Biology of Humans
17a. Sexually Transmitted Diseases and AIDS
In the previous chapter, we discussed the structure and function of the reproductive systems. We also discussed birth control. In that discussion we mentioned the effectiveness of each method of birth control in preventing pregnancy and in preventing the spread of sexually transmitted diseases (STDs). In this chapter, we first describe three STDs that are caused by bacteria: chlamydia, gonorrhea, and syphilis. Then we describe three STDs that are caused by viruses: genital herpes, genital warts, and HIV/AIDS. HIV is discussed in this chapter because sexual contact is the most common means of transmission, although the virus can be transmitted in other ways as well.
Long-Lasting Effects of STDs
Sexually transmitted diseases (STDs) take a serious toll on humanity, both in their direct effects on the infected individuals and because of the cost to society in general. Nineteen million infections occur each year in the United States. Two-thirds of the U.S. residents infected are younger than 25. The cost of treating their infections is in the billions of dollars.
We should also mention another trait of STDs: they are sexist. They affect women more severely than men, causing sterility more often in women than in men, ectopic pregnancy (a pregnancy in which the embryo begins development outside the uterus), and cervical cancer.
STDs are most common among adolescents and young adults (aged 14-26) because they are the most sexually active segment of the population. Indeed, 26% of female adolescents 14 to 19 years old have at least one STD, and 15% have more than one STD. Furthermore, 20.1% of females who have had only one lifetime sexual partner (so far) have contracted at least one STD. And, 50% or more of female adolescents with three or more partners has an STD. The most common STD is genital infections with the human papillomavirus (HPV).
· HIV/AIDS is a global pandemic.
One reason STDs are so rampant is that people are often unaware of being infected. Many cases of STDs lack symptoms. Indeed, the prevalence of asymptomatic cases has led to use of the term sexually transmitted infection (STI) rather than sexually transmitted disease. Also, the symptoms of some STDs, such as syphilis, disappear without treatment, leading the person to believe—mistakenly—that he or she is cured.
STDs Caused by Bacteria
We consider three STDs that are caused by bacteria: chlamydia, gonorrhea, and syphilis.
Chlamydia and Gonorrhea
Chlamydia, the most frequently reported infectious disease in the United States, is caused by a very small bacterium (Chlamydia trachomatis) that cannot grow outside a human cell. One of the oldest known sexually transmitted diseases, gonorrhea, is caused by the bacterium Neisseria gonorrhoeae.
Chlamydial infections are rapidly becoming epidemic because they are highly contagious and because they do not necessarily cause noticeable symptoms that would prompt the infected person to seek treatment (Figure 17a.1). In fact, most people who have chlamydia do not have symptoms, and many people learn that they have it only because a responsible partner diagnosed with the infection informs them. Any symptoms that do develop may take weeks or months to appear. In the meantime, even without outward signs of infection, the disease can be passed along to others.
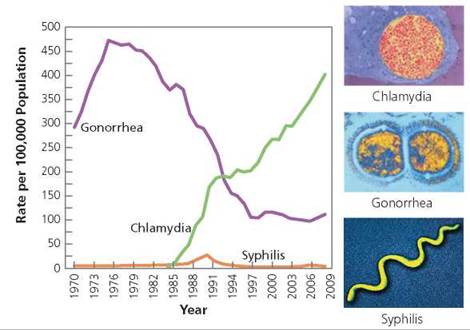
FIGURE 17a.1. The relative rates of chlamydia, gonorrhea, and syphilis from 1984 to 2008. The bacteria that cause these STDs are shown at the right. Centers for Disease Control
Chlamydia and gonorrhea primarily infect the mucous membranes of the genital or urinary tract, throat, or anus. The bacteria that cause these STDs cannot survive long if exposed to air, so they are generally transferred by direct contact between an infected mucous membrane and an uninfected one during sexual intimacy. The bacteria can infect the cells of mucous membranes, including those of the urethra, vagina, cervix, oviducts, throat, anus, and eyes. The most common sites of infection are the mucous membranes of the urethra or the reproductive structures, because these are most likely to be in contact during sexual intimacy. Chlamydia and gonorrhea can also spread to the lining of the anus during anal intercourse or to the throat during oral sex. Furthermore, they can infect the eyes if an eye is touched by a finger that has just touched an infected area. In the case of infants, eye infection can occur as the baby passes through an infected vagina or cervix during the birth process.
The most common symptoms of chlamydia or gonorrhea are those of urinary tract infection. Inflammation of the urethra causes a burning sensation during urination, itching or burning around the opening of the urethra, and a discharge from the urethra (Figure 17a.2). In males, the most common site of chlamydial infection is the urethra, because this is the mucous membrane most likely to be exposed to the bacteria during sexual intimacy.
