Biology of Humans
18a. Autism Spectrum Disorders
In Chapter 18 we examined human development, with a focus on the prenatal period. In this chapter, we examine autism spectrum disorders, lifelong developmental disorders that are usually diagnosed in early childhood. We look at their symptoms and possible causes. We also consider how these disorders are diagnosed and treated. Finally, we explore the fear that childhood vaccines are linked to the onset of autism.
Characterization and Prevalence
Autism (also called autistic disorder) is a neurodevelopmental disorder characterized by impaired communication skills, poor social interactions, and unusual behaviors. It has many of the same symptoms as pervasive developmental disorder not otherwise specified (PDD-NOS) and Asperger syndrome (sometimes called Asperger's disorder), so these three developmental disabilities are classified together as autism spectrum disorders (ASDs). Symptoms of ASDs begin in early childhood (for autism, the onset criterion is before the age of 3) and last a lifetime. The disorders are quite common: the Centers for Disease Control and Prevention (CDC) estimates that about 1 in 110 children in the United States has an ASD. ASDs cross racial, ethnic, and socioeconomic lines, and they are four times more common in boys than girls. Estimates of the prevalence of ASDs have increased in recent decades, but the meaning of this increase is unclear. Some believe that the apparent increase in prevalence does not represent a true increase in number of cases, but rather increased awareness and recognition of the disorders as well as improved and expanding diagnostic criteria. ASDs are associated with other medical conditions, including Fragile X syndrome and untreated phenylketonuria (see Chapter 20), although these represent a minority of ASD cases.
· This boy has autism, a developmental disorder characterized by impaired communication, poor social skills, and unusual patterns of behavior.
Autism was first described as a disorder in 1943 by Leo Kanner, an Austrian-born physician who immigrated to the United States. In 1944, Hans Asperger, an Austrian physician who remained in his country of birth, independently published his observations of children who were similar in many ways to those described by Kanner, except that they functioned at a higher cognitive level (Figure 18a.1). Asperger was the first to describe the symptoms of the disorder that would later be named for him. Children with Asperger syndrome have impaired communication and poor social and motor skills, but they can be intellectually gifted. In fact, Asperger termed them "little professors" because of their ability to speak at length about their favorite topic, be it opera, astronomy, or fossil fishes. Asperger's work was published in German, and it did not reach English-speaking audiences until the 1980s when English psychiatrist Lorna Wing, herself the mother of an autistic child, highlighted his work in one of her academic papers. PDD-NOS was formally defined in 1987 and describes individuals who have severe impairment in communication and social skills or who exhibit stereotyped behavior but do not meet the full criteria for autism, Asperger syndrome, or psychiatric disorders such as schizophrenia. Because some, but not all, of the features of another explicitly defined developmental or psychiatric condition are present, PDD-NOS is said to be a subthreshold condition. Current definitions of all three ASDs are based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), a handbook that is widely used by psychologists and psychiatrists to classify mental disorders. The handbook is published and regularly updated by the American Psychiatric Association; the fifth edition is expected in 2013.
FIGURE 18a.1. The symptoms of autism and Asperger syndrome were formally described by Austrian-born physicians in the 1940s.
Symptoms
Symptoms of ASDs include marked deficits in communication and social skills and the performance of unusual and repetitive motor patterns (Figure 18a.2). Although there is considerable overlap in diagnostic criteria for autism and Asperger syndrome, there are some differences (Table 18a.1). At one end of the spectrum, some people with autism are profoundly challenged intellectually; at the other end, some with Asperger syndrome are intellectually gifted. Some people with autism never speak, while some with Asperger syndrome speak at length, but in onesided conversations. In fact, whereas the diagnostic criteria for autism include having either a clinically significant delay in language or no speech at all, Asperger syndrome is defined as having no clinically significant general delay in language or cognitive development (cognitive development is not characterized in the diagnostic criteria for autism). Even within the three categories of ASDs set forth in the DSM-IV-TR, there is tremendous variation in the presence and intensity of symptoms.
