CONCEPTS IN BIOLOGY
PART VI. PHYSIOLOGICAL PROCESSES
26. The Body's Control Mechanisms and Immunity
26.7. The Body's Defense Mechanisms—Immunity
Immunity is the body’s ability to maintain homeostasis by resisting or defending against potentially harmful agents, including microbes, toxins, and abnormal cells, such as cancer cells. The body’s immune system comprises specialized cells and messenger molecules, that work together to defend against infection and disease. Immune responses can be divided into two general categories: innate immune mechanisms and adaptive immune mechanisms. Innate immune mechanisms (also known as nonspecific immune mechanisms) are generic and protect the body against many kinds of agents. They are present and function from birth. Adaptive immune mechanisms (also known as specific immune mechanisms) are able to identify specific pathogens based on their exact chemical makeup. They are not present at birth and require exposure to a harmful agent to be activated. Once activated, adaptive immune mechanisms use specific combinations of chemicals and cells to destroy a specific enemy. Adaptive immune mechanisms also involve cellular memory, which allows the body to mount a rapid response to an enemy it has encountered previously.
Innate Immunity
The body has three kinds of innate defenses—physical barriers, protective chemicals, and certain kinds of defensive cells. All three may work together to safeguard the body.
Physical barriers are extremely important in protecting the body. For example, the skin and mucous membranes are barriers that prevent most bacteria, viruses, parasitic worms, and large toxic molecules from getting through and causing harm. The cells of the upper respiratory system are ciliated and covered with mucus. Should bacteria or dust particles be caught in the fluid, the cilia’s upward beating moves them toward the mouth and nose, where they can be eliminated by sneezing, coughing, or swallowing. If the threatening agent is swallowed, stomach acid (about pH 2) also acts as an innate defense. A mixture of materials with a low pH forms a protective barrier in the vagina.
Protective chemicals are produced by several kinds of cells and are involved in various ways in destroying pathogens. The enzyme lysozyme, found in sweat, tears, mucus, saliva, breast milk, and gastric secretions, destroys the cell walls of bacteria. Complement is a group of proteins primarily manufactured in the liver that circulate in the blood and help other systems defend against threats of cellular pathogens, such as bacteria, fungi, and protozoa. Complement proteins can help form holes in pathogens, allowing their content to leak out. Interferons are proteins that attach to the surface of cells and cause the cells to interfere with the ability of viruses to replicate. If a cell becomes infected with a virus, it produces interferons, which help control the virus in the cell but also act as messengers. These are sent to nearby cells, preparing them to produce their own interferons and initiate reactions that will inhibit viral replication should the virus arrive.
Many kinds of cells are involved in innate immunity. Various kinds of white blood cells recognize pathogens and communicate to other cells that there is a problem. Other white blood cells respond by producing and releasing a variety of chemicals. These chemicals can recruit other defensive cells to the site of injury or infection, kill pathogens directly, cause dilation of blood vessels, or perform other defensive functions. Certain white blood cells actively attack pathogens and kill them. Others engulf pathogens and the body cells that have been killed by infection. This pattern of interaction at the site of an infection is commonly called Inflammation. Inflammation is a pattern of events that leads to increased temperature, redness, swelling, and pain in the affected area. Because of the pain and swelling associated with inflammation, most people don’t think of it as a good thing. However, it is an important part of the innate immune response.

Inflammation also occurs when tissue cells are damaged even though there may not be pathogens present. If you hit your thumb with a hammer or are stung by a bee, inflammation occurs because damaged tissue cells release chemicals that initiate inflammation. The events that occur during inflammation are summarized in table 26.2.
