THE LIVING WORLD
Unit Six. Animal Life
27. How the Animal Body Defends Itself
In 1796, an English country doctor named Edward Jenner carried out an experiment that marks the beginning of the study of immunology. Smallpox was a common and deadly disease in those days. Jenner observed, however, that milkmaids who had caught a much milder form of “the pox” called cowpox (presumably from cows) rarely caught smallpox. Jenner set out to test the idea that cowpox conferred protection against smallpox. He infected people with mild cowpox (figure 27.14), and as he had predicted, many of them became immune to smallpox.
Figure 27.14. The birth of immunology.
This famous painting shows Edward Jenner inoculating patients with cowpox in the 1790s and thus protecting them from smallpox.
We now know that smallpox and cowpox are caused by two different but similar viruses. Jenner’s patients who were injected with the cowpox virus mounted a defense that was also effective against a later infection of the smallpox virus. Jenner’s procedure of injecting a harmless microbe to confer resistance to a dangerous one is called vaccination. Vaccination is the introduction into a person’s body of a dead or disabled pathogen or, more commonly these days, of a harmless microbe with pathogen proteins displayed on its surface. The vaccination triggers an immune response against the pathogen, without an infection ever occurring. Afterward the bloodstream of the vaccinated person contains circulating memory cells (B and T cells) directed against that specific pathogen. The vaccinated person is said to have been “immunized” against the disease.
Through genetic engineering, scientists are now routinely able to produce “piggyback,” or subunit, vaccines. These vaccines are made of harmless viruses that contain in their DNA a single gene cut out of a pathogen, a gene encoding a protein normally exposed on the pathogen’s surface. By splicing the pathogen gene into the DNA of the harmless host, that host is induced to display the protein on its surface. The harmless virus displaying the pathogen protein is like a sheep in wolf’s clothing, unable to hurt you but raising alarm as if it could. Your body responds to its presence by making an antibody directed against the pathogen protein that acts like an alarm to the immune system, should that pathogen ever visit your body.
If the activities of memory cells provide such an effective defense against future infection, why can you catch some diseases like flu more than once? The reason you don’t stay immune to flu is that the flu virus has evolved a way to evade the immune system—it changes. The genes encoding the surface proteins of the flu virus mutate very rapidly. Thus, the shapes of these surface proteins alter swiftly. Your memory cells do not recognize viruses with altered surface proteins as being the same viruses they have already successfully defeated or been vaccinated against, because the memory cells’ receptors no longer “fit” the new shape of the flu surface proteins. When the new version of flu virus invades your body, you need to mount an entirely new immune defense.
Sometimes the flu virus surface proteins possess shapes that the immune system does not readily recognize. When mutations arose in a bird flu in 1918 that allowed this flu virus to pass easily from one infected human to another, over 20 million Americans and Europeans died in 18 months (figure 27.15). Less-profound changes in flu virus surface proteins occur periodically, resulting in new strains of flu for which we are not immune. The annual flu shots are vaccines against these new strains. Researchers are able to predict the current year’s strain of the flu by examining pre-season flu reports from across the globe to prepare a vaccine against the year’s dominant strain. However, as you learned in chapter 16, entirely new flu virus strains from birds or pigs can infect humans, and genetic recombination within infected organisms can create even more new combinations of viral surface proteins.

Figure 27.15. The flu epidemic of 1918 killed over 20 million in 18 months.
With 25 million Americans alone infected during the influenza epidemic, it was hard to provide care for everyone. The Red Cross often worked around the clock.
The Search for an AIDS Vaccine
One of the most intensive efforts in the history of medicine is currently under way to develop an effective vaccine against HIV, the virus responsible for AIDS. Researchers are using the “piggyback” method shown in figure 27.16. Steps 1 through 3 show how the gene that encodes an HIV surface protein is isolated, and then it is inserted into the DNA of a harmless vaccinia virus (steps 4 and 5). The genetically engineered vaccinia virus is injected into the body 6, which triggers the body to begin producing antibodies and memory cells against the HIV surface protein antigen 7. The HIV virus has nine genes, encoding a variety of proteins. Initial efforts focused on producing a subunit vaccine containing the HIV env (envelope) gene, which encodes the protein on the outside of the virus.
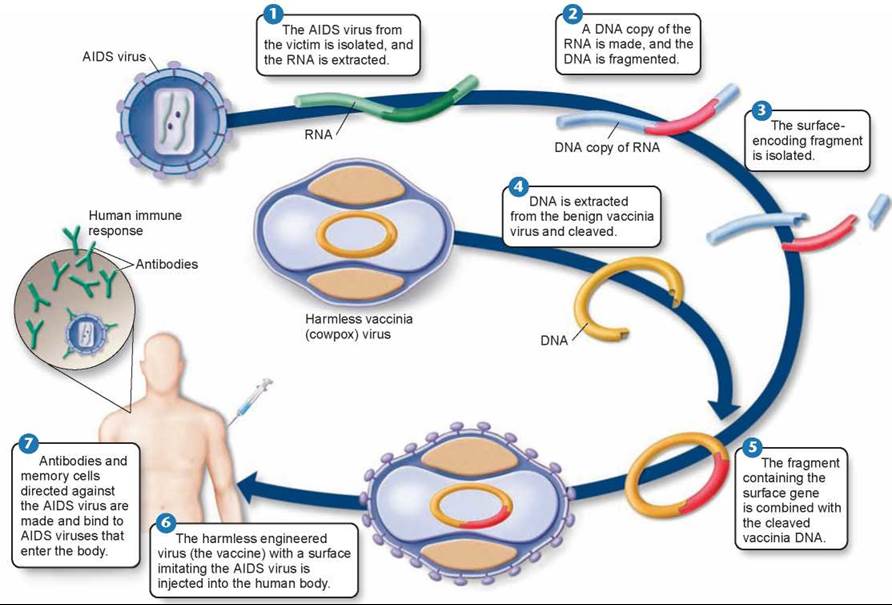
Figure 27.16. Researchers are attempting to construct an AIDS vaccine.
Unfortunately, the HIV virus mutates even more rapidly than the flu virus, and vaccines developed from one strain of the HIV virus are not effective against others. The AIDS vaccines are said to solicit narrowly neutralizing antibodies, ones that protect against only one or a few of the many hundreds of strains of HIV. This high mutation rate has been the single biggest obstacle to developing a successful AIDS vaccine.
New vaccine approaches look more promising. An intensive effort to identify broadly neutralizing antibodies that protect against many or all strains of HIV is yielding very encouraging results. One place where HIV doesn’t mutate much is where it attaches to the cell it infects. Researchers created a probe shaped exactly like that key site and used it to fish out antibodies that bind particularly well to it. By 2010, more than a half dozen broadly neutralizing antibodies had been obtained, the strongest of which neutralizes 91% of all known AIDS strains! The next step will be to do a little “reverse engineering,” using these broadly neutralizing antibodies to refine the HIV probe. Eventually, the researchers hope that the modified probe can be administered to people as a vaccine that will solicit broadly neutralizing “anti-HIV” antibodies and so protect against AIDS.
Key Learning Outcome 27.8. Vaccines introduce antigens similar or identical to those of pathogens, eliciting an immune response that defends against the pathogen too.