptoms after prolonged administration.
49.2 A. Hyperpigmentation is a feature of Addison disease, the diagnosis in this case. Decreased plasma cortisol because of adrenal insufficiency releases feedback inhibition of ACTH secretion by the pituitary, resulting in elevation of ACTH biosynthesis. The ACTH precursor peptide is cleaved to also yield MSH, the factor responsible for hyperpigmentation even in areas not exposed to sunlight.
49.3 B. Inhibition of this step in cortisol biosynthesis relieves feedback inhibition of its biosynthetic enzymes, leading to accumulation of cortisol precursors, particularly 11-deoxycortisol. Normal patients will also have a compensatory increase in the secretion of ACTH.
BIOCHEMISTRY PEARLS
![]() Most cases of Addison disease are because of idiopathic atrophy of the adrenal cortex induced by autoimmune responses.
Most cases of Addison disease are because of idiopathic atrophy of the adrenal cortex induced by autoimmune responses.
![]() Cortisol interacts with intracellular receptors to trigger their binding to specific response elements in the promoters of target genes to influence transcription of their messenger RNAs.
Cortisol interacts with intracellular receptors to trigger their binding to specific response elements in the promoters of target genes to influence transcription of their messenger RNAs.
![]() Under separate positive control by norepinephrine, the intermediate pituitary converts ACTH to MSH, which accounts for the “well tanned” appearance.
Under separate positive control by norepinephrine, the intermediate pituitary converts ACTH to MSH, which accounts for the “well tanned” appearance.
![]() Aldosterone insufficiency produces severe dehydration, plasma hypertonicity, acidosis, decreased circulatory volume, hypotension, and circulatory collapse.
Aldosterone insufficiency produces severe dehydration, plasma hypertonicity, acidosis, decreased circulatory volume, hypotension, and circulatory collapse.
REFERENCES
Bowen RA, Austgen L, Rouge M. Pathophysiology of the Endocrine System. Colorado State University, 2006. http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/.
Litwack G, Schmidt TJ. Biochemistry of hormones I: polypeptide hormones. In: Devlin TM, ed. Textbook of Biochemistry with Clinical Correlations. 7th ed. New York: Wiley-Liss; 2010.