TABLE 26.2. Inflammation
What You Observe |
What's Really Happening |
The event that triggers inflammation |
Damage to tissue by molecules, microbes, or other materials; for example, a scratch, infecting bacteria releasing toxins, a splinter. |
General events of inflammation |
Inflammatory chemicals released by injured cells and immune system cells serve as signals calling neutrophils from nearby capillaries. White blood cells (lymphocytes, monocytes, macrophages) go through the blood vessel walls and move to the damaged area, where they attack the enemy and clean up damaged cells by phagocytosis. The pH of tissue fluid decreases, helping control pathogens. |
Increased temperature |
Inflammatory chemicals such as histamine cause dilation (an increase in the diameter) of capillaries which causes increased flow of warm blood to the area. |
Swelling |
As capillaries dilate, they also become more porous, allowing fluid and white blood cells to move from the vessel into the tissue. |
Redness |
Inflammatory chemicals cause increased blood flow in the area. |
Pain |
Inflammatory chemicals and the pressure caused by swelling affect nerve endings. |
Under certain circumstances, the inflammatory process can get out of hand. If inflammation continues unchecked, the process can result in tissue damage. Under such circumstances, anti-inflammatory medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can be used to interfere with the inflammatory process. Aspirin, ibuprofen, ketoprofen, and naproxen are all over-the-counter NSAIDs.
Adaptive Immunity
Adaptive immune mechanisms are targeted at specific pathogens. Although a person is born with an immune system with the ability to develop adaptive immunity, these defenses must be “turned on” in order to work. To be “turned on,” the body must be exposed to an antigen associated with the pathogen. An antigen is a large organic molecule, usually a protein, that is recognized by cells of the immune system, which stimulate them to begin a series of events that result in the destruction of that specific antigen-bearing agent. Antigens can be individual molecules, such as botulism toxin. They can also be parts of cells, such as molecules found on the surface or inside bacteria, viruses, or eukaryotic cells. Furthermore, with adaptive immunity, the immune system cells remember the antigen and can react quickly to the pathogen if the body encounters the pathogen again. This mechanism is often called acquired immunity because it begins to work only after certain cells of the immune system have come into contact with a specific antigen. The cells that respond to antigens are primarily T-lymphocytes and B-lymphocytes. The way each of these cells responds is very different, so adaptive immune mechanisms are subdivided into B-cell or antibody-mediated immunity and T-cell or cell-mediated immunity. However, a great deal of interaction between these two cell types must occur to defend a person against a specific enemy.
B-Cells and Antibody-Mediated Immunity
B-lymphocytes (B-cells) are produced and mature in the bone marrow. They are hard to find in the blood but are found in large numbers in the lymph nodes and spleen. When a B-cell contacts an antigen, chemical messengers are sent from the cell surface to its nucleus and genes are activated. In these B-cells, certain portions of the DNA are cut and spliced to produce a new nucleotide sequence. This new gene causes the synthesis of a specific protein able to combine with that antigen. These protein molecules are called immunoglobulins or antibodies. An antibody is a protein made by the B-cells in response to an antigen (figure 26.22). There are five classes of antibodies, differing in their structures and functions (table 26.3).
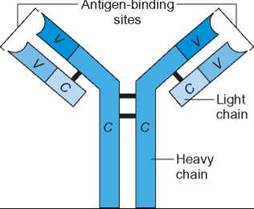
FIGURE 26.22. Structure of an Immunoglobulin Gamma (IgG) Antibody
An IgG antibody contains two heavy (long) polypeptide chains and two light (short) chains arranged so that there are two “variable regions” at the top of the Y-shaped molecule. This is where the antigen combines with the antibody (V = variable region, C = constant region).
