Must Know High School Biology - Kellie Ploeger Cox 2019
PART FIVE Forms of Life
The Animal Immune System
MUST ![]() KNOW
KNOW
![]() The immune system is based on recognition of self versus non-self.
The immune system is based on recognition of self versus non-self.
![]() The immune system’s first and second lines of defense are innate and nonspecific.
The immune system’s first and second lines of defense are innate and nonspecific.
![]() The immune system’s third line of defense is specific and has memory.
The immune system’s third line of defense is specific and has memory.
We are constantly waging a battle against foreign invaders. If your body has the upper hand, you don’t even know the battle is being fought; if you are losing the war, you’ll know: fever, aches, runny nose, and maybe even some swelling. Your symptoms during sickness are by-products of your immune system revving up to full speed in order to destroy the invading pathogens. Your must know is to understand the immune system wages a you-versus-not-you battle, immunologically speaking.
You are a happy collection of cells: obviously your own cells, but also all the bacterial cells that are colonizing the inside and outside of you. Do not discount these prokaryotic tenants as passive passengers—without our microbial community, we could not survive.
![]()
IRL
Our bodies are ecosystems composed of many different populations spread out upon a landscape of varying tissue terrains. Humans have on average 1,000 different microbial species colonizing our bodies. There are salt-tolerant Staphylococcus species living on our skin, the cavity-causing Streptococcus mutans hanging out on our teeth, and fiber-digesting Bacteroides residing in our intestines. Yes, some of these bacteria are bad, but most are good, and their presence is keeping us healthy. The entire collection of microbial species colonizing our bodies is referred to as the microbiome, and research is continuing to elucidate how important our microbiomes are to our general health. Some bacteria, for example, provide a direct benefit, such as Lactobacillus providing B vitamins in our large intestine.
Oftentimes, the benefits aren’t as obvious (but are just as important). When we have these good bacteria taking up residence on our bodies, they are effectively preventing bad bacteria from moving into the neighborhood. As you will soon learn, ecological niches can only be inhabited by a single species; we want friendly species inhabiting our bodies’ niches.
Unfortunately, you often don’t realize the benefit until it’s gone. If you have ever taken antibiotics in order to fight an infection, you might have suffered some side effects such as diarrhea and cramping. This occurred because the antibiotics also wiped out some of your good gut bacteria. The collateral damage of removing a happy inhabitant opened up a niche that can now be occupied by the not-so-welcomed. An extreme example is an infection of Clostridium difficile, a bacterial species that is an opportunistic invader of the colon, and can cause severe diarrhea or even life-threatening inflammation.
Your body has multiple layers of defense, essentially protecting your insides from the outside. We will go over each of these, as if a foreign invader is trying to get into your body. First, it will push against a sweaty, acidic wall (your outside layer), then it will break through to be surrounded by a swarm of hungry eating machines (second line of defense), and finally it will face a tailor-made army of specific cells designed for this particular pathogen (third line of defense).
The Immune System’s Three Lines of Defense
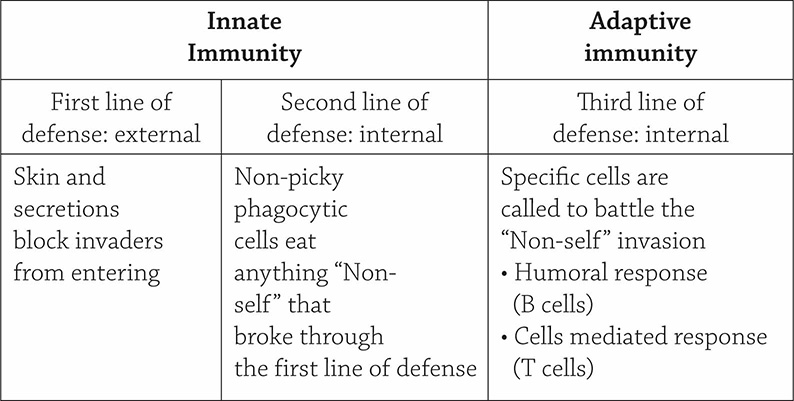
First Line of Defense: Outer Barriers
The first line of defense is the very barrier that separates you from your surroundings: your skin! The epidermal layer is a watertight wall that prevents things from easily passing through. Not only does it physically block things from entering, it also creates a hostile chemical environment by secreting acidic and salty sweat. Even the bits that seem like easy ways to sneak past the wall (such as your eyes and mouth) have their own defensive abilities: both tears and saliva contain the enzyme lysozyme, which destroys bacterial cell walls. This is a passive and nonspecific response to invasion because it need not be triggered for each specific infection—it’s ready to do its job, regardless of the type of pathogen.