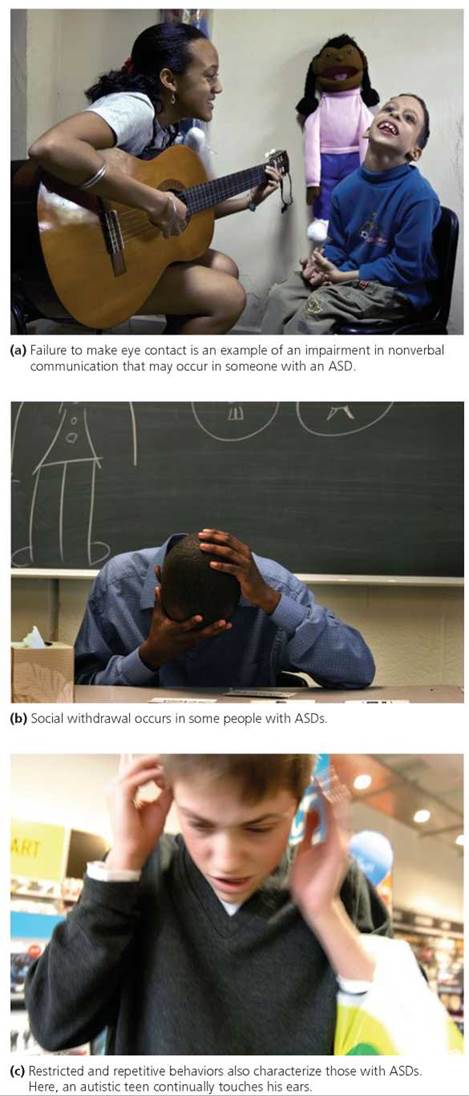
FIGURE 18a.2. Autism spectrum disorders (ASDs) are characterized by impaired communication (verbal and nonverbal), poor social skills, and the performance of unusual behaviors.
Because autism, Asperger syndrome, and PDD-NOS share many symptoms and because there is continuing debate regarding their clinical boundaries, we provide a general description of symptoms for this group of disorders as a whole and note where symptoms are specific to autism or Asperger syndrome. Some ASD symptoms can be present in people with other medical conditions (for example, people with Fragile X syndrome may either meet the full criteria for autism or only show some symptoms of autism). Some of the symptoms can also be present in people who do not have an ASD or another medical condition. For example, some normally developing toddlers may go through a brief period during which they flap their hands when excited or frustrated—a behavior that is typical of some autistic children. Hand flapping tends to occur when normally developing toddlers are incapable of fully expressing themselves through speech; when they become more fluent in speech, they stop flapping their hands. In contrast, the stereotyped behaviors characteristic of some individuals with ASDs (for example, hand flapping, rocking, and twirling) often extend well beyond the toddler years and can occur with such regularity and for such prolonged periods that they interfere with other activities.
Stop and think
Tantrums are not unusual in normally developing toddlers. What would you predict regarding timing and severity of tantrums in children with ASDs?
Communication
Verbal communication skills of people with ASDs vary dramatically. About 40% do not speak at all; about 25% use some words and then lose them between 15 and 24 months of age. Other people with ASDs exhibit delays in speaking or develop speech at the appropriate time but speak with impaired use of language and poor social skills. Complete absence of speech, found in some autistic children, does not characterize children with Asperger syndrome. Children with Asperger syndrome may exhibit mild delays in speech, and their atypical language development (especially in the social use of language) may go unnoticed until preschool or somewhat later, when their inability to form friendships becomes apparent. People with ASDs may find the give-and-take of normal conversation difficult, and they may interrupt or continue talking too long on a subject of particular interest to them; some also use an odd tone of voice. Difficulties in conversation are very characteristic of individuals with Asperger syndrome, but may also occur in individuals with PDD-NOS or high-functioning autism.