TABLE 26.3. Classes of Antibodies
Class |
Location |
Function |
Immunoglobulin gamma (IgG) (also called gamma globulin) |
Blood and tissue fluids |
1. Most abundant immunoglobulin in the blood 2. Binds with free antigens or those on cell surfaces 3. Activates complement proteins to destroy pathogens 4. Encourages phagocytosis of pathogens 5. The only class that passes to the fetus through the placenta, which gives passive immunity to fetus |
Immunoglobulin mu (IgM) |
Blood |
1. The first immunoglobulin produced after B-cell encounters antigen 2. Activates complement 3. Causes pathogen cells to clump, encouraging phagocytosis |
Immunoglobulin alpha (IgA) |
Blood, mucus, saliva, tears, breast milk |
1. Produced in huge quantities on mucous membranes of the digestive, urogenital, and respiratory systems 2. Prevents pathogens from attaching to the surface of cells |
Immunoglobulin delta (IgD) |
Blood |
1. Found on surface of B-cells 2. Probably involved in development and activation of B-cells |
Immunoglobulin epsilon (IgE) |
Blood—attached to basophils |
1. Protects against parasitic worm infections 2. Binds to allergens and causes release of histamine from basophils; therefore, responsible for many allergic reactions, such as asthma and hay fever |
When B-cells become specialized for the production of a specific antibody, they remain specialized for the rest of their lives. These specialized B-cells undergo mitosis, and their descendents become either plasma cells, which produce antibodies, or memory B-cells. Plasma cells produce large quantities of antibodies, which enter the circulatory system. When an antibody molecule contacts the antigen, they combine. Figure 26.23 summarizes these events. If the antigen is an isolated toxin molecule or a virus, it is prevented from causing harm or neutralized. If the antigen is part of a pathogen, the antigen-antibody combination along with other molecules such as complement, causes holes to be formed in the cell, killing the pathogen. The antigen-antibody combination can also act as an attractant for phagocytes, such as macrophages and neutrophils, causing them to engulf and destroy the pathogen.
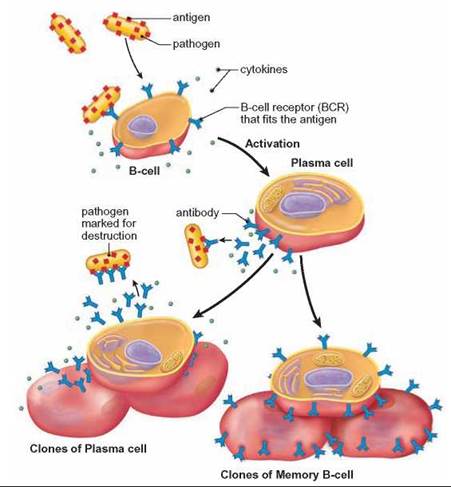
FIGURE 26.23. B-cells and Production of Antibodies
When a B-cell first encounters an antigen, it is triggered to express genes that produce antibodies against the antigen. The activated B-cell divides and produces large numbers of plasma cells that produce the antibodies and memory cells that can be activated later when the person is again exposed to the same pathogen.
Once the trouble is brought under control, the number of plasma cells slowly drops and so does the antibody level. This leaves the memory B-cells to serve as a backup team, should that antigen appear in the future. Memory B-cells know how to make the correct antibody to defend against that specific antigen, but they don’t make much of it. The antibodies they produce are on their surface. If the same antigens appear again, they attach to the antibodies causing the memory B-cells to undergo mitosis, changing into a large population of antibody-secreting plasma cells. A second exposure to an antigen results in a more rapid increase in the level of antibodies because the memory cells already have the ability to produce the antibody needed. The amount of antibody increases rapidly and again protects the body from harm.
Immunization is the technique used to induce the immune system to develop an acquired immunity to a specific disease by the use of a vaccine. Vaccines are antigens made so they can start an active immunity without causing disease. A vaccine can be a solution that contains whole, live pathogens in a form so changed that they are not harmful. It can also contain dead organisms or just the antigenic portion of the pathogen; some vaccines are synthetic. When the vaccine is first given, B-cells become activated, just as they do when they encounter an actual disease organism. This is called the primary immune response (figure 26.24). The next time the person is exposed to the vaccine, there is a sharp increase in the amount of antibody produced. This is called the secondary immune response. As time passes, the amount of antibody will begin to fall. It will remain high only if the person is repeatedly exposed to the same antigen, either by accident or as the result of a booster shot. For example, if a person lives or works in an area where tetanus toxin can regularly stimulate a secondary immune response (e.g., through a puncture wound), a constant high level of immunity to tetanus toxin is naturally maintained. Each time the memory B-cells come in contact with tetanus toxin, the amount of antibody is “boosted” to its maximum protective level. If natural exposure does not occur, the amount of antibody falls slowly, sometimes reaching a low, unprotective level. There are no quick ways to determine how “naturally” protected someone is. If a physician suspects that a patient might develop a case of tetanus, a booster injection of tetanus vaccine is given to stimulate antibody production artificially to ensure a high level of protection.