Second Line of Defense: Phagocytes and Inflammation
Imagine you accidentally cut your hand against a tree branch. After a bit of light bleeding and mild pain, the wound becomes swollen, red, and tender. Welcome to the second line of defense! Something got past your skin (easy to do if there is a cut), and the invader is met by a team of specialized cells called phagocytes. A phagocytic cell is a cell of the immune system that ingests and breaks down bacteria and other foreign substances. There are specific types of phagocytic cells called macrophages and neutrophils. The pain/heat/swelling of an injury is all supposed to help these phagocytes swoop into the injury site. When tissues are damaged (the cut), a chemical called histamine is released, causing the capillaries in the vicinity to dilate (increased blood flow causes the heat) and leak fluids into the surrounding tissue (the swelling). This brings in the phagocytes and allows them to sneak through the capillary walls into the tissues, where the infection lies. As it was in the first line of defense, these phagocytes act innately and quickly, regardless of the infectious agent. For this chapter, our second must know refers back to what we just learned: the first and second lines of defense are innate and nonspecific.
Third Line of Defense: Adaptive Immunity
Now things get interesting. Mammals have this amazing thing called adaptive immunity, where the body mounts an immune response when challenged by outside invaders. Keeping our must know concepts in mind, if the first and second lines of defense are both innate (work immediately) and nonspecific (doesn’t matter the pathogen), the third line of defense is specific (the type of pathogen matters) and needs to first learn about the pathogen before it can mount a full offensive response (it is not innate and immediate). Before I get into the details, let’s first learn some helpful vocabulary. Our immune systems are based on this idea of self versus non-self, right? We call any potentially pathogenic non-self invader an antigen. To be even more specific, an antigen does not need to be an entire, intact bacterium or virus; it can be a part of a pathogen, such as a specific viral protein or piece of bacterial cell membrane. This idea will be important later, when we talk about vaccinations. If an antigen is the bad guy, your lymphocytes are the good guys. Lymphocytes are special immune system cells (commonly called white blood cells), of which there are two types: B cells and T cells. The B cells are responsible for the immune system’s humoral response (targeting antigens that are freely floating around in the bloodstream), and the T cells are in charge of the immune system’s cell-mediated response (targeting invasions that directly involve your own body cells).
Before we look at the humoral and cell-mediated responses in more detail, I want to first provide a big-picture overview for you. Yeah, okay, the immune response is specific and has memory. What exactly does that mean? Well, the two concepts actually go hand in hand. When a specific pathogen enters your body, only one circulating B or T cell is equipped to deal with it. Seriously, it’s mind-blowing. When each of your lymphocytes are created, there is a slight (intentional) difference in their cell membrane surface receptors. This means each lymphocyte can latch on to a unique antigen:
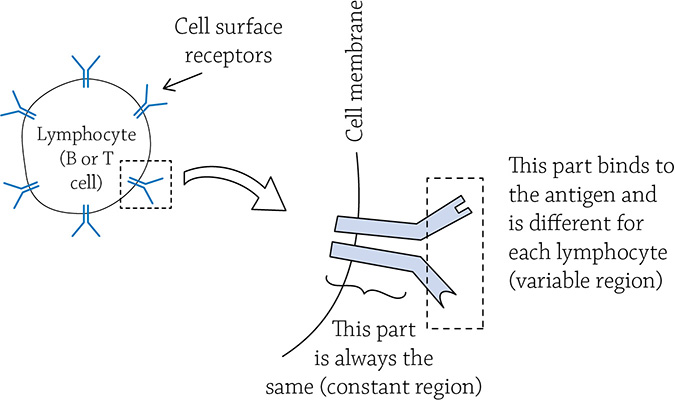
Variable and constant regions of lymphocyte cell surface receptors
That’s the “specific” part of your immune system. There is a countless number of variations in lymphocytes in order to match the countless number of different antigens that may assault your body. But clearly, a single lymphocyte isn’t enough to counteract an invasion. That one special lymphocyte, however, immediately begins to copy itself once it latches on to the pathogen; the antigen-lymphocyte contact is like a call to arms. The “chosen” lymphocyte now knows there is an invasion occurring, and it is the only one able to stop it! By cloning itself (copying itself over and over again), it creates an army of cells that all match the invading antigen.