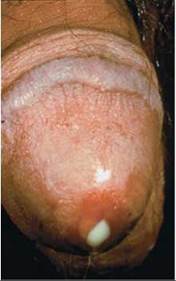
FIGURE 17a.2. A yellowish white discharge from the urethra caused by gonorrhea
In women, chlamydia and gonorrhea are more likely to affect the pelvic organs than the urethra, because the vagina and cervix are a woman's primary sites of contact during sexual intimacy. The general term for an infection of the pelvic organs is pelvic inflammatory disease (PID). The symptoms of PID—abdominal pain or tenderness, lower-back pain, pain during intercourse, abnormal vaginal bleeding or discharge, fever, or chills—can come on gradually or suddenly and vary in intensity from mild to severe.
Pelvic inflammatory disease can be caused by a number of organisms, but the most common culprits are the sexually transmitted bacteria that cause chlamydia and gonorrhea. The bacteria ascend from the vagina through the cervix to the uterus. There, they may infect the endometrium and then spread to the wall of the uterus and to the oviducts. Near the ovary, the oviduct opens to the abdominal cavity, allowing the infection to spread into the abdominal cavity. The infection can be curbed by treatment with antibiotics, which kill the bacteria. Unfortunately, pelvic infections are less likely to produce symptoms than are urinary tract infections, and the untreated infection may permanently damage a female's reproductive system.
Because a man is more likely to experience noticeable symptoms of chlamydia and gonorrhea, men are more likely to seek diagnosis and treatment before the infections have caused lasting damage. However, undiagnosed chlamydia and gonorrhea can have long-term reproductive consequences for both men and women, so it is important that a man who is diagnosed with chlamydia or gonorrhea inform everyone he has been sexually intimate with. If left untreated, Chlamydia and gonorrhea can cause scar tissue to form in the tubes through which gametes travel. If the vas deferens or oviducts are completely blocked by scar tissue, the man or woman becomes sterile. Sterility is more likely to occur in women than in men, because women are less likely to have symptoms that prompt treatment. In a woman, partial blockage of the oviduct may allow the tiny sperm to reach the egg and fertilize it, but the blockage will not allow the much larger embryo to move past the scar tissue to reach the uterus (Figure 17a.3). The embryo may then implant in the oviduct, resulting in an ectopic pregnancy that places the woman's life in danger.
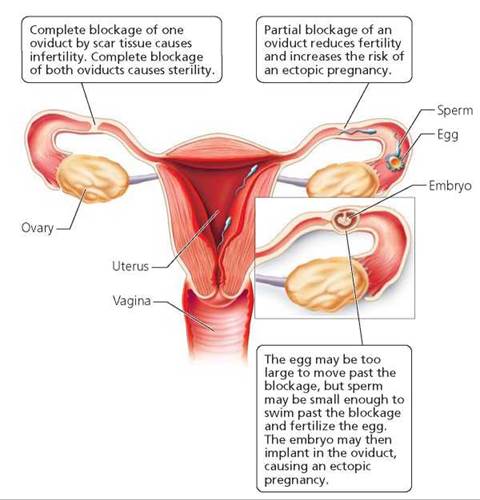
FIGURE 17a.3. Chlamydia and gonorrhea can cause pelvic inflammatory disease, which can cause scar tissue to form in the oviducts.
Chlamydia and gonorrhea are of special concern to pregnant women. Newborns can be infected with either chlamydia or gonorrhea as they pass through an infected cervix or vagina at birth. Chlamydial or gonorrheal infections picked up during birth can affect the mucous membrane of the eye (the conjunctiva), the throat, vagina, rectum, or lungs. These infections are sometimes fatal to an infant. Chlamydial infections during pregnancy place the fetus at risk as well. Specifically, chlamydia can cause the protective membranes around the fetus to rupture early, which can kill the fetus.
Diagnosis of chlamydia and gonorrhea can now be done in a physician's office with quick, accurate tests. Urine tests detect the DNA of Chlamydia or the gonococcal bacterium. Gonorrhea can also be diagnosed by observing the bacterium in a smear of cells taken from the infected area or grown in a laboratory. Both chlamydia and gonorrhea can be cured with antibiotics. Some strains of the gonococcal bacteria are now drug resistant. Therefore, every patient undergoing treatment for gonorrhea must be retested for the bacterium when the antibiotic regimen has been completed to make sure the infection is cured.
Syphilis
Syphilis rates decreased steadily during the 1990s, reaching their lowest point in 2000. Since then, the frequency of syphilis has risen slightly, primarily among men who have sex with men.
Syphilis is caused by a corkscrew-shaped bacterium (a spirochete) called Treponema pallidum. As terrible as these bacteria are, they are extremely delicate and cannot survive drying or even minor temperature changes. A person can contract syphilis only by direct contact with an infected sexual partner. The bacteria can invade any mucous membrane or enter through a break in the skin. The bacteria can also cross the placenta and infect the growing fetus if a pregnant woman is infected.
If untreated, syphilis progresses through three stages. The first stage is characterized by a painless bump, called a chancre (shang'-ker), that forms at the site of contact, usually (but not always) the genitals, and normally appears within 2 to 8 weeks of the initial contact (Figure 17a.4). The chancre appears as a hard, reddish brown bump with raised edges that make it resemble a crater. Unfortunately, a chancre is not always noticed, because it can form in places that are difficult to see and because it may be mistaken for something else. The chancre lasts for one to a few weeks. During that time it ulcerates, becomes crusty, and disappears. The disease, however, has not disappeared.