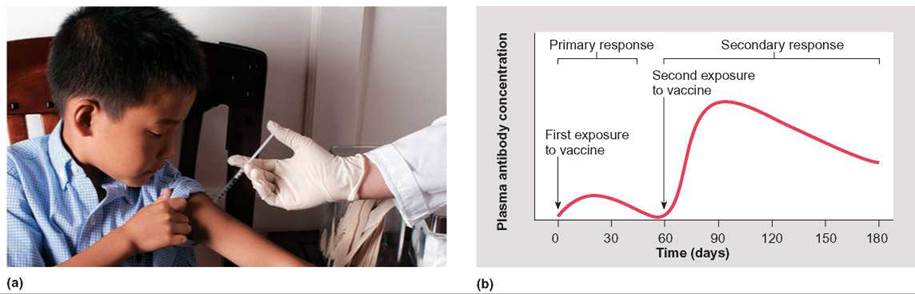
FIGURE 26.24. Active Immunity Due to Immunization
(a) Vaccines immunize children against various childhood diseases. (b) The primary immune response, after the first exposure to a vaccine, is minimal, but the secondary immune response, which may occur after the second exposure, shows a dramatic rise in the amount of antibody present in the plasma.
As a disease travels through a population, surviving individuals have developed an immunity that makes them resistant to reinfection. It also keeps them from becoming the source of infection to others. Thus, the population as a whole develops what is known as herd immunity. This concept is based on the relative proportions of immune and susceptible individuals in the population (herd). In other words, if enough people become immune as the result of contracting the illness or immunization, there is less chance that the susceptible people will get the illness. You see herd immunity develop during the “flu season.” At first, there is an increase in the number of cases, they reach a peak, and finally the number of cases decreases as more people become immune. If enough people in the population (herd) were to be vaccinated before the virus arrived, the immunized people would protect those who, for whatever reason, did not or could not get the vaccine. Public health officials try to immunize large portions of the susceptible population in an attempt to maintain a high level of herd immunity. The proportion of immune to susceptible persons must be constantly monitored because new susceptible individuals continuously enter a population through migration and birth and because pathogens change so that they do not necessarily display the same antigens.
T-Cells and Cell-Mediated Immunity
Cells that will become T-lymphocytes (T-cells) are initially produced in the bone marrow but travel to the thymus gland where they differentiate into T-cells. After they are differentiated they leave the thymus and are found in the blood, lymph, and lymph tissue. Like B-cells, T-cells must be brought into battle through an activation process. To activate T-cells, the antigen must be “presented” to them by other cells, called antigen-presenting cells (APCs) which are often macrophages that have phagocytosed the pathogen. Phagocytosis was covered in chapter 4. Inside an APC, the pathogen is broken down, and each antigenic molecule is attached to a molecule already present in the APC. This new combination is inserted into the APC’s cell membrane so that each molecule sticks out on the APC’s surface like a microscopic hair. The APC activates the T-cells by presenting the antigen to T-cells when they attach to one another at receptor sites on the surface of the T-cells (figure 26.25). Several kind of T-cells with specific functions have been identified.
