MCAT Biology Review
Chapter 5: The Endocrine System
5.2 Endocrine Organs and Hormones
The hypothalamus, the pituitary, the thyroid, the parathyroid glands, the adrenal glands, the pancreas, the gonads (testes and ovaries), and the pineal gland are all endocrine glands, as shown in Figure 5.3. Each of these organs is capable of synthesizing and secreting one or more hormones. Furthermore, there are collections of cells within organs, such as the kidneys, gastrointestinal glands, heart, and thymus that serve important endocrine roles. The organs in this second group are traditionally not called endocrine organs because hormone production is not their main function.
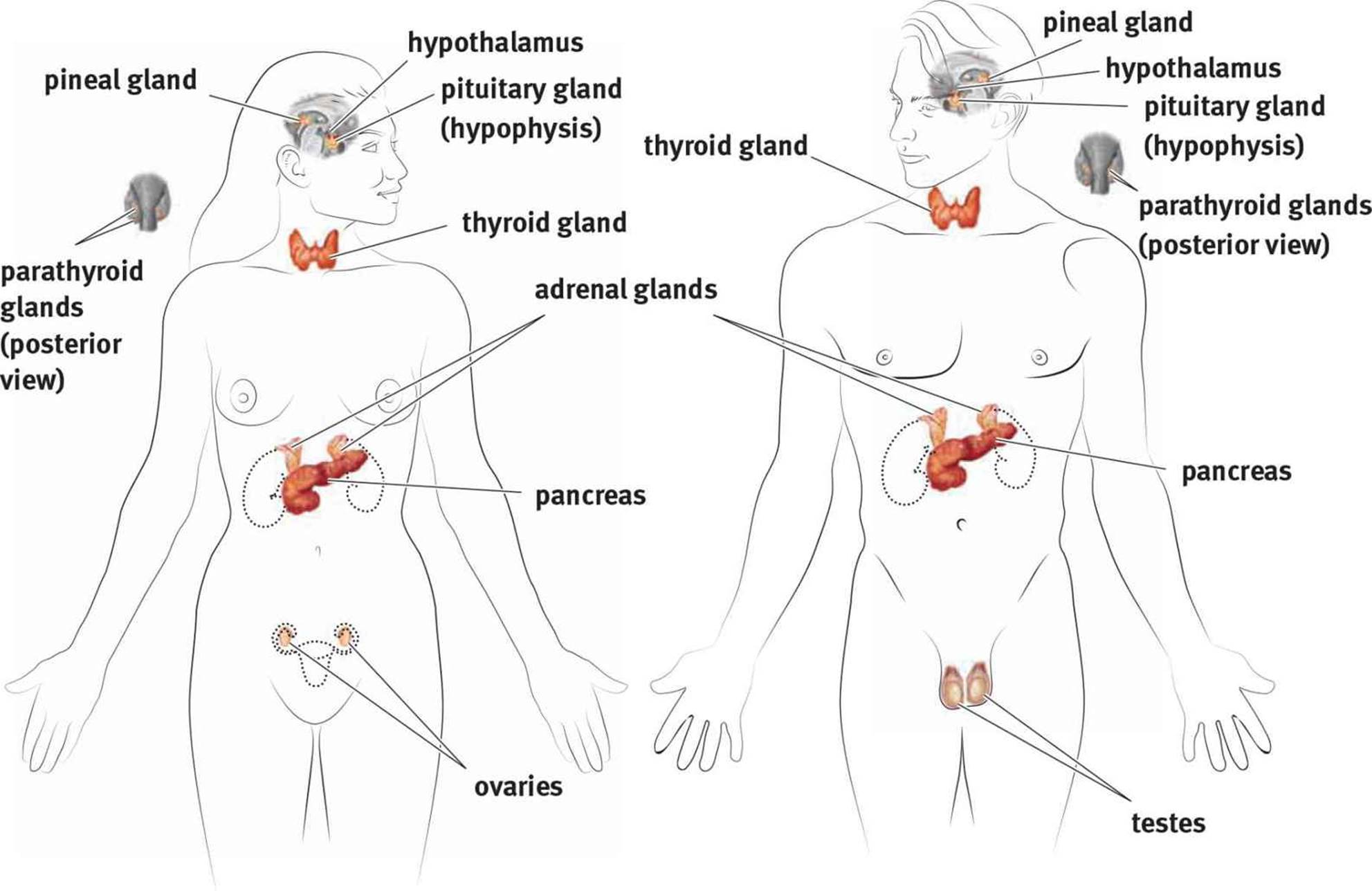 Figure 5.3. Organs of the Endocrine System Endocrine organs produce hormones that are secreted into the bloodstream to act on distant target tissues.
Figure 5.3. Organs of the Endocrine System Endocrine organs produce hormones that are secreted into the bloodstream to act on distant target tissues.
Now that we have discussed the mechanisms through which hormones act and their classification, we can discuss the individual endocrine organs and the hormones secreted by each.
HYPOTHALAMUS
Let’s begin with the hypothalamus, the bridge between the nervous and endocrine systems. By regulating the pituitary gland through tropic hormones, the hypothalamus is capable of having organism-wide effects. The hypothalamus is located in the forebrain, directly above the pituitary gland and below the thalamus (hence the name hypothalamus). Because the hypothalamus and the pituitary are close to each other, the hypothalamus controls the pituitary through paracrine release of hormones into a portal system that directly connects the two organs. The hypothalamus receives input from a wide variety of sources. For example, a part of the hypothalamus called the suprachiasmatic nucleus receives some of the light input from the retinas and helps to control sleep–wake cycles. Other parts of the hypothalamus respond to increases in blood osmolarity. Still other parts of the hypothalamus regulate appetite and satiety.
BRIDGE
The hypothalamus contains a number of nuclei in its three sections, called the lateral, ventromedial, and anterior hypothalamus. These nuclei play roles in emotional experience, aggressive behavior, sexual behavior, metabolism, temperature regulation, and water balance. The parts of the hypothalamus are discussed in Chapter 1 of MCAT Behavioral Sciences Review.
The release of hormones by the hypothalamus is regulated by negative feedback. Negative feedback occurs when a hormone (or product) later in the pathway inhibits hormones (or enzymes) earlier in the pathway. This type of feedback maintains homeostasis and prevents wasted energy by restricting production of substances that are already present in sufficient quantities. The hypothalamus and pituitary gland are inextricably linked. The pituitary gland has an anterior and posterior component, each with a unique interaction with the hypothalamus. We will discuss each in turn.
Interactions with the Anterior Pituitary
The hypothalamus secretes compounds into the hypophyseal portal system, which is a blood vessel system that directly connects the hypothalamus with the anterior pituitary, as shown in Figure 5.4. Thus, hormones released from the hypothalamus travel directly to the anterior pituitary and cannot be found in appreciable concentrations in the systemic circulation. Note that the term hypophysis is an alternative term for the pituitary. Once hormones have been released from the hypothalamus into this portal bloodstream, they travel down the pituitary stalk and bind to receptors in the anterior pituitary, stimulating the release of other hormones.