TABLE 18a.1. Diagnostic Criteria for Autism and Asperger Syndrome
Areas of Impairment (Number of Symptoms Required for Diagnosis*) |
Symptoms |
Autism |
Asperger Syndrome |
Communication (at least one symptom from list for autism) |
No spoken language or delay in development of language |
X |
|
In those who speak, marked impairment in ability to converse with others |
X |
|
|
Use of stereotyped, repetitive, or idiosyncratic language |
X |
|
|
Lack of social imitative play or spontaneous imaginative play |
X |
|
|
Social interaction (at least two symptoms from list for autism and Asperger syndrome) |
Marked impairment in ability to regulate social interactions through nonverbal behaviors such as gestures, eye contact, and facial expressions |
X |
X |
Failure to develop age-appropriate relationships with peers |
X |
X |
|
Lack of spontaneous sharing of interests or experiences with others |
X |
X |
|
Lack of social or emotional reciprocity |
X |
X |
|
Restricted, repetitive, and stereotyped patterns of behavior (at least one symptom from list for autism and Asperger syndrome) |
Persistent preoccupation with stereotyped and restricted patterns |
X |
X |
Inflexible adherence to specific, nonfunctional rituals or routines |
X |
X |
|
Stereotyped or repetitive motor behavior, such as rocking or hand flapping |
X |
X |
|
Persistent preoccupation with parts of objects |
X |
X |
Modified from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), (American Psychiatric Association, 2000).
*A diagnosis of autism requires a total of six (or more) items from the three areas of impairment, with the minimum required from each area of impairment shown in parentheses in the first column. A total number of required items is not part of the diagnostic criteria for Asperger syndrome.
Using and understanding nonverbal communication also pose problems for people with ASDs. In some cases, their facial expression is disconnected from their words; for example, they may smile when describing an extremely sad or frightening experience. Some have difficulty making eye contact, while others stand too close to the person they are speaking with. The ability to notice and understand the facial expressions and body language of others also may be poorly developed.
Social Skills
Impairments in communication are often associated with impairments in social skills. For example, an individual with an ASD who has trouble listening to others and engaging in the give-and-take of conversation will likely experience difficult social interactions. Inability to imitate the actions of others is characteristic of people with ASDs; this is a major disadvantage because imitation is an important way that young children learn how to speak and act in social situations. As a result, some individuals with ASDs say whatever comes to mind, whether it is appropriate or not. Some people with ASDs may not want to interact with other people at all. Others may pursue social interactions but have difficulty forming and maintaining social relationships because of their impaired ability to communicate and to interact.
Adapting to changes in daily schedules can be challenging to those with ASDs; some may collapse in a severe and prolonged tantrum when a daily routine changes. These outbursts may frighten others or, at the very least, make them uncomfortable and less likely to engage in social interaction. Finally, other behavioral conditions frequently found in children with ASDs—such as impulsivity, hyperactivity, aggressiveness, self-injurious behavior, and atypical responses (over- or underreaction) to sensory stimuli such as touch, pain, smell, and sound—can further compromise social interactions.
Motor Patterns and Behavior
As noted earlier, repetitive movements, such as flapping the hands, can occur with ASDs. In children, the repeated actions may involve toys (for example, spinning the blades of a toy helicopter close to the eyes) or other objects (for example, repetitively turning lights on and off or opening and closing a door). These repetitive motor activities are called self-stimulatory activities, and they too make social interaction difficult. In addition to these repetitive movements, people with ASDs may exhibit poor motor coordination. Motor clumsiness is viewed by many as a distinguishing feature of Asperger syndrome, although it is not currently listed as a defining characteristic by the DSM-IV-TR.
Some people with ASDs develop unusual rituals, such as touching several objects in succession and in precise order before leaving home. While these rituals may seem odd or unnecessary to observers, they can be very important to the person performing them. Indeed, disrupting or preventing these rituals can cause extreme frustration and tantrums. Preoccupation with parts of objects and all-consuming interests also characterize ASDs. Some may be fixated on certain topics, such as train or tide timetables, that they talk about incessantly.
Timing of Symptom Development
Although symptoms of ASDs usually become apparent in the first few years after birth, the underlying neurological defects are thought to occur early in embryonic development. About 30% to 50% of parents of children with ASDs notice problems during the first year; 80% to 90% notice problems by 2 years of age. As mentioned previously, Asperger syndrome may be noticed later than autism because there are no clinically significant overall delays in speech and cognitive development. Nevertheless, most parents of a child with Asperger syndrome notice by the child's third birthday that there is something unusual about their child; some symptoms may be apparent in infancy. It is worth noting that some children with autism develop certain communication, social, and motor skills on time and then subsequently lose them.