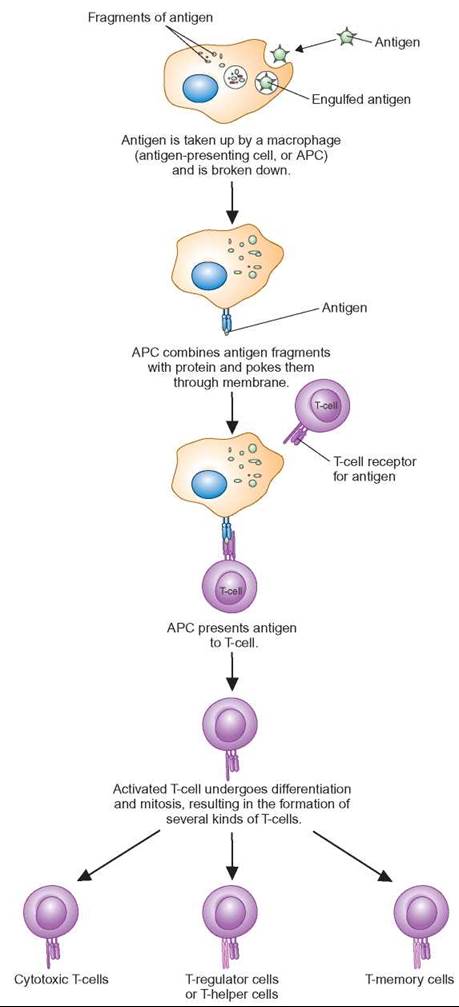
FIGURE 26.25. Specialized T-Cells
T-cells become specialized as T-regulator cells, T-helper cells, cytotoxic T-cells, or T-memory cells by interaction with an antigen- presenting cell (APC). APCs are macrophages that have engulfed an antigen and present it to undifferentiated T-cells. Once differentiated, each kind of T-cell has a special job to perform in defending the body against harm.
T-helper cells produce chemicals called cytokines. When disease organisms invade the body or other cellular abnormalities occur, cytokines stimulate the actions of B-cells to produce antibodies; stimulate cytotoxic T-cells to kill infected body cells; and recruit macrophages and phagocytes to consume damaged cells.
T-regulator cells produce cytokines that are responsible for shutting down the immune response of both B- and T-cells following a period when they were activated to fight an infection. They are also important in preventing immune system cells from attacking normal body cells.
Cytotoxic T-cells are specialized for killing body cells that cause disease. After identifying the enemy cells, cytotoxic T-cells move toward their target cells, press up against their surface, and make holes in them. Cytotoxic T-cells target cancer cells, cells infected with viruses or intracellular bacteria or protozoa, and foreign cells, such as cells from an organ transplant.
T-memory cells are generated in much the same fashion as B-memory cells, and they play a similar role. They remember the specific antigen of their enemy and can multiply when exposed to the same antigen at a later time (Outlooks 26.1).
OUTLOOKS 26.1
The Immune System and Transplants
People who have damaged tissues or organs often die even though the other parts of their body are functioning normally. Therefore, transplantation of healthy tissues or organs from one person to another could save lives. Because our immune system is designed to attack organisms or cells that display foreign antigens on their surface, successful transplants must avoid being attacked by the recipient's immune system.
There are genes on chromosome 6 in humans that produce proteins that are displayed on the surface of all cells. The proteins are called human leukocyte antigen (HLA) proteins. (The genes are also called major histocompatibility complex [MHC] genes and are found in nearly all vertebrates.) There are on the order of 200 different alleles for these genes. Each person has a specific set of these genes and the proteins they produce and, since there are so many possible combinations of these alleles, each person displays a unique combination of these antigens on their cell surfaces. For the transplant of most tissues or organs to be successful, the antigens of the donor tissue must resemble those of the recipient as closely as possible.
Determining whether the tissues of a donor and recipient are closely matched is a three-step process. First, the blood types (A, B, AB, O) of the donor and the recipient must be compatible (see chapter 10 for a discussion of blood type). Second, a set of HLA proteins are matched. Six of these proteins are considered when making a match. The greatest success is achieved when all six antigens are the same for both the donor and the recipient. Finally, a cross-match is made to make sure that the recipient has not been exposed previously to an antigenic substance in the donor tissue that would trigger a reaction against the donor tissue. The most common causes of exposure to other human antigens are pregnancy (exposure to some of a fetus's antigens), blood transfusions, and previous transplants.
A few kinds of tissues do not have blood vessels (cornea of the eye, tendons, cartilage). Because the recipient's blood and the B- and T-lymphocytes in the blood do not flow through these tissues, the recipient does not become sensitized to the foreign material. Therefore, transplanting these structures usually does not cause the recipient's immune system to reject the transplant.