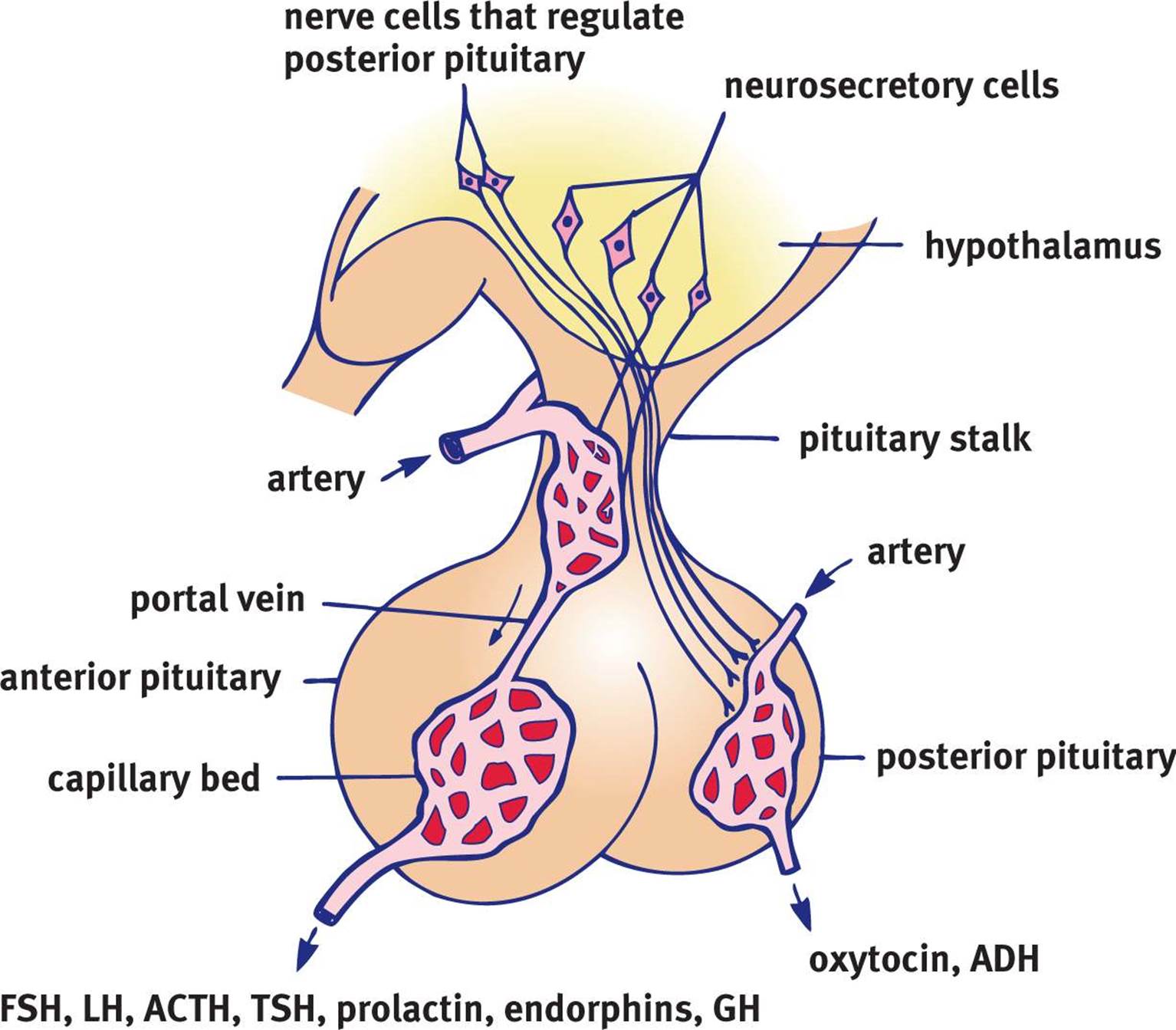 Figure 5.4. The Hypophyseal Portal System A system of blood vessels connects the hypothalamus to the pituitary.
Figure 5.4. The Hypophyseal Portal System A system of blood vessels connects the hypothalamus to the pituitary.
The hypothalamus secretes several different tropic hormones. The following indicates each hormone released by the hypothalamus and the hormone(s) released by the anterior pituitary in response:
· Gonadotropin-releasing hormone (GnRH) → follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
· Growth hormone-releasing hormone (GHRH) → growth hormone (GH)
· Thyroid-releasing hormone (TRH) → thyroid-stimulating hormone (TSH)
· Corticotropin-releasing factor (CRF) → adrenocorticotropic hormone (ACTH)
There is one exception to this pattern—prolactin-inhibiting factor (PIF), which is actually dopamine, is released by the hypothalamus and causes a decrease in prolactin secretion.
KEY CONCEPT
Whereas most of the hormones in the anterior pituitary require a factor from the hypothalamus to be released, prolactin is the exception. As long as the hypothalamus releases PIF (which is actually dopamine), no prolactin will be released. It is the absence of PIF that allows for prolactin to be released.
Each of the tropic hormones then causes the release of another hormone from an endocrine gland that has negative feedback effects. For example, release of CRF from the hypothalamus will stimulate the anterior pituitary to secrete ACTH. ACTH will then cause the adrenal cortex to increase the level of cortisol being secreted into the blood. However, cortisol is detrimental when levels become too high. To prevent excess cortisol secretion, cortisol can inhibit the hypothalamus and anterior pituitary from releasing CRF and ACTH, respectively, as shown in Figure 5.5. This makes sense because CRF and ACTH have already accomplished their desired effect: getting more cortisol into the blood. What does this mean in terms of receptors in the hypothalamus and pituitary? Cortisol receptors must be present in these organs; otherwise, they wouldn’t be able to recognize that cortisol levels had increased. Three-organ systems like these are commonly referred to as axes; for example, the hypothalamic–pituitary–adrenal (HPA) axis, the hypothalamic–pituitary–ovarian (HPO) axis, and so on.
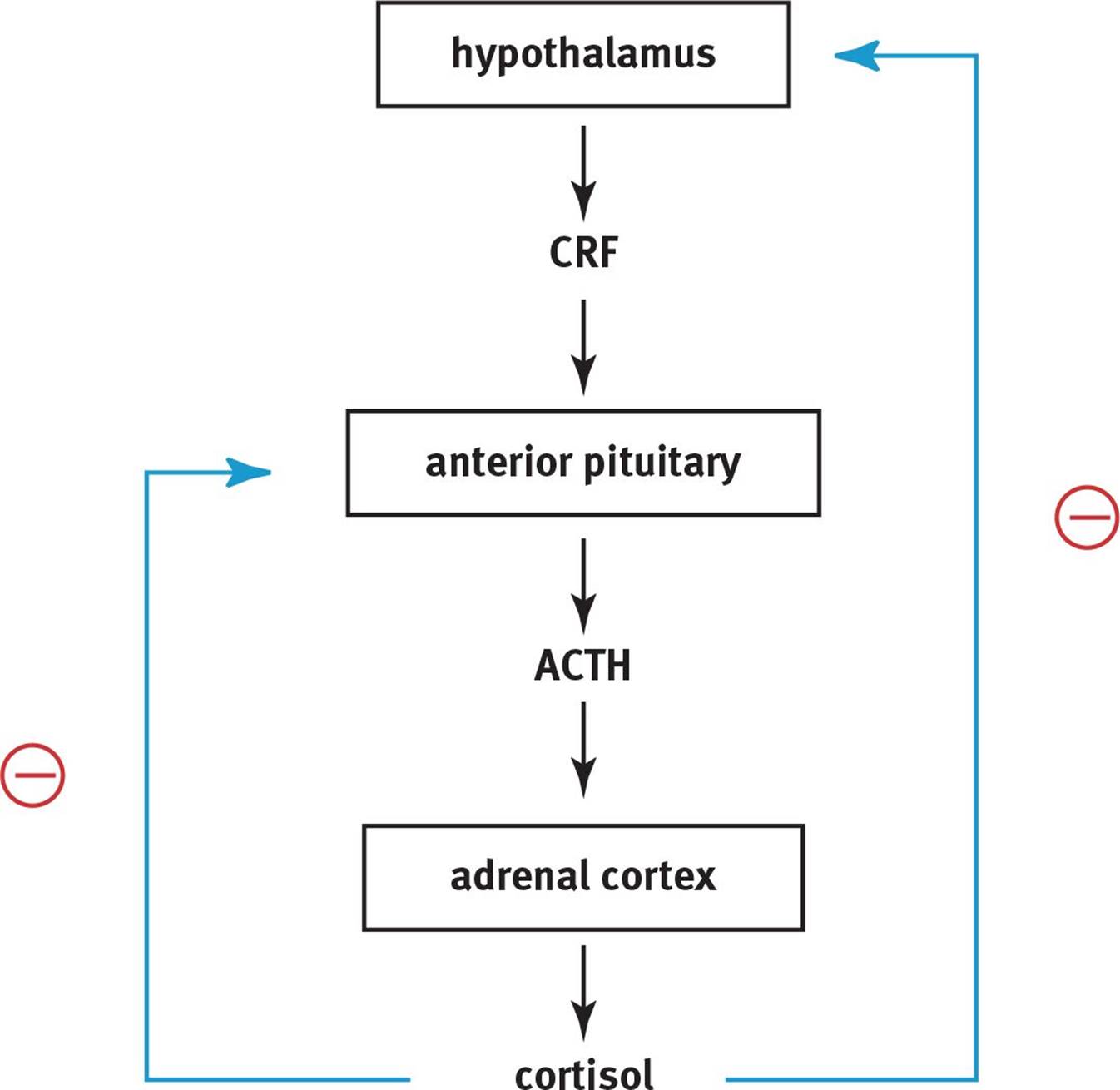 Figure 5.5. Hypothalamic Negative Feedback Mechanism
Figure 5.5. Hypothalamic Negative Feedback Mechanism
KEY CONCEPT
Although it seems as if the pituitary has all the power in the endocrine system, the anterior pituitary is controlled by the hypothalamus, which is located directly above it.