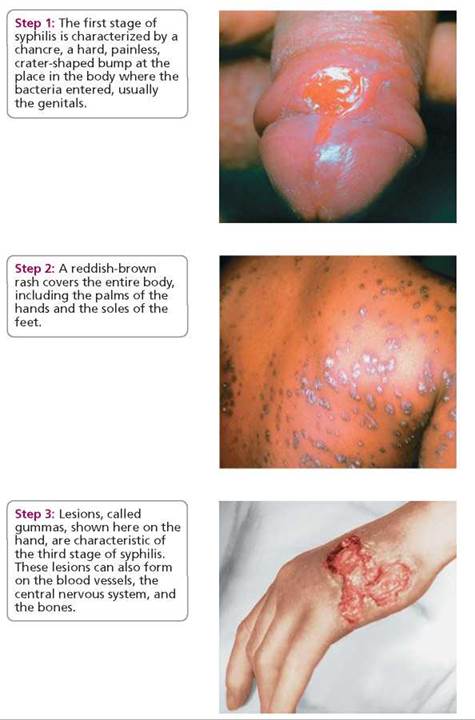
FIGURE 17a.4. Untreated syphilis goes through three stages.
During the primary stage of syphilis, diagnosis is made by identifying the bacterium in the discharge from a chancre. At this stage, syphilis can be treated and cured with an antibiotic such as penicillin.
If syphilis is not detected and treated in the first stage, it can progress to the second stage, which is characterized by a reddish brown rash covering the entire body, including the palms of the hands and soles of the feet. The rash usually appears within a few weeks to a few months after the disappearance of the chancre. The rash does not hurt or itch. Each bump eventually breaks open, oozes fluid, and becomes crusty. The ooze contains millions of bacteria. Therefore, the secondary stage is the most contagious stage of syphilis.
Syphilis in this stage is diagnosed by a blood test to detect antibodies for Treponema bacteria. Second-stage syphilis can be cured with antibiotics such as penicillin, but the disease becomes increasingly difficult to treat as it progresses. Again, the symptoms go away whether or not they are treated. However, in some people, the symptoms recur periodically. Other people may have no outward signs of syphilis for years.
The third stage brings the drama to a grisly conclusion. At this stage, lesions called gummas may appear on the skin or certain internal organs. Gummas often form on the aorta, the major artery that delivers blood from the heart to the rest of the body. As a result, the artery wall may be weakened and may burst, causing the person to bleed to death internally. The bacteria that cause syphilis can also infect the nervous system, damaging the brain and spinal cord, so that the person may have difficulty walking, become paralyzed, or become insane. The disease may also cause blindness by affecting the optic nerve, the iris, and other parts of the eye.
In its third stage, syphilis is very difficult to treat. Treatment requires massive doses of antibiotics over a prolonged period. The damage that has already been done to the body cannot be repaired.
Characteristics of bacterial STDs (their symptoms, diagnosis, treatment, and effects) are summarized in Table 17a.1.
TABLE. 17a.1. Overview of Bacterial STDs
Disease |
Symptoms |
Diagnosis and Treatment |
Effects |
Chlamydia |
First symptoms occur 7-21 days after contact Up to 75% of women and 50% of men show no symptoms Women: Vaginal discharge Vaginal bleeding between periods Pain during urination and intercourse Abdominal pain accompanied by fever and nausea Men: Urethral discharge Pain during urination |
Diagnosis: Urine test for chlamydial DNA Treatment: Antibiotics |
Long-term reproductive consequences such as sterility Infection can pass to infant during childbirth Can cause rupture of the protective membrane surrounding the fetus |
Gonorrhea |
First symptoms occur 2-21 days after contact About 30%-40% of men and women show no symptoms Women: Vaginal discharge Pain during urination and bowel movement Cramps and pain in lower abdomen More pain than usual during menstruation Men: Thick yellow or white discharge from penis Inflammation of the urethra Pain during urination and bowel movements |
Diagnosis: Examination of penile discharge or cervical secretions Urine test for DNA of the bacterium that causes gonorrhea Cell culture Treatment: Antibiotics |
Can cause long-term reproductive consequences such as sterility Infection can pass to infant during childbirth Can cause heart trouble, arthritis, and blindness |
Syphilis |
Stage 1: Occurs 2-8 weeks after contact Chancre forms at site of contact Lymph nodes in groin area swell Stage 2: Occurs 6 weeks to 6 months after contact Reddish brown rash appears anywhere on the body Flu-like symptoms present Ulcers or warty growth may appear Patches of hair may be lost Stage 3: Lesions appear on skin and internal organs May affect nervous system Blindness Brain damage |
Diagnosis: Identification of the bacterium from a chancre Blood test to detect antibodies to the bacterium that causes syphilis Treatment: Large doses of antibiotics over a prolonged period of time |
Infection can pass to fetus during pregnancy Can cause heart disease, brain damage, blindness, and death |
STDs Caused by Viruses
Unlike STDs caused by bacteria, viral STDs cannot be cured with antibiotics. One can treat the symptoms, but one can never be certain that the virus has been eliminated. Therefore, it is always important to take precautions not to pass the virus on to others.