Diagnosis
Diagnostic criteria for ASDs have changed several times in recent decades. These changes are reflected, in part, in the multiple editions of the DSM. A key change occurred in DSM-III, issued in 1980, when autism was formally differentiated from schizophrenia as a developmental disorder rather than a psychiatric one, and specific criteria for autism were listed. Later editions of the DSM included modified criteria for autism and specifically listed as disorders PDD-NOS (DSM-III Revised, 1987) and Asperger syndrome (DSM-IV, 1994). Today, physicians begin to consider a diagnosis of ASD when a child fails to meet age-specific developmental milestones.
Children differ in the pace at which they develop. Nevertheless, there are age-specific developmental milestones to which their progress can be compared to identify delays (see Figure 18a.3 and Table 18a.2). Identifying developmental delays is important because early diagnosis of an ASD can lead to early intervention, which can benefit the child. To this end, pediatricians and nurses routinely conduct developmental screening of infants and young children at their periodic physical examinations. In addition to asking the parents questions about their child's development, these health care professionals directly interact with the child to see how the child reacts, speaks, and moves (Figure 18a.4). If delays are noted, then the parents may be advised to seek the opinion of a developmental pediatrician or psychologist, and additional screening may be performed. This screening typically involves several of the following diagnostic tools: extensive interviews of the parents regarding their child's developmental history; detailed records from the pediatrician; clinical observations of the child's behavior; psychological testing; speech, language, and hearing assessments; and physical and neurological examinations.
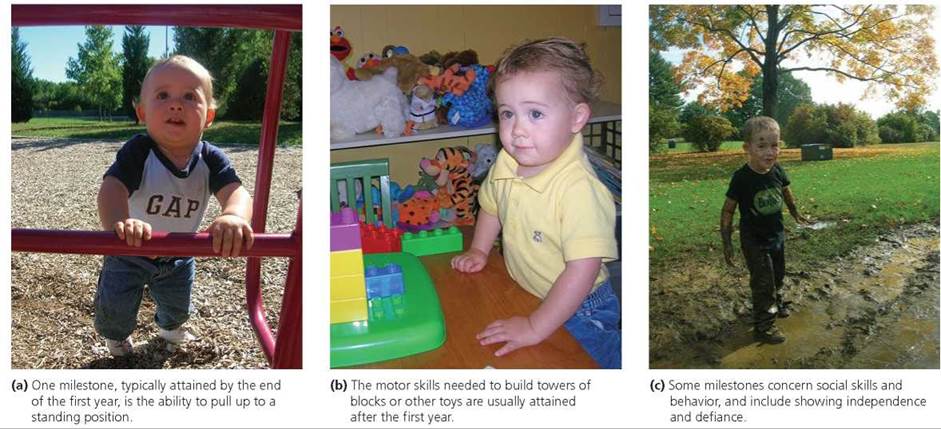
FIGURE 18a.3. The pace at which a young child develops can be viewed in the context of age-specific developmental milestones. Shown here is the same child at 10 months, 20 months, and nearly 3 years of age.
TABLE 18a.2. Some Developmental Milestones Used to Assess a Young Child’s Progress in the Areas of Communication, Social Behavior, and Motor Skills
Age |
|
Developmental Milestones |
|
|
Communication |
Social Behavior |
Motor Skills |
By the end of the first year |
Babbles with changes in tone Tries to imitate words Uses simple gestures and single words |
Is shy with strangers Repeats gestures for attention Tests parental responses to behavior |
Reaches sitting position without help Crawls forward on belly Pulls self to standing position |
By the end of the second year |
Uses simple phrases and several single words Points to named objects Repeats words heard in conversation |
Imitates behavior of others Shows independence and defiance Shows some self-awareness |
Walks independently and begins to run Kicks a ball Pulls or carries a toy while walking |
By the end of the third year |
Recognizes and identifies common objects Uses sentences with 4 or 5 words Speaks such that strangers can understand most words |
Spontaneously shows affection Takes turns in games Separates from parents with relative ease |
Runs with ease Pedals a tricycle Builds a tower of more than six blocks |
*More complete lists of developmental milestones can be found at www.cdc.gov/ncbddd/autism/actearly/screening.

FIGURE 18a.4. Routine developmental screening at periodic visits to the pediatrician can help identify developmental delays or losses.
Why does developmental screening play such an important role in diagnosing ASDs? Is there a medical test for these disorders?