Interactions with the Posterior Pituitary
The posterior pituitary does not receive tropic hormones through the hypophyseal portal system. Rather, neurons in the hypothalamus send their axons down the pituitary stalk directly into the posterior pituitary, which can then release oxytocin and antidiuretic hormone. Oxytocin is a hormone that stimulates uterine contractions during labor, as well as milk letdown during lactation. There is evidence that oxytocin is also involved in bonding behavior. Antidiuretic hormone (ADH, also called vasopressin) increases reabsorption of water in the collecting ducts of the kidneys. ADH is secreted in response to increased plasma osmolarity, or increased concentration of solutes within the blood.
REAL WORLD
A tumor of the pituitary gland may result in compression of the portal system that connects the pituitary to the hypothalamus. This will block the ability of PIF to reach the pituitary and exert its effect. Thus, more prolactin will be released. This may result in lactation (galactorrhea), even in males. Thus, milk production in a male or nonpregnant female should urge a physician to check for a pituitary tumor.
ANTERIOR PITUITARY
As described earlier, the pituitary gland is divided into anterior and posterior sections. Because this distinction has already been covered, our discussion of the pituitary gland here will focus on the hormones released by each section.
MNEMONIC
Products of the anterior pituitary:
FLAT PEG
· Follicle-stimulating hormone (FSH)
· Luteinizing hormone (LH)
· Adrenocorticotropic hormone (ACTH)
· Thyroid-stimulating hormone (TSH)
· Prolactin
· Endorphins
· Growth hormone (GH)
Additionally, the four hormones in FLAT are all tropic hormones, while the three hormones in PEG are all direct hormones.
The anterior pituitary synthesizes and secretes seven different products. Four of these are tropic hormones, while the other three are direct hormones.
Tropic Hormones
We are going to mention the tropic hormones only briefly here. These hormones work by causing the release of another hormone at the organ level. Thus, we will discuss the tropic hormones in tandem with the endocrine organ on which they act. The release of both follicle-stimulating hormone (FSH) and luteinizing hormone (LH) is stimulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus. These two hormones act on the gonads (testes and ovaries). The release of adrenocorticotropic hormone (ACTH) is stimulated by corticotropin-releasing factor (CRF) from the hypothalamus; ACTH acts on the adrenal cortex. The release of thyroid-stimulating hormone (TSH) is stimulated by thyroid-releasing hormone (TRH) from the hypothalamus; TSH acts on the thyroid.
Direct Hormones
Prolactin is more important in females than in males; it stimulates milk production in the mammary glands. Milk production in the male is always pathologic. During pregnancy, estrogen and progesterone levels are high. In addition, prolactin, a hormone that increases milk production, is also secreted by the anterior pituitary. Prolactin is an unusual hormone in that the release of dopamine from the hypothalamus decreases its secretion. The high levels of estrogen and progesterone allow for the development of milk ducts in preparation for lactation, but it is not until shortly after the expulsion of the placenta, when estrogen, progesterone, and dopamine levels drop, that the block on milk production is removed and lactation actually begins.
Milk ejection occurs when the newborn infant latches on to the breast. Nipple stimulation causes activation of the hypothalamus, resulting in two different reactions. First, oxytocin is released from the posterior pituitary, resulting in contraction of the smooth muscle of the breast and ejection of milk through the nipple. Second, the hypothalamus stops releasing dopamine onto the anterior pituitary, which—as mentioned above—allows prolactin release, causing production of milk and regulation of the milk supply.
Endorphins decrease the perception of pain. For example, after completing a marathon, many people will say they are on an endorphin “high” or “rush.” Endorphins mask the pain from just having run 26.2 miles and can even induce a sense of euphoria. Many pharmaceutical agents, such as morphine, mimic the effect of these naturally occuring painkillers.
Growth hormone (GH) is named for exactly what it does: it promotes the growth of bone and muscle. This sort of growth is energetically expensive and requires large quantities of glucose. Growth hormone prevents glucose uptake in certain tissues (those that are not growing) and stimulates the breakdown of fatty acids. This increases the availability of glucose overall, allowing the muscle and bone to use it. GH release is stimulated by growth hormone-releasing hormone (GHRH) from the hypothalamus.
Bone growth originates in special regions of the bone known as epiphyseal plates, which seal shut during puberty. An excess of GH released in childhood (before this closure) can cause gigantism, and a deficit results in dwarfism. In adults, the situation is slightly different. Because the long bones are sealed, GH still has an effect, but it is primarily in the smaller bones. The resulting medical condition is known as acromegaly. The bones most commonly affected are those in the hands, feet, and head. Patients with acromegaly tend to present to their doctors because they have had to buy larger shoes, cannot wear their rings, and can no longer fit into their hats.
POSTERIOR PITUITARY
The posterior pituitary contains the nerve terminals of neurons with cell bodies in the hypothalamus. As mentioned earlier, the posterior pituitary receives and stores two hormones produced by the hypothalamus: ADH and oxytocin.
ADH is secreted in response to low blood volume (as sensed by baroreceptors) or increased blood osmolarity (as sensed by osmoreceptors), as shown in Figure 5.6. Its action is at the level of the collecting duct, where it increases the permeability of the duct to water. The net effect is a greater reabsorption of water from the filtrate in the nephron. This results in greater retention of water, which results in increased blood volume and higher blood pressure.
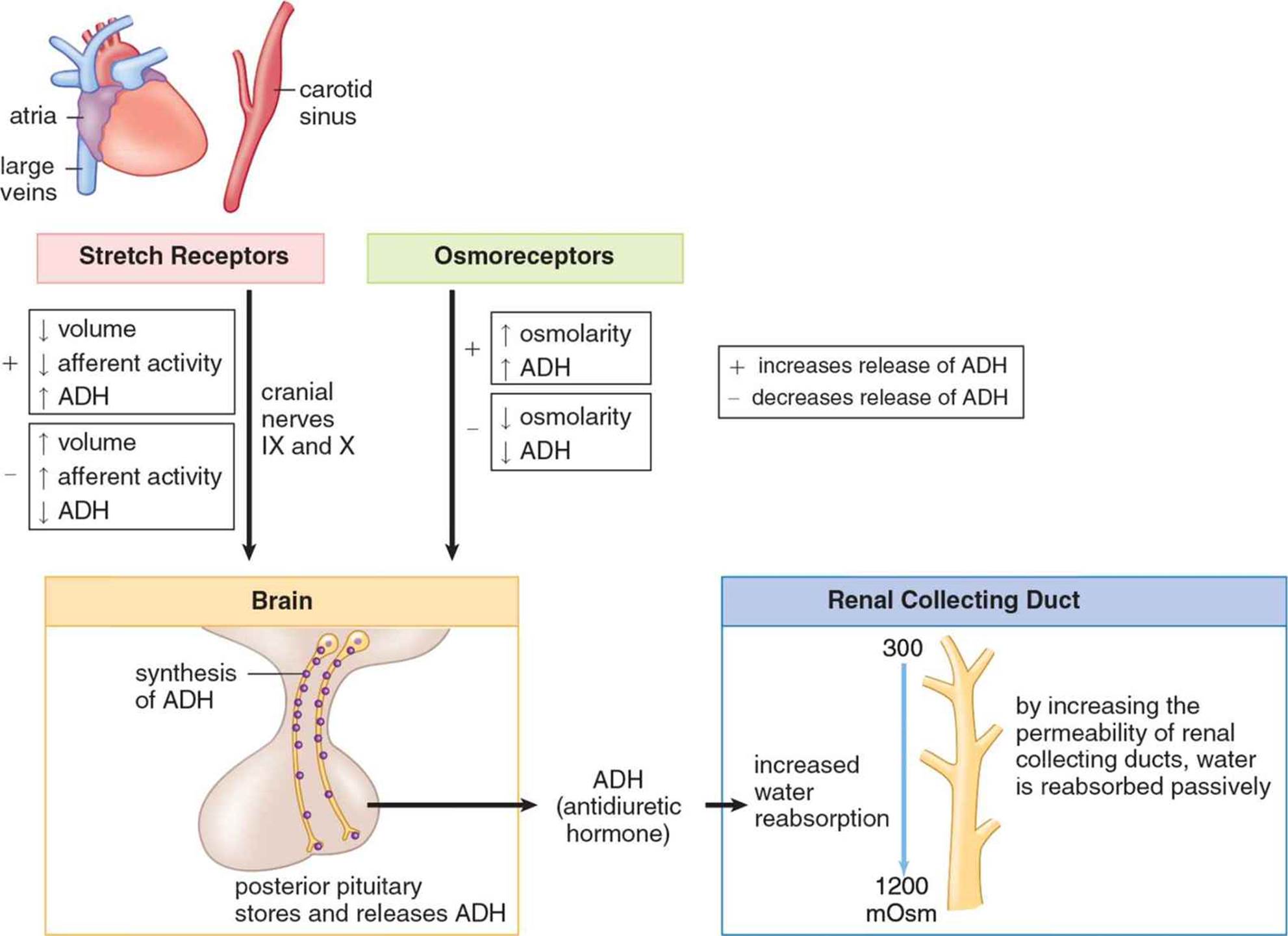 Figure 5.6. Antidiuretic Hormone (ADH)
Figure 5.6. Antidiuretic Hormone (ADH)
Oxytocin is secreted during childbirth and allows for coordinated contraction of uterine smooth muscle. Its secretion may also be stimulated by suckling, as it promotes milk ejection through contraction of smooth muscle in the breast. Finally, oxytocin may be involved in bonding behavior. Oxytocin is unusual in that it has a positive feedback loop: the release of oxytocin promotes uterine contraction, which promotes more oxytocin release, which promotes stronger uterine contractions, and so on. Positive feedback loops can usually be identified by this theme of a “spiraling forward” process and usually have a definitive endpoint—in this case, delivery.