Genital Herpes
Genital herpes is caused by herpes simplex viruses (HSVs). There are actually two types of HSV. They cause similar sores but tend to be active in different parts of the body. Type 1 (HSV-1) is most commonly found above the waist, where it causes fever blisters, or cold sores. Type 2 (HSV-2) is more likely to be found below the waist, where it causes genital herpes on the genitals, buttocks, or thighs. As a result of oral-genital sex with an infected person, however, HSV-1 can cause sores on the genitals, and HSV-2 can cause cold sores (Figure 17a.5).

FIGURE 17a.5. Herpes simplex viruses cause blisters to form at the site of infection.
Herpes simplex viruses are quite contagious and can be spread by direct contact with viruses that are being shed from an infected surface or that are in the fluid on the blisters. Mucous membranes are most susceptible. Skin is a good barrier, unless there is a cut, abrasion, or burn; acne; eczema; or other break.
The first hints of genital herpes infection begin about 2 to 20 days (an average of 6 days) after the initial contact. The initial bout may be severe, often accompanied by fever, aching muscles, and swollen glands in the groin. Soon blisters appear, accompanied by local swelling, itching, and possibly burning, especially if the blisters get wet during urination. The blisters form at the site of contact and last about 2 days before they ulcerate, leaving small, painful sores. At this point individuals infected with genital herpes are at an increased risk of acquiring an HIV infection as well, if they are exposed to the HIV virus.
During dormant periods, the virus retreats to ganglia (clusters of nerve cells) near the spinal cord. Then, at times of emotional or physical stress, the virus may be reactivated and blisters may re-form.
Most people with herpes apparently never develop symptoms, or the symptoms are so mild that they go unnoticed. Nonetheless, these asymptomatic individuals can unwittingly transmit the virus. In fact, most cases of genital herpes are transmitted by partners who never had symptoms or whose symptoms were atypical and undiagnosed! If they had known, they would likely have avoided unprotected sexual contact.
Genital herpes is most contagious when active sores are present, so sexual contact should be avoided during an outbreak. Unprotected contact should be avoided at all times, because genital herpes can also be spread when there are no symptoms.
Most women with herpes have successful pregnancies and normal deliveries. In some cases, however, the infection spreads to the fetus as it is growing in the uterus and can cause miscarriage or stillbirth. HSV can also be transmitted to the newborn during vaginal delivery, especially if active sores are present. To avoid exposing the baby to HSV, physicians often recommend delivery by cesarean section (surgical removal from the uterus) if the mother has active sores.
Clinicians diagnose herpes by examining the sores or by testing the fluid from sores for the presence of the virus. It is also possible to identify the DNA of the herpes virus in the material wiped off when the genital area is gently swabbed. Blood tests can also detect antibodies to the herpes viruses. However, such blood tests may not be useful during an initial attack, because the antibodies may not show up for several months.
Although there is no cure for HSV, there are three antiviral drugs—Zovirax, Famvir, and Valtrex—that help ease symptoms during the initial outbreak and reduce the frequency of recurrences. Unfortunately, strains of HSV that are resistant to antiviral drugs are beginning to crop up.
HPV and Genital Warts
Genital warts may be caused by any of several human papillomaviruses (HPVs). These are not the same viruses that cause warts on the hands and feet. Although chlamydia holds the title of being the most common of all STDs in the United States, HPV is the most common of the viral STDs. Roughly 50% of sexually active people will acquire an infection with HPV at some point in their lives. The body's defense mechanisms usually eliminate HPV without the virus causing serious health problems.
Most people with genital HPV are not aware of the infection, because they don't have any symptoms. However, HPV can be spread by genital contact with an infected person, even when there are no symptoms. Recall from Chapter 13a that viruses replicate in a host cell, and new viruses can be released from the cell slowly, without causing symptoms. The newly released viruses can cause genital HPV on uninfected areas of the same person or on another person if genital contact is made.
There are many strains of HPV. Genital infections with some strains of HPV are considered low-risk infections; these cause genital warts. The warts can be flat or raised and can occur singly or in groups. Without treatment, they often grow in size. Although warts can form in a visible location (Figure 17a.6), they often form in locations where they are not likely to be discovered—the vagina, cervix, or anus. Genital warts are usually diagnosed on the basis of their appearance. However, flat warts are not usually visible unless they are painted with a vinegar-like solution. In women, a Pap test, which looks for precancerous cells on the cervix, is also helpful. A Pap test is a painless test in which the cervix is gently swabbed to collect cells that are then examined for abnormalities under a microscope.