There is no medical test (e.g., blood test or scan of the brain) forASDs; instead, doctors rely on several tools to assess behavioral symptoms. Typically, delays detected during routine developmental screening are further evaluated through parent interviews, psychological testing, and assessments of speech, language, and hearing.
Several diagnostic checklists and rating scales for diagnosing ASDs are available. Some differentiate children at risk of having an ASD from the general population. For example, the Checklist for Autism in Toddlers (CHAT) is used with children aged 18 to 24 months. The Childhood Asperger Screening Test (CAST) can be administered to children aged 4 to 11 years. Other screening tools, such as the Gilliam Autism Rating Scale (GARS) and the Gilliam Asperger's Disorder Scale (GADS), differentiate individuals with autism and Asperger syndrome, respectively, from those with other developmental disorders. GARS and GADS are used with individuals from 3 to 22 years of age, and they can be completed by a parent, teacher, or clinician.
Results from screening can be used by a trained clinician, together with other diagnostic tools, to consider an ASD diagnosis. Recent advances include the development of new standardized assessment tools for children under 24 months of age.
Stop and think
Screening tools have not proven particularly effective in distinguishing PDD-NOS from other developmental disorders. Why might PDD-NOS be difficult to distinguish?
Possible Causes
In the years following its formal description in 1943, autism was thought to be caused by aberrant parenting, an idea initially put forth by Leo Kanner. According to the "Refrigerator Mother" hypothesis, a cold, uncaring parent (usually the mother) caused the child to retreat into autism. It was not until the mid-1960s that this hypothesis was directly attacked and replaced with the view that autism is a neurodevelopmental disorder with a genetic basis. Autism cannot be linked to any particular parenting style.
Although we now know that autism and other ASDs are not caused by aberrant parenting, we still do not know their precise causes. Most researchers agree that there are probably multiple causes and that genes and environment play a role.
Some research has focused on the neurobiological basis of ASDs. Neuroimaging studies and studies of brain tissue from people with ASDs indicate fundamental differences from controls in brain growth and organization. Many of these differences probably originate in the prenatal period. For example, abnormal migration of cells during formation of the nervous system may affect brain structure and neural circuitry, and ultimately influence thinking and behavior. Imaging the brain during cognitive tasks or response to visual or auditory stimulation suggests that people with ASDs use different cognitive strategies and may process certain types of information in different brain areas. A particularly consistent finding of neuroimaging studies is that people with ASDs display underactivation of the part of the brain involved in face recognition. Despite these advances in identifying structural and functional differences in the brains of those with ASDs, a reliable marker for these disorders has yet to be identified; for this reason, routine neuroimaging is not recommended as a diagnostic tool.
Two main types of studies indicate that autism has a strong genetic component. First, family studies show higher than expected rates of autism among family members. For example, the rate of recurrence of autism in siblings of autistic individuals is 2% to 6%, which is 10 to 60 times greater than the prevalence of autism in the general population. Second, studies of twins demonstrate that autism has a genetic basis.
Recall from Chapter 18 that dizygotic (fraternal) twins occur when two secondary oocytes are fertilized by different sperm; these twins are no more genetically similar than siblings who are not twins. Monozygotic twins result from the splitting of a pre-embryo and are nearly genetically identical. (We say "nearly" here because new research has shown that while identical twins have very similar DNA, they do not have identical DNA. Identical twins may differ, for example, in the number of copies of a particular gene. Prior to this discovery, scientists knew that identical twins experience epigenetic changes, which are changes in gene expression induced by environmental factors such as diet. Although epigenetic changes affect the way genes are expressed, they do not reflect changes in the underlying DNA sequence, so this new information about identical twins is very exciting.)
Researchers studying the genetics of autism have compared the incidence of autism in monozygotic and dizygotic twins. If one monozygotic twin has autism, then there is a 75% chance that the other twin will have autism. In contrast, if one dizygotic twin has autism, then there is a 3% chance that the other twin will have autism (note that this falls within the 2% to 6% rate of recurrence among non-twin siblings mentioned previously). These comparative findings indicate a genetic basis for autism because the incidence among twins is higher when they are nearly genetically identical. However, data for monozygotic twins also suggest an environmental component because despite being nearly genetically identical, both twins are not always autistic. These findings suggest that one twin was exposed to environmental factors during the prenatal and/or postnatal period that, in combination with a susceptible genetic background, led to the expression of autism. Although comparable twin studies are not yet available for Asperger syndrome, the disorder does run in families—indicating it, too, has a genetic basis.