So here is where the memory part comes into play: once the invading pathogen is destroyed and the threat is removed, the numbers of lymphocytes specific for that particular pathogen never completely go away. There remains a troupe of memory cells, just in case that one pathogen tries its luck again in a second invasion. If it does invade a second time, it won’t have a chance … those memory cells are waiting, clone themselves immediately, and wipe out the non-self invader before you even have a chance to feel sick!
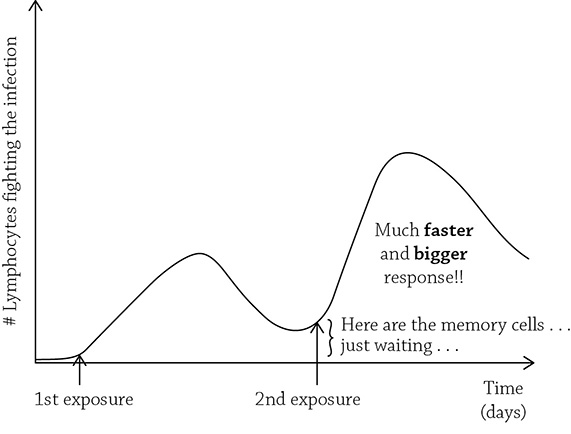
Primary and (faster) secondary immune responses to the same pathogen
You can see that the heightened secondary response is due to those memory cells, just waiting for a second chance to fight the infection. Keep this in mind when we consider the science behind vaccinations, later on in the chapter. Also keep in mind our third must know: the third line of defense is specific and has memory.
B Cells and the Humoral Response
As I mentioned earlier, the humoral response and the cell-mediated response target slightly different enemies. First, let’s talk about the humoral response. This is the immune system’s reaction to extracellular pathogens (extracellular means outside of a cell). As we learned, a lucky B cell will be activated because its cell membrane receptor perfectly matches the offending antigen. Once the B cell latches on to the antigen, it will begin to clone itself, and each B cell will begin to secrete these tiny proteins called antibodies that look just like the B cell’s membrane receptor. These little antibodies take down the infection by binding to the virus (or toxin, or bacterium), causing them to clump up into easy-to-eat aggregates. This entices the phagocytic cell (remember that guy? From the second line of defense?) to gobble up the pathogen. The B cells that secreted all those helpful antibodies are called plasma cells; there are other B cells that will abide their time and wait for a second exposure to that same pathogen. They comprise the memory part of our immune system, and are called memory B cells.
![]()
Take note of the fact that these B cells make direct contact with the antigen (the little black triangle). This is possible because the humoral response focuses on extracellular pathogens, floating around freely in the body fluids, not trying to hide in your own body cells. The sneaky hidden pathogens require a different approach. Call in the cell-mediated immune response!
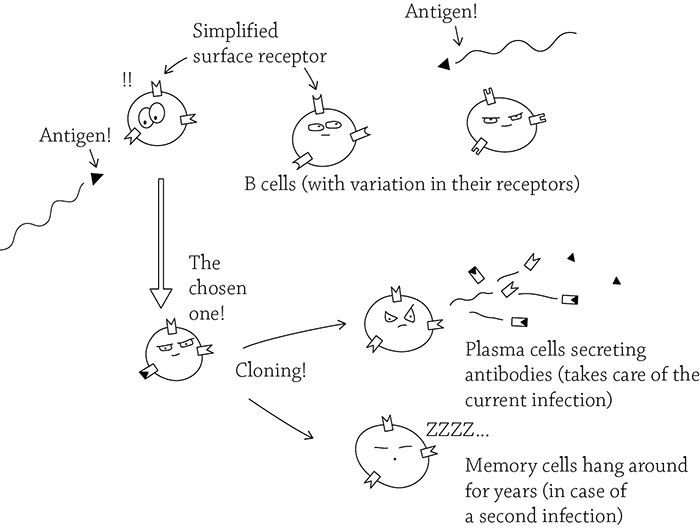
B cells and the humoral response
T Cells and the Cell-Mediated Response
Oftentimes, a viral infection is “hidden” in your body. Viruses are obligate intracellular parasites, meaning they cannot reproduce unless they invade and commandeer one of your body cells (how rude). Luckily, T cells are able to deal with this sneaky sort of invasion. It requires the help of the infected cell in which the antigen is concealed. A T cell (specifically called a cytotoxic T cell, or Tc, is called to arms if an infected body cell raises an alarm. Specifically, the infected body cell will take a fragment of the virus and combine it with a special protein that identifies “self,” called MHC.