FIGURE 17a.6. Genital warts on the penis
Treatments for genital warts are intended to kill the cells that contain the virus. Methods for removing genital warts include (1) freezing (cold cautery), (2) burning with an electrical instrument (hot cautery), (3) laser (high-intensity light), (4) surgery, and (5) podophyllin (a chemical that is painted onto the warts and washed off after the prescribed time period, before it burns the skin). Also available are creams that the patient applies to shrink genital warts. The creams work by boosting the body's defense mechanisms against the virus. These treatments may destroy visible warts; but HPV may remain nearby in normal-looking tissue and can cause new warts to form weeks or months after old ones have been destroyed.
Other strains of HPV cause high-risk genital infections, which can persist for long periods of time and are closely linked to both cervical cancer in women and penile cancer in men. HPV is thought to be responsible for one-third of all cases of penile cancers in the United States, and it can be isolated in 90% of women with cervical cancer. HPV can also cause anal cancer.
Women should have Pap tests regularly, and those who have ever had HPV should have a Pap test at least once a year. There is now a vaccine that is effective against four HPVs, including two strains that are responsible for most cases of cervical cancer. Health advisors recommend that girls be vaccinated when they are 10 to 12 years old. There is no equivalent vaccine available for men.
The characteristics of genital herpes and genital HPV, both caused by viruses, are summarized in Table 17a.2.
TABLE 17a.2. Overview of Viral STDs
Disease |
Symptoms |
Diagnosis and Treatment |
Effects |
Genital herpes |
First symptoms appear 2-20 days after contact Many people have no symptoms Flu-like symptoms present Small, painful blisters that can leave painful ulcers appear Blisters go away but the virus remains Symptoms recur periodically |
Diagnosis: Examination of blisters Laboratory test on the fluid from the sore to detect the presence of the virus Blood test for antibodies Treatment: Antiviral drugs can ease symptoms |
Cannot be cured Recurrences of blisters Infection can pass to fetus, causing miscarriage or stillbirth Can cause brain damage in newborns |
HPV genital infection |
First symptoms appear 1-6 months after exposure; presence of symptoms depends on type of HPV Small warts appear on sex organs May cause itching, burning, irritation, discharge, bleeding |
Diagnosis: Appearance of growth In women, Pap test may help Treatment: For removal: freezing, burning, laser surgery |
Formation of additional warts Closely associated with cervical cancer and penile cancer Infection can pass to infant during childbirth |
What would you do?
Do you think that you should be permitted to file a lawsuit against someone for transmitting an STD? Why or why not? If you were a juror in such a lawsuit, what factors would influence your decision?
HIV/AIDS
In the past several decades, acquired immune deficiency syndrome, or AIDS, has left its mark on many aspects of society, including medicine, science, law, economics, and education. The name of the condition is apt, because the symptoms are those associated with a damaged immune system. Unlike many other immune deficiencies, however, AIDS is not inherited but acquired. A syndrome is a set of symptoms that tend to occur together, and people with AIDS experience a devastating set of symptoms.
We now know that a virus, the human immunodeficiency virus (HIV), causes AIDS. However, as we will learn shortly, AIDS is actually the final stage in an HIV infection during which the immune system is slowly weakened. A primary target of HIV is helper T cells, which serve as the main switch for the entire immune response (see Chapter 13). Once HIV enters a helper T cell, the T cell stops functioning well, although this cessation of function is not immediately apparent. HIV will eventually kill the infected helper T cell. The infection and eventual death of helper T cells cripple the immune system, giving disease-causing organisms that routinely surround us the opportunity to cause infection. These are the opportunistic infections that characterize AIDS and, in time, cause death.
Global Pandemic
According to the World Health Organization (WHO), toward the end of 2009, an estimated 31.1 to 35.8 million people globally were living with an HIV infection. Africa is currently the area hardest hit by HIV: Two-thirds of the people living with HIV are in sub-Saharan Africa. There are now more people living with HIV than ever before, but because of antiretroviral therapy, the number of new HIV infections has dropped 17% since 2001.
Form of HIV
The genetic material in HIV is RNA. The RNA, along with several virus-specified enzymes, is encased in a protein coat. The RNA and protein coat constitute the core of the virus (Figure 17a.7).
Surrounding the protein coat is an outer covering, or envelope, consisting of spikes of protein embedded in a lipid membrane. The lipid membrane is actually a piece of plasma membrane stolen from the previous host cell and altered for use by the virus. The protein spikes of the viral envelope are responsible for binding the virus to the host cell.
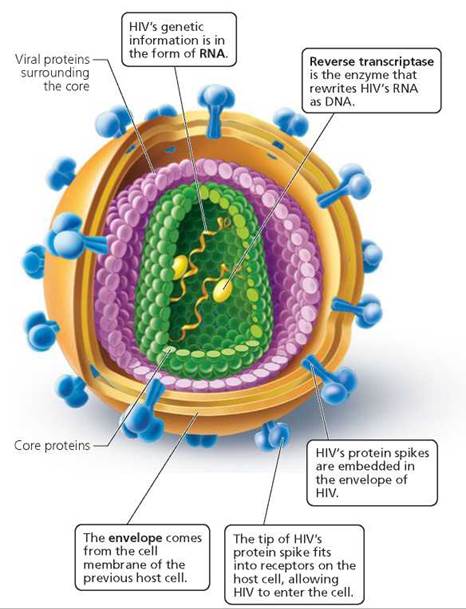
FIGURE 17a.7. The structure of HIV (human immunodeficiency virus)
Replication of HIV
HIV binds to an uninfected cell when the spherical region at the end of a protein spike fits into a receptor on the host cell surface—like a key in a lock. The host cell receptor is a surface protein called CD4. Helper T cells are the predominant cell types with these CD4 receptors and are therefore the most common targets of HIV. When an HIV spike is properly docked in a CD4 receptor, the contents of the virus enter the host cell (Figure 17a.8).