Blood transfusions are also a special case of tissue transplantation that does not require matching of the HLA antigens. This is because the red blood cells do not express the HLA genes and platelets express these genes very weakly. Although lymphocytes do express the HLA genes, the rejection reaction is usually not a problem because blood transfusions are a temporary replacement. Instead of the three-step process, the blood type (A, B, AB, and O) and a second blood type called the Rh factor, of the donor and recipient are matched and a sample of the donor's red blood cells is mixed with a sample of the recipient's plasma to determine if there are any antigens on the donor's red blood cells that will cause a problem.
All other organ and tissue transplants require all three steps to assure that there is a reasonable chance that the donated tissue will be accepted by the recipient's immune system. Even when the match is as close as possible, most transplant recipients must use drugs that suppress the immune system for their lifetime.

Immune System Diseases
As with other body systems, the immune system can malfunction, resulting in diseases. The most common are allergic reactions, autoimmune diseases, and immunodeficiency diseases. An allergy is an abnormal immune reaction to an antigen. Possibly the most familiar are allergies to foods, pollens, and drugs. Such allergies are also known as type I hypersensitivities. All allergies involve the interaction of an antigen with a B-cell antibody. An antigen that causes an allergy and comes from outside the body, such as dust, pollen, tobacco, fungi, eggs, and penicillin, is called an allergen.
Type I hypersensitivities are associated with immunoglobulin E (IgE). B-cells capable of producing IgE are first exposed to the allergen through the skin, respiratory tract, or intestinal tract and become activated. Unlike most other immunoglobulins, IgE can bind to the surface of mast cells and basophils (figure 26.26). When a person comes in contact with the allergen a second time, the allergen (antigen) attaches to the antibody, which is already attached to mast cells and basophils. This causes the release of large amounts of histamine, leukotrienes, and prostaglandins that cause a variety of symptoms. Symptoms vary greatly in people and include skin rashes, hives, itching throat, asthma, eczema, migraine headaches, and bedwetting.
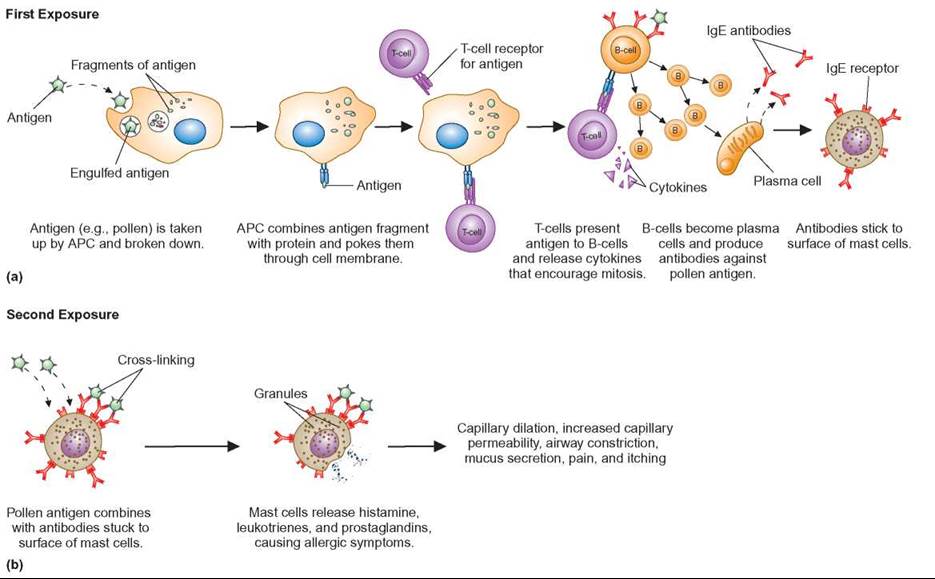
FIGURE 26.26. How an IgE Allergy Works
(a) When a person is first exposed to an allergen, such as pollen, the allergen is taken up by an antigen-presenting cell (APC), which initiates a complex series of events that lead to the release of IgE antibodies, which stick to the surface of mast cells and basophils. A few days later, when pollen is encountered again, (b) the increased population of antibody-coated mast cells combines with the allergen, causing them to release the chemicals responsible for the symptoms.