KEY CONCEPT
The two hormones released from the posterior pituitary are actually synthesized in the hypothalamus, and simply released from the posterior pituitary gland. The posterior pituitary does not synthesize any hormones itself.
THYROID
The thyroid is controlled by thyroid-stimulating hormone from the anterior pituitary. The thyroid is on the front surface of the trachea; it can be palpated (felt) as an organ near the base of the neck that moves up and down with swallowing. The thyroid has two major functions: setting basal metabolic rate and calcium homeostasis. It mediates the first effect by releasing triiodothyronine (T3) and thyroxine (T4), whereas calcium levels are controlled by calcitonin.
Triiodothyronine and Thyroxine
Triiodothyronine (T3) and thyroxine (T4) are both produced by the iodination of the amino acid tyrosine in the follicular cells of the thyroid. The numbers 3 and 4 refer to the number of iodine atoms attached to the tyrosine. Thyroid hormones are capable of resetting the basal metabolic rate of the body by making energy production more or less efficient, as well as altering the utilization of glucose and fatty acids. Increased amounts of T3 and T4 will lead to increased cellular respiration. This leads to a greater amount of protein and fatty acid turnover by speeding up both synthesis and degradation of these compounds. High plasma levels of thyroid hormones will lead to decreased TSH and TRH synthesis; negative feedback prevents excessive secretion of T3 and T4, as shown in Figure 5.7.
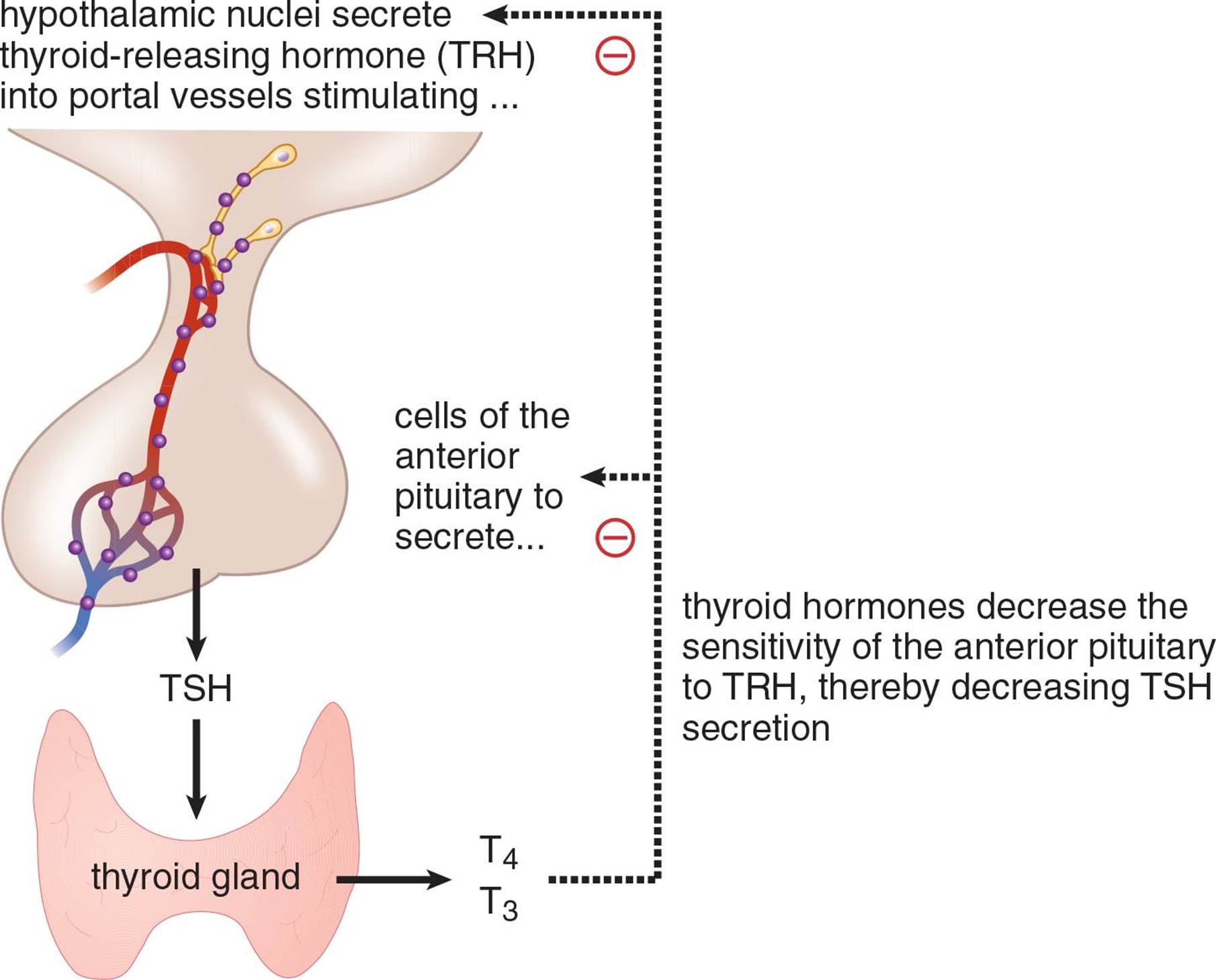 Figure 5.7. Thyroid Hormone Negative Feedback Mechanism
Figure 5.7. Thyroid Hormone Negative Feedback Mechanism
A deficiency of iodine or inflammation of the thyroid may result in hypothyroidism, in which thyroid hormones are secreted in insufficient amounts or not at all. The condition is characterized by lethargy, decreased body temperature, slowed respiratory and heart rate, cold intolerance, and weight gain. Thyroid hormones are required for appropriate neurological and physical development in children. Most children are tested at birth for appropriate levels because a deficiency will result in mental retardation and developmental delay (cretinism).
An excess of thyroid hormone, which may result from a tumor or thyroid overstimulation, is called hyperthyroidism. We can predict the clinical course of this syndrome by considering the opposite of each of the effects seen in hypothyroidism: heightened activity level, increased body temperature, increased respiratory and heart rate, heat intolerance, and weight loss.