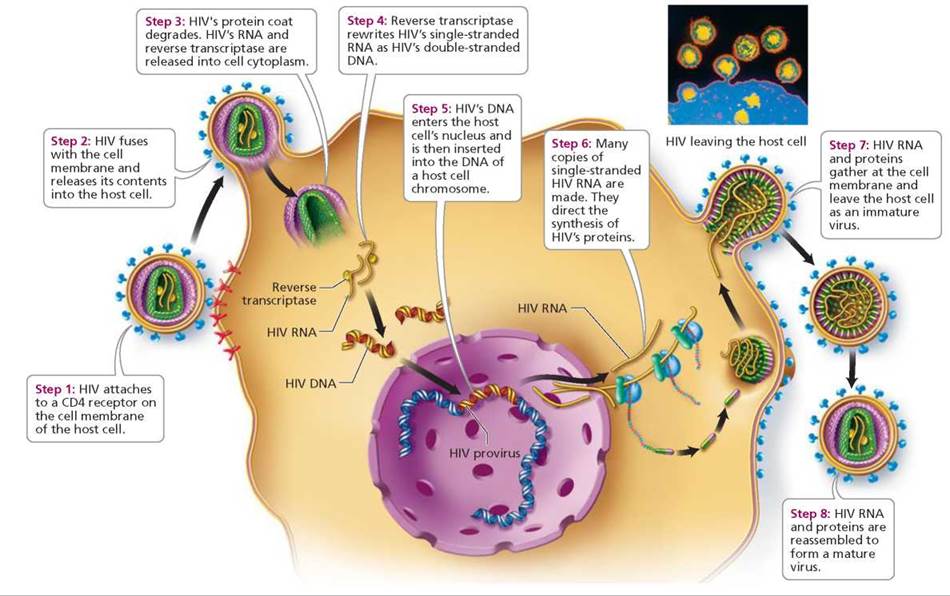
FIGURE 17a.8. The life cycle of HIV
Why is the insertion of HIV DNA into the host cell chromosome so important to HIV's replication?
If HIV DNA is not inserted into the host cel! chromosome, it cannot produce HIV RNA or HIV-specified proteins.
Once within the host cell, the RNA of HIV undergoes a process called reverse transcription. During this process, the viral RNA is rewritten as double-stranded DNA. Because going from RNA to DNA is the reverse of the usual genetic information transfer, viruses that work this way are known as retroviruses (retro-, backward). The backward copying of genetic information from RNA into DNA is performed by an enzyme called reverse transcriptase, which is inserted into the host cell along with viral RNA.
The newly formed viral DNA, which contains all the instructions necessary for producing thousands of new viruses, is then spliced into the host DNA. Once HIV's DNA is integrated into the host cell chromosome, that DNA is called the HIV provirus. After they have been incorporated into the host cell DNA, the host cell treats the HIV genes as it would its own. Each time the cell reproduces, the viral DNA is copied along with the cell's DNA. When HIV is transmitted to another person, it is usually in the form of a latent—that is, inactive—HIV provirus when the infected cell enters the other person's body.
The HIV genes can reside in a helper T cell chromosome for years, until the cell is activated to respond to some foreign antigen, such as another kind of virus, a fungus, or a parasite. At this point, the virus begins making copies of itself instead of allowing the cell to fight the invader. The viral genome is activated and turns the cell into a virus factory. Some of the newly produced HIV RNA will become genetic material for new viruses, and some will be used to produce virus-specified proteins. The viral components gather at the cell membrane and bud off from the host cell. The HIV RNA and proteins then self-assemble into new, mature viruses, which move through the bloodstream to infect new cells.
Transmission of HIV
HIV is found in bodily fluids—blood, semen, vaginal secretions, breast milk, saliva, tears, urine, cerebrospinal fluid, and amniotic fluid. However, HIV is not easily transmitted. Only the first four of the bodily fluids listed contain HIV concentrations high enough to cause infection in another person. HIV cannot be transmitted by casual contact. The major modes of transmission are as follows:
• Unprotected sexual activity. HIV can be transmitted through unprotected sexual activity of any kind—that is, activity in which skin or mucous membranes of the vagina, vulva, penis, mouth, or anus of the partners are not separated by a barrier (i.e., a latex condom) that the virus cannot penetrate.