The most severe allergic reaction is anaphylactic shock. Within minutes after exposure to the allergen, this shock reaction progresses from (1) extensive skin reddening and itching to (2) smooth muscle spasms to (3) capillary breakage in the skin, eyes, and internal organs to (4) a burning sensation in the rectum, the mouth, and possibly the vagina to (5) severe headache to (6) hot flashes to (7) a quick drop in blood pressure to (8) a constriction of bronchial smooth muscle, resulting in respiratory failure, to (9) death. To counteract anaphylactic shock, people with severe allergic reactions are advised to carry and use an EpiPen as soon as they are exposed to the allergen. The medication in this single-use hypodermic syringe is epinephrine (adrenalin), which quickly counteracts the symptoms. However, after using the pen, the person should seek medical attention immediately, because the EpiPen may not totally control the reaction.

Autoimmune diseases are disorders that result from the immune system’s turning against the normal chemicals and cells of the body. In other words, the immune response makes a mistake, sees healthy cells as harmful, and attacks them. Some examples of autoimmune diseases are rheumatoid arthritis, type 1 (insulin-dependent) diabetes, systemic lupus, Crohn’s disease, and psoriasis. In rheumatoid arthritis, B-cells produce antibodies that mistakenly identify proteins in the cartilage and bone as dangerous and destroy them. In type 1 diabetes, the insulin-producing cells of the pancreas are destroyed by T-cells.
Immunodeficiency diseases are disorders that result from the immune system’s not producing one or more component cells or chemicals. In this situation, the system cannot provide the protection needed to maintain health. People with such disorders are more susceptible to infections and cancers. People born with the genetic disorder severe combined immunodeficiency disease (SCIDS), or “boy-in-the-bubble” disease, lack the ability to synthesize the enzyme adenosine deaminase (ADA), which is crucial to the formation of T-cells.
Acquired immunodeficiency syndrome (AIDS) is also an immunodeficiency disease but is not genetic. AIDS is the result of a virus infection caused by the human immunodeficiency virus (HIV). HIV infects T- and B-cells and eventually destroys them. When the immune system’s population of T-cells has been reduced significantly, it can no longer defend the body against microbial infections. It also loses its ability to recognize and destroy tumor cells.
26.7. CONCEPT REVIEW
18. What are the differences between innate and adaptive immunity?
19. How do B-cell and T-cell systems work to defend against disease?
Summary
A nerve impulse is caused by sodium ions entering the cell as a result of a change in the permeability of the cell membrane. Thus, a wave of depolarization passes down the length of a neuron to the synapse. The axon of a neuron secretes a neurotransmitter, such as acetylcholine, into the synapse, where these molecules bind to the dendrite of the next cell in the chain, resulting in an impulse in it as well. The acetylcholinesterase present in the synapse destroys acetylcholine, so that it does not repeatedly stimulate the dendrite. The brain is composed of several functional units. The lower portions of the brain control automatic activities, the middle portion of the brain controls the basic categorizing of sensory input, and the higher levels of the brain are involved in thinking and self-awareness.
Several kinds of sensory inputs are possible. Many kinds of chemicals can bind to cell surfaces and be recognized. This is how the senses of taste and smell function. Light energy can be detected because light causes certain molecules in the retina of the eye to decompose and stimulate neurons. Sound can be detected because fluid in the cochlea of the ear is caused to vibrate, and special cells detect this movement and stimulate neurons. The sense of touch consists of a variety of receptors that respond to pressure, cell damage, and temperature.
Muscles shorten because of the ability of actin and myosin to bind to one another. A portion of the myosin molecule is caused to bend when ATP is used, resulting in the sliding of actin and myosin molecules past each other. Skeletal muscle responds to nervous stimulation to cause movements of the skeleton. Smooth muscle and cardiac muscle have internally generated contractions, which can be modified by nervous stimulation or hormones.