Calcitonin
If we were to examine thyroid tissue under a light microscope, we would see two distinct cell populations within the gland. Follicular cells produce thyroid hormones and C-cells (also called parafollicular cells) produce calcitonin. Calcitonin acts to decrease plasma calcium levels in three ways: increased calcium excretion from the kidneys, decreased calcium absorption from the gut, and increased storage of calcium in the bone. High levels of calcium in the blood stimulate secretion of calcitonin from the C-cells.
MNEMONIC
Calcitonin tones down calcium levels in the blood.
PARATHYROID GLANDS
The parathyroids are four small pea-sized structures that sit on the posterior surface of the thyroid. The hormone produced by the parathyroid glands is aptly named parathyroid hormone (PTH). PTH serves as an antagonistic hormone to calcitonin, raising blood calcium levels; specifically, it decreases excretion of calcium by the kidneys, increases absorption of calcium in the gut (via vitamin D), and increases bone resorption, thereby freeing up calcium, as shown in Figure 5.8. Like the hormones we have already seen, PTH is also subject to feedback inhibition. As levels of plasma calcium rise, PTH secretion is decreased. Parathyroid hormone also affects phosphorus homeostasis by resorbing phosphate from bone and reducing reabsorption of phosphate in the kidney (thus promoting its excretion in the urine).
KEY CONCEPT
Calcium is an exceptionally important ion. The critically important functions of calcium include:
· Bone structure and strength
· Regulation of muscle contraction
· Clotting of blood (calcium is a cofactor)
In addition, calcium also plays a role in cell movement, exocytosis, and neurotransmitter release.
PTH also activates vitamin D, which is required for the absorption of calcium and phosphate in the gut. The overall effect of parathyroid hormone, therefore, is a significant increase in blood calcium levels with little effect on phosphate (the absorption of phosphate in the gut and its excretion in the kidney somewhat cancel each other).
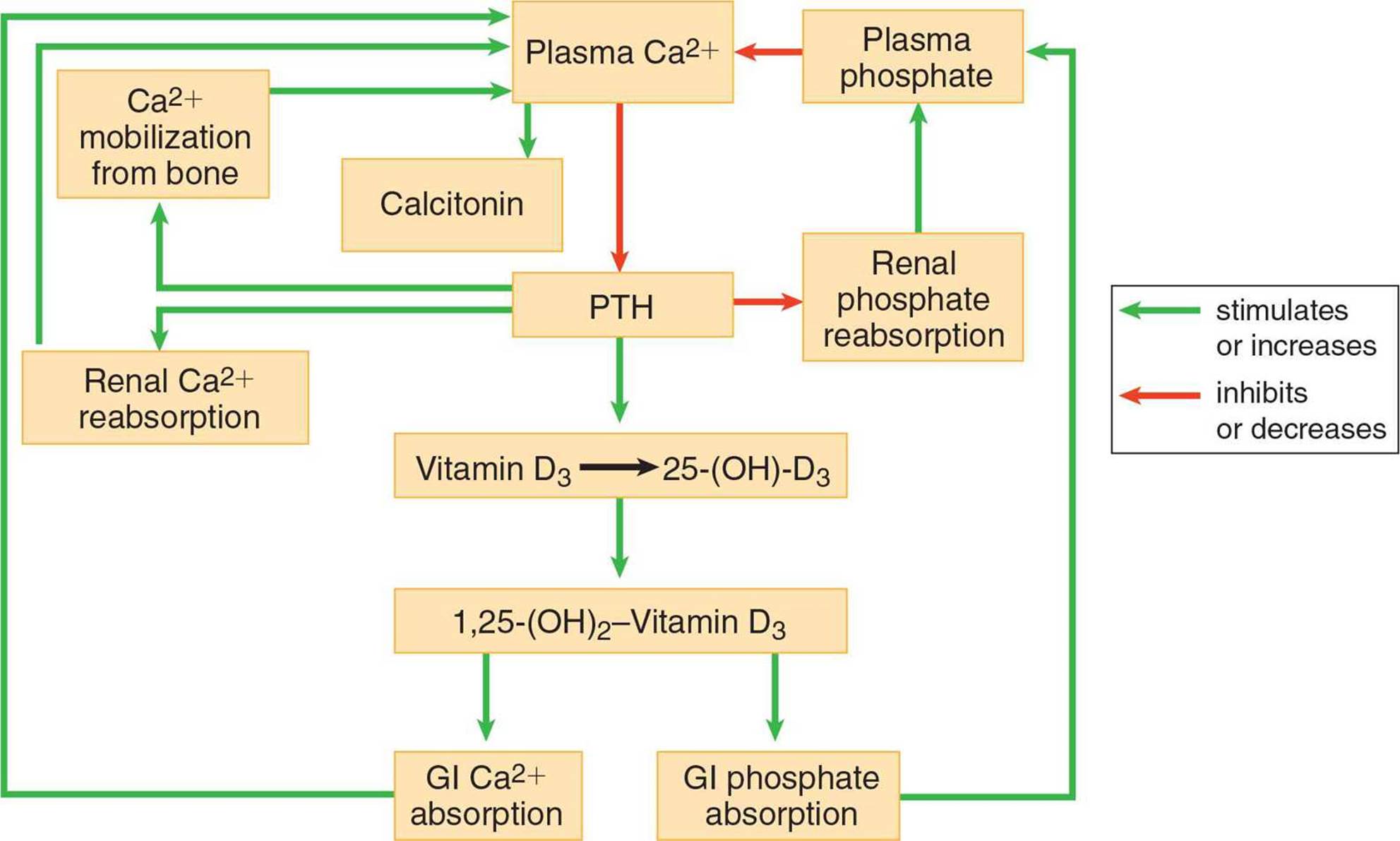 Figure 5.8. Calcium and Phosphorus Homeostasis
Figure 5.8. Calcium and Phosphorus Homeostasis
KEY CONCEPT
Just like glucagon and insulin, PTH and calcitonin are antagonistic to each other. We should think of these hormones as a pair with the primary function of regulating calcium levels in the blood. PTH increases calcium levels, whereas calcitonin decreases calcium levels.
ADRENAL CORTEX
The adrenal glands are located on top of the kidneys. Adrenal actually translates to near or next to the kidney. Each adrenal gland consists of a cortex and a medulla. This distinction is more than anatomical. Each part of the gland is responsible for the secretion of different hormones. Theadrenal cortex secretes corticosteroids. These are steroid hormones that can be divided into three functional classes: glucocorticoids, mineralocorticoids, and cortical sex hormones.
Glucocorticoids
Glucocorticoids are steroid hormones that regulate glucose levels. In addition, these hormones also affect protein metabolism. The two glucocorticoids most likely to be tested on the MCAT are cortisol and cortisone. These hormones raise blood glucose by increasing gluconeogenesis and decreasing protein synthesis. Cortisol and cortisone can also decrease inflammation and immunologic responses. Cortisol is also known as a stress hormone because it is released in times of physical or emotional stress. This increases blood sugar and provides a ready source of fuel in case the body must react quickly to a dangerous stimulus.
REAL WORLD
Many people who suffer from joint pain may be treated with glucocorticoid injections into the joint space. These injections decrease inflammation. In addition, glucocorticoids are used to treat systemic inflammation such as that which occurs due to allergies or autoimmune disease.
Glucocorticoid release is under the control of adrenocorticotropic hormone (ACTH) as described earlier. Corticotropin-releasing factor (CRF) from the hypothalamus promotes release of adrenocorticotropic hormone (ACTH) from the anterior pituitary, which promotes release of glucocorticoids from the adrenal cortex.
Mineralocorticoids
Mineralocorticoids are used in salt and water homeostasis; their most profound effects are on the kidneys. The most noteworthy mineralocorticoid is aldosterone, which increases sodium reabsorption in the distal convoluted tubule and collecting duct of the nephron. Water follows the sodium cations into the bloodstream, increasing blood volume and pressure. Note that, while the blood pressure increases, the plasma osmolarity remains unchanged—unlike with ADH. Aldosterone also decreases the reabsorption of potassium and hydrogen ions in these same segments of the nephron, promoting their excretion in the urine.