It is unlikely that a single gene is responsible for the genetic component of an ASD. Indeed, current models suggest that several genes, perhaps as many as 15, are involved, and that when these genes are present in combination they lead to an increased vulnerability to autism that may be triggered by environmental factors. Research is under way to identify candidate genes and environmental triggers.
Little is known about the environmental risk factors for ASDs. Some research focuses on maternal effects (specifically the intrauterine environment) and complications during pregnancy and birth. Prenatal exposure to certain prescription drugs, such as thalidomide (see Chapter 18) or valproic acid (an anticonvulsant and mood stabilizer), is linked to an increased risk of autism. There is some evidence that maternal illness, such as rubella (German measles), during pregnancy is an environmental trigger for autism. Recent studies indicate an association between infertility treatments (specifically drugs used to induce ovulation) and autism, and the association appears to strengthen with duration of treatment. In other words, the longer a woman is treated for infertility, the higher are her chances of having a child with an ASD. The challenge now is to sort out the roles of many factors— premature delivery, low birth weight, twinning, and maternal age—that are associated with both autism and infertility treatments. One environmental variable that has been suspected— early childhood vaccines—is discussed later in the chapter.
Treatment and Therapy
There are no cures for ASDs, but educational interventions can help children with these developmental disorders reach their full potential. Successful educational programs provide structure, organization, and direction for the child. Such programs directly teach children with ASDs the social skills that other children learn by other means. Given the enormous individual variation in how ASDs are manifested, it is imperative that educational programs are designed for the individual child; to this end, school-age children typically have an Individualized Educational Program (IEP). An IEP is developed and periodically reviewed by a team that typically includes the parents (or guardians), teachers, social workers, school psychologists, and representatives of the school district. An IEP is federally guaranteed under the Individuals with Disabilities Education Act (IDEA), and ensures that a child with an ASD will receive the most appropriate education available. In addition to classroom accommodations, such programs may include speech therapy, occupational therapy (designed to improve social, fine motor, and selfhelp skills), and sensory integration therapy (designed to facilitate development of the nervous system's ability to process external stimuli such as touch, sound, and sight, in more typical ways).
Specific educational interventions may differ for children with different ASDs. For example, the typical difference in verbal abilities between children with autism and children with Asperger syndrome often necessitates different treatment approaches. Those autistic children with little or no verbal ability may be taught to communicate with picture cards, in an approach called the Picture Exchange Communication System (Figure 18a.5). The Picture Exchange Communication System forms the basis for a recently developed computer-based communication tool, Speaks4me. With this new tool, a user selects images and drops them into place along a timeline. When satisfied with the arrangement, the user clicks on an audio icon, and the newly created sentence or phrase is read aloud by a voice, thereby turning images into speech. The better verbal abilities associated with Asperger syndrome mean that counseling and forms of talk therapy can be part of the treatment plan.
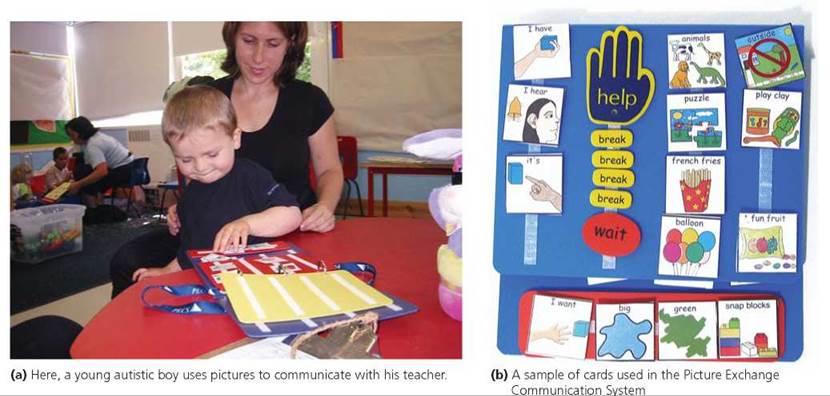
FIGURE 18a.5. The Picture Exchange Communication System is used to help autistic children with limited or no verbal abilities to communicate.