• Intravenous drug use. Contact with infected blood is another way that HIV can be transmitted. Since 1985, all blood donated to blood banks is tested for HIV; this testing has essentially eliminated the risk of getting HIV from a blood transfusion. However, intravenous drug users who share needles do have an increased risk of HIV infection.
• Infected mother to offspring before, during, and after birth. HIV can be transmitted from an infected mother to her offspring across the placenta during prenatal development, during delivery, or in breast milk during nursing. An HIV-infected woman who is not treated for HIV during pregnancy and does not breast-feed her infant has about a 25% chance of spreading HIV to her newborn. However, if the mother is treated with drugs that slow replication of HIV (antiretroviral drugs), she has less than a 2% chance of transmitting the virus to her newborn.
Stop and think
Hospitals do not isolate patients with HIV unless they have another infectious disease. Why is this a safe practice?
Sites of HIV Infection
HIV can infect any cell that has a CD4 receptor. The most important of these cells is the helper T cell, which turns on the entire immune response (see Chapter 13). The hallmark of an HIV infection is a progressive decline in helper T cell numbers. This loss is devastating because it leaves the body increasingly defenseless against other infections.
HIV can also infect the brain, killing nerve cells. When the brain is infected, the symptoms can include forgetfulness, impaired speech, inability to concentrate, depression, seizures, and personality changes. Roughly 60% of people with AIDS have signs of dementia.
Stages of HIV Infection
An HIV infection usually progresses through a series of stages: the initial infection, an asymptomatic stage, initial disease symptoms, early immune failure, and AIDS. The progress of an HIV infection is usually monitored by following both the decline in the number of helper T cells and the increase in viral load (the number of HIV free in the blood). The changes in T cell number and viral load are summarized in Figure 17a.9.
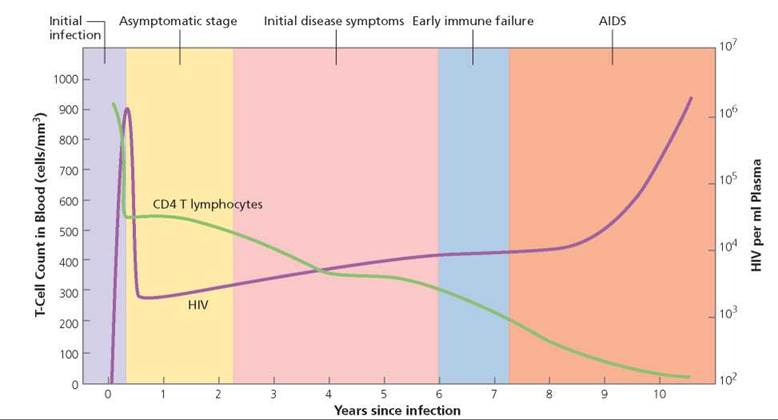
FIGURE 17a.9. An HIV infection can be monitored by following the decline in the number of T cells and the rise in viral load (number of viruses in the bloodstream).
Initial infection. During the initial stages of infection, the virus actively replicates, and the circulating level of HIV rises. The body's immune system produces antibodies against the virus in an attempt to eliminate it. Antibodies can usually be detected within 8 weeks or so, but in some cases they are not detected for many months or even years. An HIV test looks for the presence of antibodies to HIV in the blood. If antibodies are found, the person is said to be HIV positive (HIV+).
Many people have no symptoms when they first become infected; others experience some mild disease symptoms during the initial infection. Early symptoms might include enlarged lymph nodes throughout the body, fatigue, and fever. If the brain becomes infected, the initial symptoms may include headaches, fever, and difficulty concentrating, remembering, or solving problems. This initial stage is particularly dangerous, because even though many people are unaware they are infected at this point, they are particularly contagious.
Asymptomatic stage. Weeks to months after the initial stage of infection, the person usually feels well again, often for several years. This is the period of asymptomatic infection. During this stage, the immune system mounts a defense strong enough to control, but not conquer, the infection. The rate of helper T cell production increases. For a while, helper T cell production matches destruction.
During the asymptomatic stage, HIV is far from idle. It is "hiding out" in certain lymphatic organs, including the spleen, tonsils, and adenoids, but most importantly in the lymph nodes, where it replicates. Consequently, the spaces between cells in the lymph nodes become packed with virus particles. Most helper T cells reside in the lymph nodes, and many of them have the DNA form of HIV genes incorporated into their own chromosomes. Because helper T cells frequently circulate through the lymph nodes, this is an opportune place for HIV to encounter healthy T cells. Thus, millions of T cells become infected as they move through the lymph nodes on their way to other parts of the body.
Initial disease symptoms. Eventually, the immune system begins to falter as the virus gains the upper hand. As helper T cell numbers gradually drop, symptoms set in again. The initial disease symptoms fall into three classes.
1. Wasting syndrome is characterized by an otherwise unexplained loss in body weight of more than 10%, often accompanied by diarrhea. The weight loss is similar to that experienced by a cancer patient.
2. Swollen lymph nodes occur in the neck, armpits, and groin. These structures may remain swollen until later stages of HIV infection.