REAL WORLD
In addition to stimulating the secretion of aldosterone, which increases blood volume and hence blood pressure, angiotensin II also increases blood pressure directly through a powerful vasoconstrictive effect and by increasing heart rate. Angiotensin-converting enzyme (ACE) inhibitors block the conversion of angiotensin I to angiotensin II, inhibiting vasoconstriction. Therefore, ACE inhibitors are frequently prescribed for the treatment of high blood pressure and congestive heart failure. In the latter case, vasodilation helps reduce the resistance against which the failing heart must pump. Most ACE inhibitors’ names end with –pril (lisinopril, enalapril, ramipril).
Unlike the glucocorticoids, aldosterone is primarily under the control of the renin – angiotensin –aldosterone system, as shown in Figure 5.9. Decreased blood pressure causes the juxtaglomerular cells of the kidney to secrete renin, which cleaves an inactive plasma protein,angiotensinogen, to its active form, angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin-converting enzyme (ACE) in the lungs. Angiotensin II stimulates the adrenal cortex to secrete aldosterone. Once blood pressure is restored, there is a decreased drive to stimulate renin release, thus serving as the negative feedback mechanism for this system.
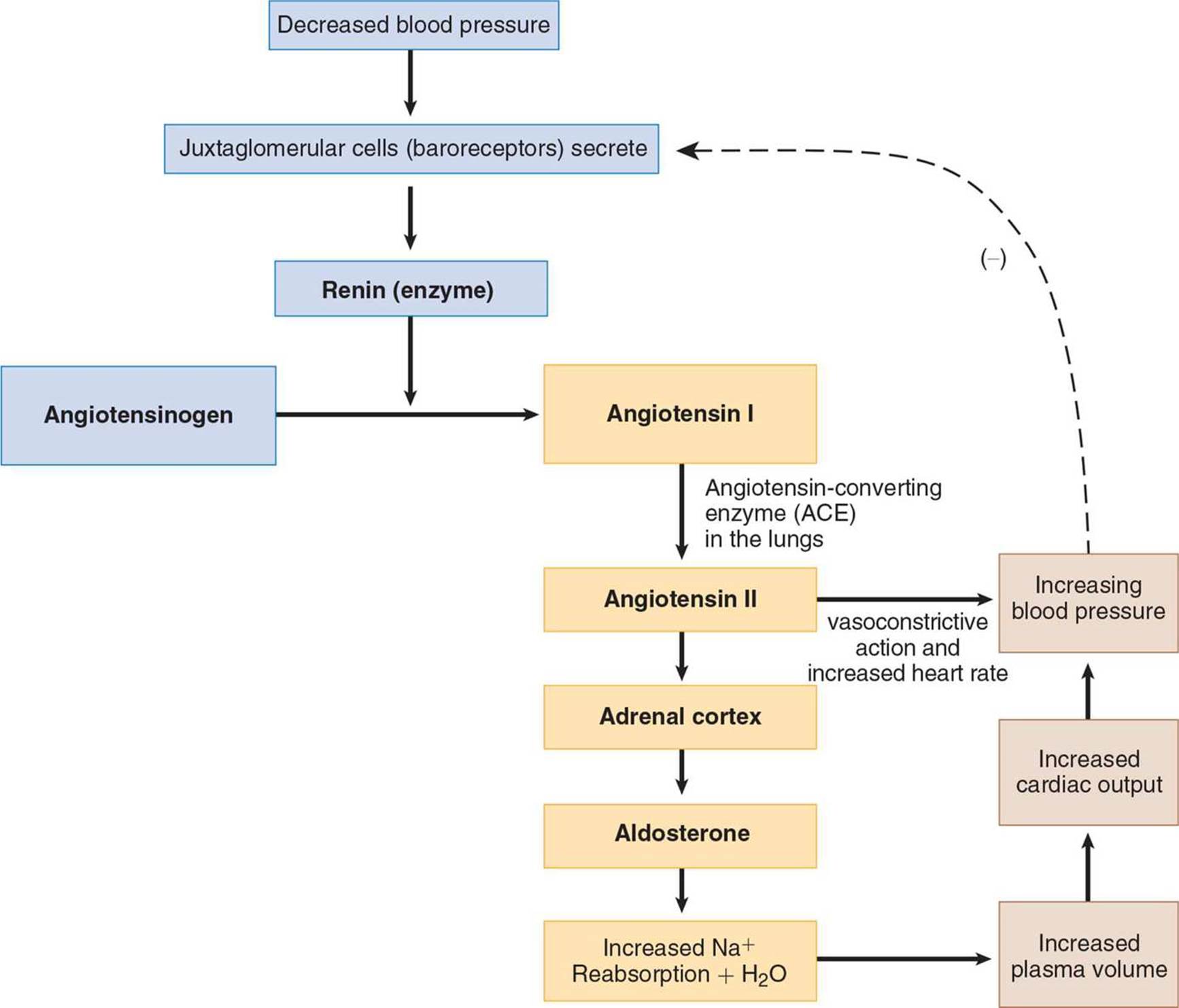 Figure 5.9. The Renin– Angiotensin– Aldosterone System
Figure 5.9. The Renin– Angiotensin– Aldosterone System
Cortical Sex Hormones
The adrenal glands also make cortical sex hormones (androgens and estrogens). Because males already secrete large quantities of androgens in the testes, adrenal testosterone plays a small role in male physiology. However, females are much more sensitive to disorders of cortical sex hormone production. For example, certain enzyme deficiencies in the synthetic pathways of other adrenal cortex hormones result in excess androgen production in the adrenal cortex. Such a deficiency would result in no obvious phenotypic effects in a male fetus; however, a genotypic female may be born with ambiguous or masculinized genitalia due to the presence of excess cortical sex hormones. Males can be affected by similar disorders if they lead to excessive production of estrogens.
MNEMONIC
Functions of the corticosteroids:
The 3 S’s
· Salt (mineralocorticoids)
· Sugar (glucocorticoids)
· Sex (cortical sex hormones)
ADRENAL MEDULLA
Nestled inside the adrenal cortex is the adrenal medulla. A derivative of the nervous system, this organ is responsible for the production of the sympathetic hormones epinephrine and norepinephrine. The specialized nerve cells in the medulla are capable of secreting these compounds directly into the circulatory system. Both epinephrine and norepinephrine are amino acid-derivative hormones that belong to a larger class of molecules known as catecholamines.
Much like the sympathetic component of the autonomic nervous system, the hormones released from the adrenal medulla affect a wide variety of systems in the body, and all of their effects are centered on the fight-or-flight response. Epinephrine can increase the breakdown of glycogen to glucose (glycogenolysis) in both liver and muscle, as well as increase the basal metabolic rate. Both hormones will increase heart rate, dilate the bronchi, and alter blood flow to supply the systems that would be used in a sympathetic response. That is, there is vasodilation of blood vessels leading to the skeletal muscle, heart, lungs, and brain, increasing bloodflow to these organs. Concurrently, vasoconstriction decreases blood flow to the gut, kidneys, and skin. Note that the stress response involves both cortisol and epinephrine. Classically, cortisol is thought of as being important for long-term (slow) stress responses, while catecholamines are thought of as being important for short-term (fast) stress responses. Note, however, that cortisol actually increases the synthesis of catecholamines as well, resulting in an increase in catecholamine release.
PANCREAS
The pancreas has both exocrine and endocrine functions. Exocrine tissues secrete substances directly into ducts; the pancreas produces a number of digestive enzymes, as discussed in Chapter 9 of MCAT Biology Review. From an endocrine standpoint, small groups of hormone-producing cells are grouped together into islets of Langerhans throughout the pancreas, as shown in Figure 5.10. Islets contain three distinct types of cells: alpha (α), beta (β), and delta (δ) cells. Each cell type secretes a different hormone: α-cells secrete glucagon, β-cells secrete insulin, and δ-cells secrete somatostatin.