To date, no single therapeutic drug is known to improve core symptoms of ASDs—impairments in communication and social behavior and repetitive or unusual behaviors. Ongoing research holds promise. One candidate drug is oxytocin, a hormone released by the posterior pituitary gland (see Chapter 10). Oxytocin promotes uterine contractions during childbirth, prompts milk letdown during lactation, and enhances social bonding. A small study published in 2010 showed that adults with either Asperger syndrome or high-functioning autism were more likely following treatment with oxytocin delivered in a nasal spray to focus on the eyes when viewing pictures of human faces. Other measures of social function also improved. Several drugs are used with limited to moderate success to treat behavioral features that often accompany ASDs. For example, the Food and Drug Administration approved the use of the antipsychotic drug risperidone in children with ASDs who display severe tantrums, aggression, or self-injurious behavior. Still other drugs may be prescribed to treat hyperactivity, impulsivity, and anxiety often present in children with ASDs.
The prognosis for individuals with ASDs depends on many factors. In general, for children, better outcomes are associated with better verbal and cognitive abilities, less severe symptoms overall, and early identification of the disorder and appropriate intervention programs. The outcomes for adults with ASDs correlate best with cognitive abilities; those with at least normal intelligence have the best outcomes.
What would you do?
Some parents use practices and products outside of conventional medicine to relieve their child's ASD symptoms. Known as complementary and alternative medicine, these treatments include dietary therapies—such as removing from the child's diet the proteins gluten (found in wheat) and casein (found in dairy products)—and deep pressure therapy (for example, use of a nonscratching brush on the arms, hands, legs, feet, and back). These treatments are controversial and should always be discussed with the child's pediatrician before being used. If you were the parent of a child with an ASD, would you consider using such treatments? Why or why not?
Fear That Vaccines Cause Autism
One of the major medical success stories has been the development of vaccines to prevent potentially deadly diseases, including measles, mumps, rubella, diphtheria, tetanus, and polio. Indeed, vaccine programs have reduced, and in some cases even eradicated, serious infectious diseases and have saved innumerable lives. These programs have been so successful that many people today may not know what these diseases even look like or how severe they can be. Despite the success of immunization programs, however, concerns about a possible link between certain vaccines and autism have been debated for over a decade (Figure 18a.6). The debate continues, even though there is no convincing scientific evidence of a causal relationship between childhood vaccines and autism.

FIGURE 18a.6. Actress Jenny McCarthy has been outspoken in her belief that vaccines are an environmental trigger for autism.
The first hypothesis that such a link existed arose out of a 1998 study of the records of 12 children who had both autism and irritable bowel disease (a condition thought to be caused by a persistent measles-virus infection in the intestines). The parents or pediatricians of nine of the children suspected that the MMR (measles, mumps, and rubella) vaccine the children had received had caused the irritable bowel disease and contributed to the children's autism. The idea, which has not been supported by subsequent research, included the following suppositions: (1) The live virus in the MMR vaccine could cause a chronic measles infection in certain susceptible children; (2) this, in turn, could damage the bowels of these children; (3) the damaged bowels could allow certain peptides that are normally broken down by the gut to leak into the bloodstream before being completely broken down; and (4) once in the bloodstream, the peptides could damage the developing brain. Because there were too few cases in the study to establish a causal link between the MMR vaccine and autism, 10 of the 13 authors of the paper later retracted the interpretation of the data that had been presented in the paper. Other scientists criticized the study for lacking controls and using a biased sample of subjects.
Subsequent studies explored the possible link between the MMR vaccine and autism. The Institute of Medicine (IOM) of the National Academies reviewed all of these studies and issued reports in 2001 and 2004 concluding that there is no link between autism and the MMR vaccine. Studies published since 2004 have supported this conclusion. Indeed, a study published in 2008 found no evidence of an association between autism and persistent measles infection in the intestines or exposure to the MMR vaccine. In 2010, the editors of the journal that had published the 1998 study fully retracted the paper from the published record, citing its claims as false.