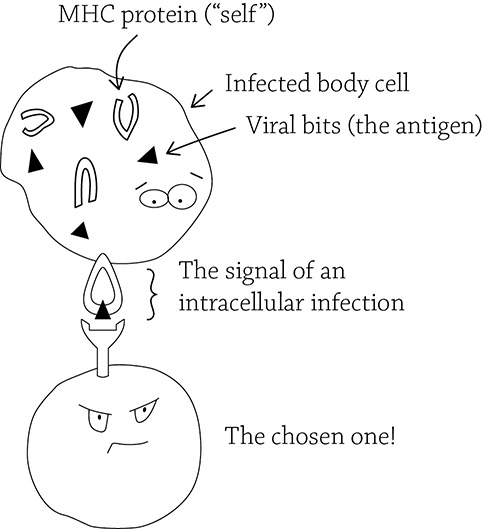
T cells and the cell-mediated response
Just like in our B cell scenario, the one cytotoxic T cell that matches the antigen will clone itself to create two populations: some memory T cells, in case the infection happens again, and a population of active cytotoxic T cells that will take care of the current infection. How does the immune system deal with a viral invasion? Its best approach is to get ahead of the infection by destroying the already-infected cells in order to stop the virus from reproducing. Interestingly enough, Tc cells also attack another form of compromised body cells: cancer.
![]()
Everybody has a unique chemical marker on the surface of their body cells. This marker—called a major histocompatibility complex (or MHC for short)—is how our immune system can identify self from non-self. Interestingly enough, everyone’s unique MHC also contributes to their body odor (and may play a subconscious role in mate preference).
When a roving Tc comes into contact with a body cell holding out the combination of self (MHC) and non-self (the antigen), it knows there’s an invasion happening. The Tc cell will clone itself (just like our B cell did), and start to immediately deal with the infection.
![]()
IRL
There’s yet one other scenario where your protective cytotoxic T cells attack other cells that seem abnormal: organ transplants. It makes perfect sense! These are body cells that appear a bit *off* (T cells’ expertise). Therefore, when a person gets an organ transplant, one of the medications they take is to calm down their immune response, so their body doesn’t reject the new organ.
Active Immunity, Passive Immunity, and Vaccinations
If you catch the flu from your friend, your immune system will rev up and deal with the infection. This is an example of active immunity, because your immune system is reacting to the introduction of an antigen and mounting a response by finding that lone B or T cell that best matches the invader, cloning it, and dealing with the immediate threat (plus creating a population of memory cells, in case the threat comes back). Here is another scenario: you are out hiking and a venomous rattlesnake bites you. Are you willing to wait for your immune system to mount a response to the venom? Sit idly by as the correct B cell clones itself and creates a sufficient concentration of antibodies to inactivate the venom that is sweeping through your body? Um, no. That is why hospitals in rattlesnake regions have something called antivenin (or antivenom), a medication that contains antibodies against specific poisons, such as those in the venom of snakes, spiders, and scorpions.
![]()
IRL
The terms venomous and toxic are easy to use incorrectly. Something is considered venomous if its poison is transferred to you through a bite; something is toxic if the poison is ingested (eaten, like tetrodotoxin from the puffer fish we learned about earlier).