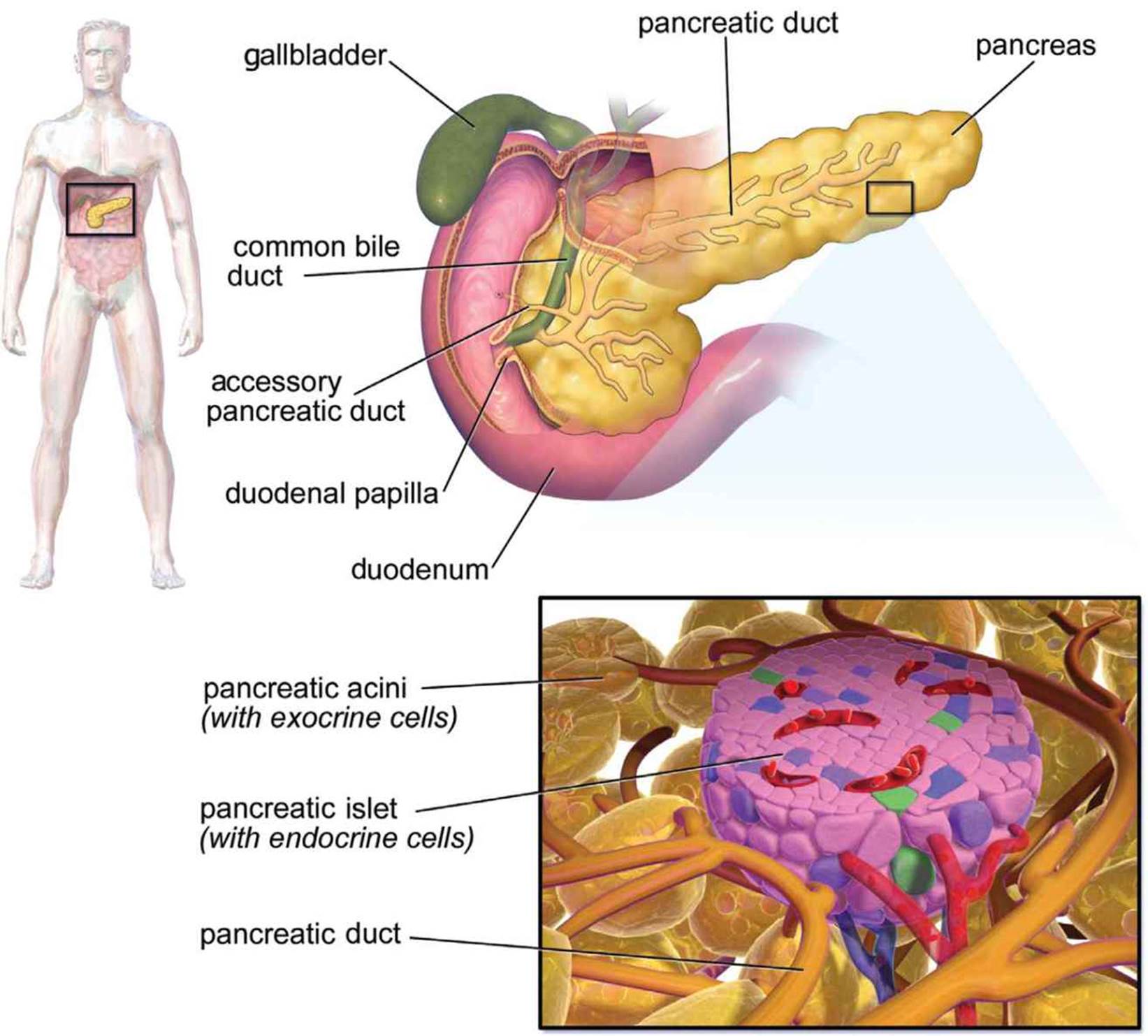 Figure 5.10. Anatomy of the Pancreas Islets of Langerhans are scattered throughout the pancreas and serve the endocrine function of the organ.
Figure 5.10. Anatomy of the Pancreas Islets of Langerhans are scattered throughout the pancreas and serve the endocrine function of the organ.
Glucagon
Glucagon is secreted during times of fasting. When glucose levels run low, the secretion of glucagon stimulates degradation of protein and fat, conversion of glycogen to glucose, and production of new glucose via gluconeogenesis. In addition to low blood glucose concentrations, certain gastrointestinal hormones (such as cholecystokinin and gastrin) increase glucagon release from α-cells. When blood glucose concentrations are high, glucagon release is inhibited.
MNEMONIC
Glucagon levels are high when glucose is gone.
Insulin
Insulin is antagonistic to glucagon and is therefore secreted when blood glucose levels are high, as shown in Figure 5.11. Insulin induces muscle and liver cells to take up glucose and store it as glycogen for later use. In addition, because it is active when glucose levels are high, insulin stimulates anabolic processes such as fat and protein synthesis.
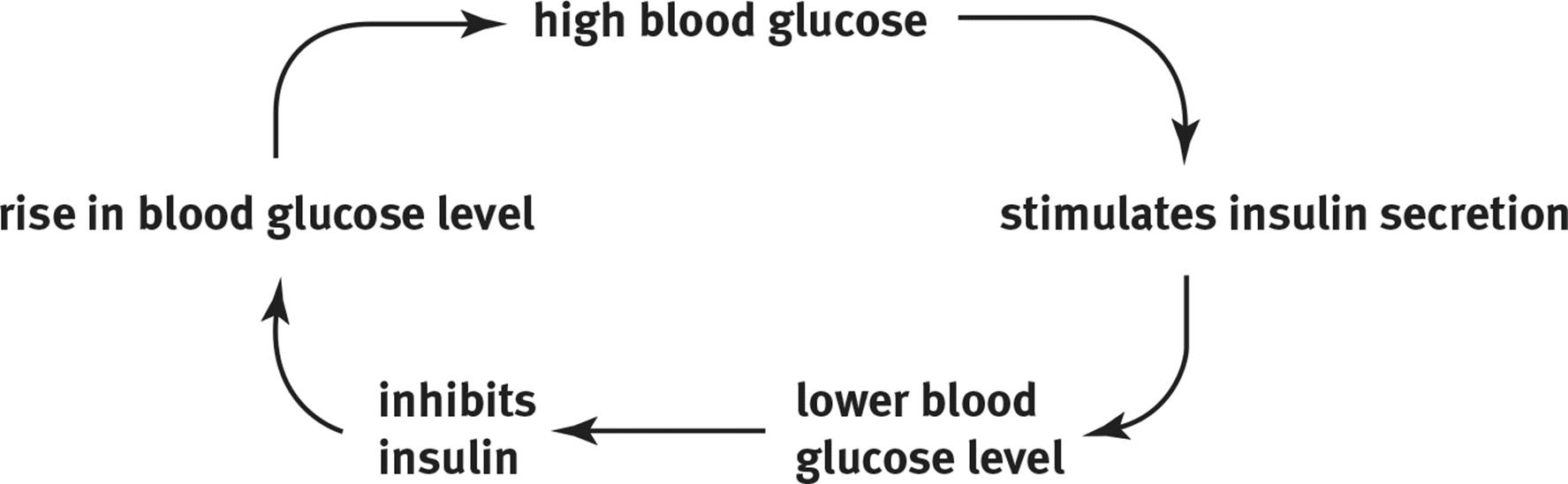 Figure 5.11. Insulin Has a Direct Relationship with Blood Glucose Concentration When blood glucose levels are high, insulin levels rise, causing cells to take up glucose from the blood; when blood glucose levels are low, insulin levels remain low as well.
Figure 5.11. Insulin Has a Direct Relationship with Blood Glucose Concentration When blood glucose levels are high, insulin levels rise, causing cells to take up glucose from the blood; when blood glucose levels are low, insulin levels remain low as well.
In excess, insulin will cause hypoglycemia, which is characterized by low blood glucose concentration. Underproduction, insufficient secretion, or insensitivity to insulin all can result in diabetes mellitus, which is clinically characterized by hyperglycemia (excess glucose in the blood). In the kidneys, excessive glucose in the filtrate will overwhelm the nephron’s ability to reabsorb glucose, resulting in its presence in the urine. Because it is an osmotically active particle and does not readily cross the cell membrane, the presence of glucose in the filtrate leads to excess excretion of water and an increase—that is sometimes quite dramatic—of the urine volume. Diabetics often report polyuria (increased frequency of urination) and polydipsia (increased thirst). There are two types of diabetes mellitus. Type I (insulin-dependent) diabetes mellitus is caused by autoimmune destruction of the β-cells of the pancreas; these individuals produce little to no insulin because the majority of β-cells have been destroyed. Type I diabetics require regular injections of insulin to prevent hyperglycemia and to permit entry of glucose into cells. Type II (non-insulin-dependent) diabetes mellitus is the result of receptor-level resistance to the effects of insulin. Type II diabetes mellitus is partially inherited and partially due to environmental factors, such as high-carbohydrate diets and obesity. Certain pharmaceutical agents can be taken orally to help the body more effectively use the insulin it produces. These individuals require insulin only when their bodies can no longer control glucose levels, even when aided by these medications.