3. Neurological symptoms may appear, either because HIV has spread to the brain or because other organisms have caused a brain infection. Among the neurological symptoms are dementia, weakness, and paralysis caused by spinal cord damage. Other symptoms include pain, burning, or a tingling sensation, usually in hands or feet, caused by peripheral nerve damage.
Early immune failure. As T cell numbers continue their gradual decline, the body becomes increasingly vulnerable to infection. Early signs of immune failure include thrush (a fungal infection in the mouth) and shingles (a painful rash caused by the same virus that causes chickenpox).
AIDS. AIDS is the final stage of an HIV infection. The time from HIV infection to diagnosis of AIDS can be 10 or more years, depending on the number of other infections the person is exposed to and the health of the immune system before infection with HIV. Now, although the body has fought long and hard, it is beginning to lose the battle. The immune system is crippled, making the person vulnerable to certain characteristic fungal, protozoan, bacterial, and viral infections, as well as cancers.
A diagnosis of AIDS is made when an HIV+ person develops one of the following conditions: (1) a helper T cell count below 200/mm3 of blood; (2) one of 26 opportunistic infections, the most common of which are Pneumocystis jiroveci pneumonia and Kaposi's sarcoma, a cancer of connective tissue that primarily affects the skin; (3) a greater than 10% loss of body weight (wasting syndrome); or (4) dementia.
Treatments
Death in a person with AIDS is usually caused by one of the opportunistic infections. Thus, treating opportunistic infections, or preventing their onset, can improve the quality of life and extend the length of life for people with AIDS. Treatment for HIV infection is also aimed at slowing the progress of the infection, both before and after the diagnosis of AIDS. The current prevailing strategy is to slow the rate at which HIV can make new copies of itself. At present, there are five classes of drugs that slow viral replication: reverse transcriptase inhibitors, protease inhibitors, fusion inhibitors, HIV entry inhibitors, and inhibitors of HIV DNA integration into the host cell chromosome. Each class of drug prevents HIV from replicating by blocking a different step in the virus replication cycle.
The original class of antiviral drugs used to slow the progression of an HIV infection consisted of drugs that act on reverse transcriptase (AZT, ddI, ddC). As discussed earlier, reverse transcriptase is the enzyme necessary for converting the RNA of HIV to DNA that can then be inserted into the DNA of the host cell chromosome.
A second class of antiviral drugs consists of protease inhibitors. Recall that after the HIV genetic information has been inserted into the DNA of the host cell, it can begin producing proteins needed to form new copies of HIV. The proteins initially produced are too big to be used and must be cut to the proper size by an enzyme called a protease. Protease inhibitors block the action of this enzyme, preventing a necessary step in the preparation of proteins for the assembly of new viruses.
A treatment called highly active antiretroviral therapy (HAART), also known as a drug cocktail, consists of combinations of drugs. Typically, the cocktail contains two inhibitors of reverse transcriptase and a protease inhibitor. The idea behind this drug combination is that a protease inhibitor will slow the rate of formation of new viruses. If HIV becomes resistant to inhibitors of reverse transcriptase, the protease inhibitor will prevent the assembly of HIV components into new viruses. Thus, the development of resistance to the other drugs will be minimized. Combination drug treatments are prolonging the lives of HIV-positive individuals. HAART can reduce the viral load to undetectable levels, but the treatment is not a cure. If treatment is stopped, HIV can leave the latent state and begin actively replicating again.
There are newer classes of antiviral drugs. Fusion inhibitors block the proteins on the surface of HIV that bind to the CD4 receptor on host cells, thereby blocking HIV from entering the host cell. Integrase inhibitors prevent HIV DNA from inserting itself into the host chromosome.
Stop and think
The drugs used to combat HIV effectively stop or slow HIV replication, but they are not effective against HIV when it is incorporated into the host cell chromosome. How does this explain why the treatment must be continued for life?
A variety of other approaches to combating an HIV infection are under active investigation. Clearly, though, the best way to fight the devastation caused by HIV is to prevent it from establishing the initial infection. Currently, the best way to do this is to avoid high-risk behaviors such as unprotected sex or intravenous drug use. Theoretically, prevention of HIV infection could also be accomplished by developing a vaccine similar to those for other viral infections such as smallpox and measles. Recall from Chapter 13 that vaccines work by causing a person's body to produce antibodies against the organisms that cause a disease, without actually causing the disease. Unfortunately, HIV has several characteristics that have thwarted efforts to develop a vaccine:
• The mutation rate in HIV is very high, especially for the proteins in its outer coat, which are the proteins that an antibody would have to recognize.
• There are two types of HIV and many strains of each type. Antibodies would have to recognize the exact strain entering the body.
• An HIV infection is latent when its genetic material has become incorporated into the host DNA (as a provirus). Antibodies cannot attack the virus while it is hidden within the host cell.
• HIV can pass directly from the interior of an infected cell to the interior of an adjacent uninfected cell. Antibodies can attack viruses outside the cell only; they cannot prevent the virus from spreading by this means of transmission.