Antivenin is cool because you are injecting the already-made antibodies directly into the bloodstream, without waiting for your own body to create them. This also occurs in newborns, who have yet to develop their own immune systems. They are given antibodies through the placenta and, once born, in their mother’s milk. Chances are, the mother is exposed to the same environmental antigens as their baby, so why not share some antibodies? Once the newborn has a functioning immune system (around three months old), they no longer have to rely on the passive transference of antibodies from their mother. That is the key term: passive. If antibodies are passively given to you, you (and your immune system) did not go through the work to create them. Active immunity, however, is when your immune system directly responds to the infection and creates its own antibodies.
![]()
What is one good thing and one bad thing about the passive immune response? It’s good because it’s fast (snake bite!) and antibodies are kindly given to you. But if you are bitten again by a rattlesnake (maybe a sign that you need to rethink your hiking locations), is your immune system now ready to protect you? Nope. The bad thing about the passive immune response is that there is no memory. Since your own body did not go through the process of cloning the correct lymphocytes (B or T cell), there is no population of memory cells hanging about and providing protection in case of a second attack.
Regardless of how your body acquires the antibodies, our must know concept still applies: both are a matter of self versus non-self. But what about vaccinations? A vaccine is a medicine created from parts of a pathogen, in order to intentionally challenge a person’s immune response to that particular pathogen. If this active or passive immunity? Vaccinations are an example of active immunity, regardless of it being a purposeful administration instead of a natural exposure. A vaccine not only refers back to our first must know (self versus non-self), but is also an example of the third must know: the immune system’s third line of defense is specific and has memory.
![]()
IRL
Speaking of memory, a vaccination’s memory cells can last years, even decades, depending on the disease it is protecting against. If the memory cells begin to dwindle, that is when you get a booster shot (a second vaccination, intended to remind your immune system about that disease you were vaccinated against years ago).
The importance of vaccinations cannot be underestimated. Here is an easy means to protect you and your loved ones against potentially deadly diseases. Vaccines are composed of parts of the pathogen (or, in some cases, an attenuated—weakened—version of the pathogen), so a vaccine is unable to actually give a person the disease. You may experience mild symptoms, but this is still much, much preferable to actually contracting the disease. Furthermore, any ickiness you may feel after a vaccination means your immune system is responding to the pathogen, which is a GOOD THING. You want those B and T cells to create a population of memory cells, willing to hang around and protect you against the flu, or measles, or cervical cancer, or tetanus, and so on. Not only are vaccinations important for your health, they are also important for the health of others that are themselves unable to vaccinate due to illness or infancy. There is a phenomenon called herd immunity that helps to protect those at risk by stopping the spread of a disease by ensuring most of us are vaccinated. It’s a social contract to help not only ourselves, but others that are unfortunately unable to protect themselves.
REVIEW QUESTIONS
1. What does the first and second lines of defense have in common (not shared by the third line of defense)?
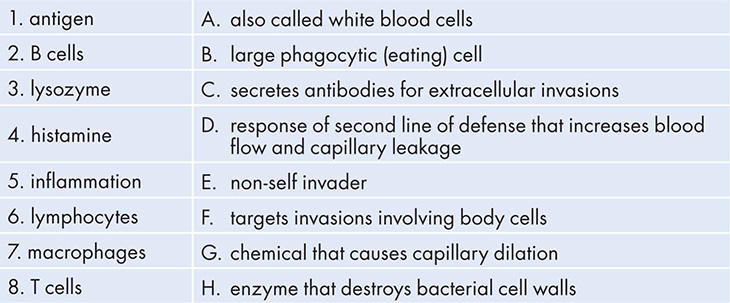
2. Match the word with the appropriate definition:
3. Choose the correct term from each pair: The cell-mediated response targets intracellular/extracellular pathogens such as viruses/pollen and relies on B cells/T cells.
4. Choose the correct term from each pair: How does the immune system “remember” an infection and protect you against a second invasion? How is it related to vaccine function?
5. Choose the correct term from each pair: What is the first line of defense when an antigen is attempting to invade your body?
6. Choose the correct term from each pair: The humoral response targets intracellular/extracellular pathogens and relies on B cells/T cells to produce antigens/antibodies to bind to and help remove the invader.
7. How does passive immunity differ from active immunity? When is this sort of immunity important?
8. Every year, you need to be revaccinated against the seasonal flu virus. Why is this necessary, unlike other vaccines that offer protection for years?