KEY CONCEPT
Insulin decreases plasma glucose. Glucagon increases plasma glucose. Growth hormone, glucocorticoids, and epinephrine are also capable of increasing plasma glucose. These hormones that raise blood glucose levels are commonly called counterregulatory hormones.
Somatostatin
Somatostatin is an inhibitor of both insulin and glucagon secretion. High blood glucose and amino acid concentrations stimulate its secretion. Somatostatin is also produced by the hypothalamus, where it functions to decrease growth hormone secretion in addition to its effects on insulin and glucagon.
GONADS
Because reproductive endocrinology is discussed in detail in Chapter 2 of MCAT Biology Review, we offer only a brief overview in this chapter. The testes secrete testosterone in response to stimulation by gonadotropins (LH and FSH). Testosterone causes sexual differentiation of the male during gestation and also promotes the development and maintenance of secondary sex characteristics in males, such as axillary and pubic hair, deepening of the voice, and muscle growth.
The ovaries secrete estrogen and progesterone in response to gonadotropins. Estrogen is involved in development of the female reproductive system during gestation and also promotes the development and maintenance of secondary sex characteristics in females, such as axillary and pubic hair, breast growth, and body fat redistribution. These two steroid hormones also govern the menstrual cycle as well as pregnancy.
PINEAL GLAND
The pineal gland is located deep within the brain, where it secretes the hormone melatonin. The precise mechanism of this hormone is unclear, although it has been demonstrated to be involved in circadian rhythms. Blood levels of melatonin are at least partially responsible for the sensation of sleepiness. The pineal gland receives projections directly from the retina, but is not involved in vision; it is hypothesized that the pineal gland responds to decreases in light intensity by releasing melatonin.
REAL WORLD
Melatonin has enjoyed somewhat of a wonder drug status over the past decade as it is touted as a remedy for everything from jet lag to aging. Certainly, one effect of melatonin is to cause overwhelming drowsiness, supporting its utility for “resetting” one’s daily rhythm. Melatonin is available over the counter in health food stores, but the long-term effects of melatonin therapy are currently unknown.
OTHER ORGANS
In addition to the organs listed above, specific cells and tissues in other organs are capable of endocrine signaling. In the gastrointestinal tract, endocrine tissue can be found in both the stomach and intestine. Many gastrointestinal peptides have been identified; important ones include secretin, gastrin, and cholecystokinin. The specific functions of these hormones are discussed in Chapter 9 of MCAT Biology Review, but as we might expect for the digestive system, the stimulus for release of most of these peptides is the presence of specific nutrients.
The kidneys play a role in water balance. As mentioned earlier, the renin–angiotensin–aldosterone system increases sodium and water reabsorption. The kidneys also produce erythropoietin, which stimulates bone marrow to increase production of erythrocytes (red blood cells). It is secreted in response to low oxygen levels in the blood.
The heart releases atrial natriuretic peptide (ANP) to help regulate salt and water balance. When cells in the atria are stretched from excess blood volume, they release ANP. This hormone promotes excretion of sodium and therefore increases urine volume. This effect is functionally antagonistic to aldosterone because it lowers blood volume and pressure.
The thymus, located directly behind the sternum, releases thymosin, which is important for proper T-cell development and differentiation. The thymus atrophies by adulthood, and thymosin levels drop accordingly. The function of T-cells is discussed in Chapter 8 of MCAT Biology Review.
A full list of hormones and their actions can be found in Table 5.1 below.
|
Hormone |
Source |
Type |
Action |
|
Follicle-stimulating hormone (FSH) |
Anterior pituitary |
Peptide |
Stimulates follicle maturation in females; spermatogenesis in males |
|
Luteinizing hormone (LH) |
Peptide |
Stimulates ovulation in females; testosterone synthesis in males |
|
|
Adrenocorticotropic hormone (ACTH) |
Peptide |
Stimulates the adrenal cortex to synthesize and secrete glucocorticoids |
|
|
Thyroid-stimulating hormone (TSH) |
Peptide |
Stimulates the thyroid to produce thyroid hormones |
|
|
Prolactin |
Peptide |
Stimulates milk production and secretion |
|
|
Endorphins |
Peptide |
Decreases sensation of pain; can promote euphoria |
|
|
Growth hormone (GH) |
Peptide |
Stimulates bone and muscle growth; raises blood glucose levels |
|
|
Antidiuretic hormone (ADH; vasopressin) |
Hypothalamus (released by posterior pituitary) |
Peptide |
Stimulates water reabsorption in kidneys by increasing permeability of collecting duct |
|
Oxytocin |
Peptide |
Stimulates uterine contractions during labor and milk secretion during lactation; may promote bonding behavior |
|
|
Triiodothyronine (T3) and thyroxine (T4) |
Thyroid (follicular cells) |
Amino acidderivative |
Stimulate metabolic activity |
|
Calcitonin |
Thyroid (parafollicular or C cells) |
Peptide |
Decreases blood calcium concentrations |
|
Parathyroid hormone (PTH) |
Parathyroids |
Peptide |
Increases blood calcium concentrations |
|
Glucocorticoids (cortisol and cortisone) |
Adrenal cortex |
Steroid |
Increase blood glucose concentrations; decrease protein synthesis; antiinflammatory |
|
Mineralocorticoids (aldosterone) |
Steroid |
Increase water reabsorption in the kidneys by increasing sodium reabsorption; promote potassium and hydrogen ion excretion |
|
|
Epinephrine and norepinephrine |
Adrenal medulla |
Amino acidderivative |
Increase blood glucose concentrations and heart rate; dilate bronchi; alter blood flow patterns |
|
Glucagon |
Pancreas (α-cells) |
Peptide |
Stimulates glycogen breakdown (glycogenolysis); increases blood glucose concentrations |
|
Insulin |
Pancreas (β-cells) |
Peptide |
Lowers blood glucose concentrations and increases anabolic processes |
|
Somatostatin |
Pancreas (δ-cells) |
Peptide |
Suppresses secretion of glucagon and insulin |
|
Testosterone |
Testis (and adrenal cortex) |
Steroid |
Develops and maintains male reproductive system and male secondary sex characteristics |
|
Estrogen |
Ovary (and placenta) |
Steroid |
Develops and maintains female reproductive system and female secondary sex characteristics |
|
Progesterone |
Steroid |
Promotes maintenance of the endometrium |
|
|
Melatonin |
Pineal gland |
Peptide |
Involved in circadian rhythms |
|
Erythropoietin |
Kidney |
Peptide |
Stimulates bone marrow to produce erythrocytes |
|
Atrial natriuretic peptide (ANP) |
Heart (atria) |
Peptide |
Promotes salt and water excretion |
|
Thymosin |
Thymus |
Peptide |
Stimulates T-cell development |
|
Table 5.1. Major Hormones in Humans |
|||
MCAT Concept Check 5.2:
Before you move on, assess your understanding of the material with these questions.
1. For each of the hypothalamic releasing hormones listed below, what hormone(s) does each affect in the anterior pituitary? On which organ does each pituitary hormone act? What hormone(s) are released by the target organs?
|
Hypothalamic Releasing Hormone |
Hormone(s) from Anterior Pituitary |
Target Organ |
Hormone(s) Released by Target Organ |
|
Gonadotropin-releasing hormone (GnRH) |
|||
|
Corticotropin-releasing factor (CRF) |
|||
|
Thyroid-releasing hormone (TRH) |
|||
|
Dopamine |
N/A |
||
|
Growth hormone-releasing hormone (GHRH) |
N/A |
2. Which two hormones are primarily involved in calcium homeostasis? Where does each come from, and what effect does each have on blood calcium concentrations?
·
·
3. Which endocrine tissue synthesizes catecholamines? What are the two main catecholamines it produces?
4. Which two pancreatic hormones are the major drivers of glucose homeostasis? Where does each come from, and what effect does each have on blood glucose concentrations?
·
·
5. Which three hormones are primarily involved in water homeostasis? Where does each come from, and what effect does each have on blood volume and osmolarity?
·
·
·