There are two types of glands: exocrine glands, which secrete through ducts into the cavity of an organ or to the surface of the skin; and endocrine glands, which release their secretions into the circulatory system. Digestive glands and sweat glands are examples of exocrine glands. Endocrine glands, such as the ovaries, testes, and pituitary gland, change the activities of cells and often cause responses resulting in growth over a period of time. The endocrine system and the nervous system are interrelated. Actions of the endocrine system can change how the nervous system functions, and the reverse is also true.
The immune system defends the body against potentially harmful agents, including microbes, toxins, and abnormal cells. Innate immune mechanisms protect the body against many kinds of harmful agents. Adaptive immune mechanisms can tell the difference between one kind of threat and another based on their exact chemical makeup. After recognizing the enemy, the body selects a specific combination of chemicals and cells to send into the battle to destroy only that enemy. Cells important to the system include B-lymphocytes, T-lymphocytes, and macrophages. Abnormally functioning immune systems can result in allergies, immunodeficiency, and autoimmune diseases.
Basic Review
1. The _____ is the space between the fibers of adjacent neurons in a chain.
2. In the _____, the somatic nervous system controls the skeletal (voluntary) muscles and the autonomic nervous system controls smooth (involuntary) muscles, the heart, and glands.
a. peripheral nervous system
b. central nervous system
c. immune system
d. medulla oblongata
3. The cells that a specific hormone affects are called
a. target cells.
b. neurons.
c. motor units.
d. T-lymphocytes.
4. _____ glands have no ducts and secrete their products into the circulatory system.
a. Exocrine
b. Endocrine
c. Salivary
d. Sweat
5. The mechanism by which an increase in a stimulus causes a reduction in a response is called
a. positive-feedback regulation.
b. immune.
c. negative-feedback control.
d. absolute.
6. Molecules that are neurotransmitters manufactured in the soma and migrate down the axon, where they are stored until needed, are called
a. somas.
b. acetylcholine.
c. cytokines.
d. estrogen.
7. Which of the following is a resulting symptom of inflammatory chemicals that cause increased blood flow and dilation of capillaries?
a. swelling
b. estrogens
c. atherosclerosis
d. nausea
8. Which cells of the immune system produce memory cells?
a. both B- and T-lymphocytes
b. B-lymphocytes only
c. T-lymphocytes only
d. macrophages
9. Histamine, leukotrienes, and prostaglandins are compounds produced and released by which cells during an allergic reaction?
a. WBCs
b. RBCs
c. basophils
d. macrophages
10. In muscle, thin myofilaments composed of the proteins actin, tropomyosin, and troponin alternate with thick myofilaments composed primarily of the protein _____.
11. A nerve impulse involves
a. a change in the permeability of the cell membrane.
b. the flow of sodium ions into the nerve cell.
c. depolarization of the nerve cell membrane.
d. All of the above are correct.
12. The chemicals produced by endocrine glands that cause changes in other tissues are called _____.
13. The cells in the retina of the eye that are able to detect different colors are called _____ .
14. The chemical sense of taste
a. has only about five kinds of chemical receptors.
b. is only found on the tip of the tongue.
c. fatigues very rapidly.
d. is learned.
15. Hearing involves
a. the movement of tiny hairs in the cochlea.
b. the movement of fluid in the cochlea.
c. nerve impulses from the cochlea to the brain.
d. All of the above are correct.
Answers
1. synapse 2. a 3. a 4. b 5. c 6. b 7. a 8. a 9. c 10. myosin 11. d 12. hormones 13. cones 14. a 15. D
Thinking Critically
Can We Improve Our Sense of Smell?
Humans are considered to have a poor sense of smell. However, when parents are presented with baby clothing, they are able to identify the clothing with which their own infant had been in contact with a high degree of accuracy. Specially trained individuals, such as wine and perfume testers, are able to identify large numbers of different kinds of molecules that the average person cannot identify. Birds rely primarily on sound and sight for information about their environment; they have a poor sense of smell. Most mammals are known to have a very well-developed sense of smell. Is it possible that we have evolved into sound-and-sight-dependent organisms, like birds, and have lost the keen sense of smell of our ancestors? Or is it that we just don’t use our sense of smell to its full potential? Devise an experiment that would help shed light on this question.