Another hypothesis linking autism to vaccines suggested that autism may be caused by a mercury-containing organic compound called thimerosal. Thimerosal had been used to prevent the growth of microorganisms in certain vaccines from the 1930s until the early 2000s. (Thimerosal was never used in the MMR vaccine, the other focus of contention.) Exposure to mercury is harmful to the nervous system, so it is perhaps reasonable to think that thimerosal might cause problems in the developing nervous system that might result in autism. In 2004, an IOM report concluded that it is biologically plausible for the cumulative amount of mercury in the series of recommended vaccinations for infants and toddlers to exceed the maximum federal safety standards. However, the standards pertain to methylmercury, and thimerosal contains ethylmercury, which is handled differently in the body. Further, although the IOM did not dispute that mercury-containing compounds, such as thimerosal, might damage the nervous system, there was no evidence that such damage was associated with autism. Thus, the IOM concluded in 2004 that the bulk of evidence favored rejection of a causal relationship between thimerosal-containing vaccines and autism. To date, there is no convincing scientific evidence to refute the IOM's conclusion.
Despite the lack of convincing scientific evidence that thimerosal-containing vaccines cause autism, the Public Health Service agencies, the American Academy of Pediatrics, and vaccine manufacturers agreed in 1999 that, as a precautionary measure, thimerosal should be reduced or eliminated in vaccines. Although it took some time and effort to develop thimerosal-free vaccines, it was feasible to remove mercury from vaccines and thereby reduce an individual's total exposure to mercury. It is far more difficult to control an individual's exposure to other sources of environmental mercury (forest fires, landfills, incinerators, and certain industrial processes). Currently, vaccines routinely recommended for children under the age of 6 do not contain thimerosal, or they contain only trace amounts—except for the inactivated influenza (flu) vaccine (Table 18a.3). Manufacturing capabilities of thimerosal-free flu vaccines are increasing. Vaccines for adults and for children 7 years of age and older are increasingly available in formulations without thimerosal or with only trace amounts.
Current scientific evidence does not support a causal association between either the MMR vaccine or thimerosal-containing vaccines and autism. Even so, a recent survey of parents of children with ASDs showed that 54% believe immunizations caused their child's ASD.
Looking ahead
In Chapter 18a, we discussed autism spectrum disorders, which have a strong genetic component. In Chapter 19, we take a closer look at chromosomes, which are the physical basis of heredity.
TABLE 18a.3. Thimerosal Content of Early Childhood Vaccines
Vaccine |
Age Administered (Months)* |
Current Thimerosal Status (Number of Manufacturers) |
Thimerosal History |
Hepatitis B |
Birth 1-2 6-18 |
Absent (2) |
Approval for thimerosal-free formulations in August 1999 or January 2007 |
Diphtheria, tetanus, acellular pertussis (DTaP)* |
2 4 6 15-18 |
Absent (2) or trace (1) |
Approval for thimerosal-free formulation in September 2000; approval for trace thimerosal formulation in March 2001; formulation of one manufacturer never contained thimerosal |
Haemophilus influenzae type b conjugate (Hib) |
2 4 6 12-15 |
Absent (3) |
Approval for thimerosal-free formulation in August 1999; formulations of two manufacturers never contained thimerosal |
Inactivated poliovirus |
2 4 6-18 |
Absent (1) |
Never contained thimerosal |
Pneumococcal conjugate (PCV7) |
2 4 6 12-15 |
Absent (2) |
Both formulations of manufacturer never contained thimerosal |
Rotavirus |
2 4 6 |
Absent (2) |
Formulations of two manufacturers never contained thimerosal |
Influenza, inactivated (flu shot) |
At least 6 months, one dose yearly thereafter |
Absent (3), trace (1), or present in greater than trace amounts (3) |
Approval for trace thimerosal formulation in September 2001; approval for thimerosal-free formulations in December 2004, October 2009, and November 2009 |
Influenza, live attenuated (nasal spray) |
At least 24 months, one dose yearly thereafter |
Absent (1) |
Never contained thimerosal |
Measles, mumps, rubella (MMR) |
12-15 |
Absent (1) |
Never contained thimerosal |
Varicella (chicken pox) |
12-18 |
Absent (1) |
Never contained thimerosal |
*Some of these vaccines have additional doses given at older ages; for example, DTaP, polio, MMR, and varicella are administered again at 4 to 6 years of age.