MCAT Biology Review
Chapter 7: The Cardiovascular System
7.2 Blood
Now that we have examined the pump and the pipes through which blood travels, let’s take a look at this fluid itself.
COMPOSITION
In the pathologist’s lab, we frequently study the composition of the blood using a centrifuge. By spinning the blood at a rapid rate, we can separate this complex fluid into its components, based on density. By volume, blood is about 55% liquid and 45% cells, as shown in Figure 7.6. Plasmais the liquid portion of blood, an aqueous mixture of nutrients, salts, respiratory gases, hormones, and blood proteins. The cellular portion of blood consists of three major categories: erythrocytes, leukocytes, and platelets. All blood cells are formed from hematopoietic stem cells, which originate in the bone marrow.
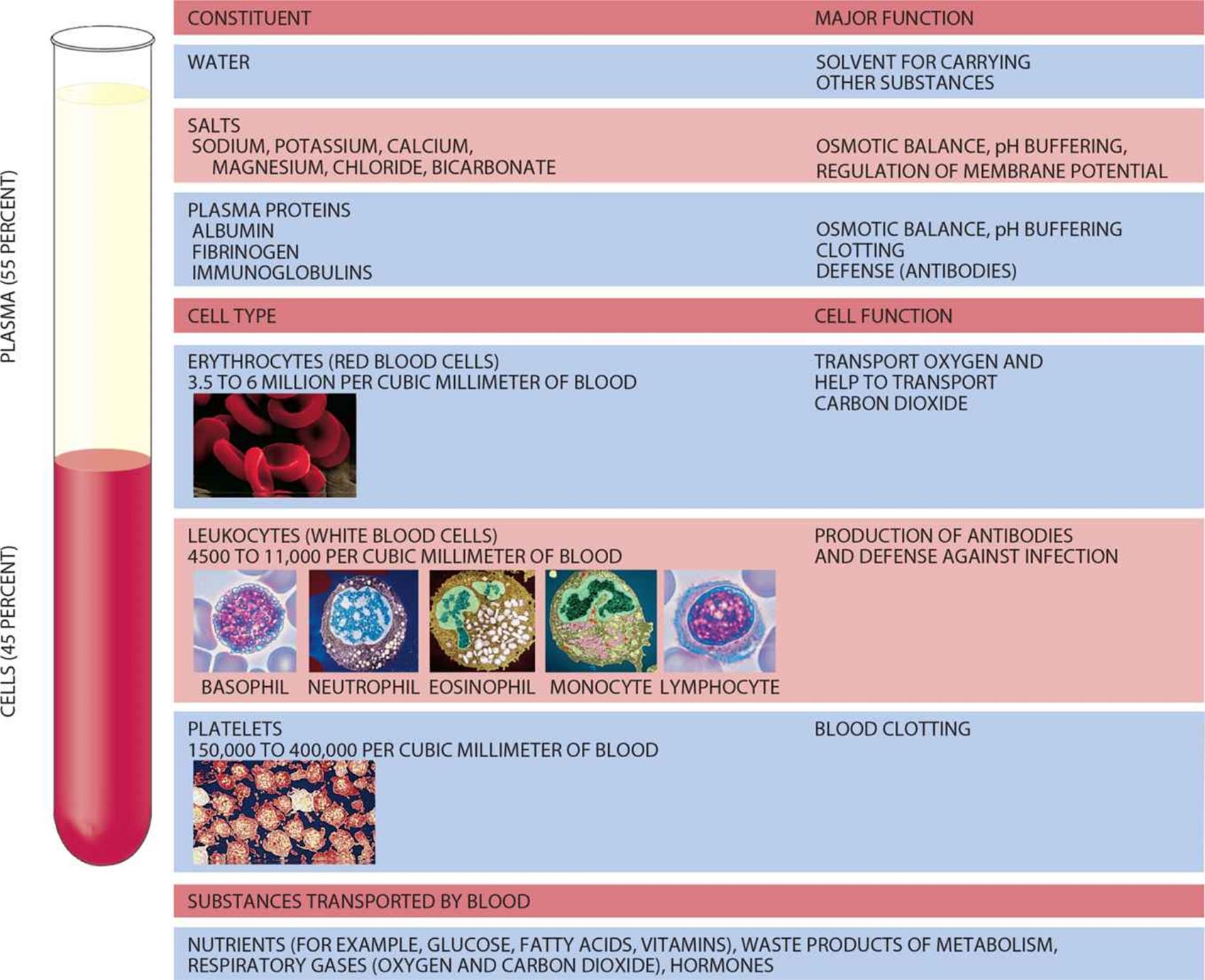 Figure 7.6. The Composition of Blood
Figure 7.6. The Composition of Blood
Erythrocytes—Red Blood Cells
In the body, oxygen and nutrients are delivered to the peripheral tissues, and carbon dioxide and other wastes (such as hydrogen ions and ammonia) are picked up from the peripheral tissues and delivered to the organs that process this waste: the lungs, liver, and kidneys. The erythrocyte orred blood cell is a specialized cell designed for oxygen transport. Oxygen does not simply dissolve in the cytoplasm of the red blood cell—remember, molecular oxygen is nonpolar and therefore has low solubility in aqueous environments. Rather, each erythrocyte contains about 250 million molecules of hemoglobin, each of which can bind four molecules of oxygen. Therefore, each red blood cell can carry approximately 1 billion molecules of oxygen.
Red blood cells are unique in a number of ways, and their modifications reflect the special role they play in the human body. Red blood cells are biconcave, or indented on both sides, which serves a dual purpose. First, this shape assists them in traveling through tiny capillaries. Second, it increases the cell’s surface area, which allows for greater gas exchange. Red blood cells are also unique in that, when they mature, the nuclei, mitochondria, and other membrane-bound organelles are lost. The loss of organelles makes space for the molecules of hemoglobin. In addition, the loss of mitochondria in particular means that the red blood cell is not able to metabolize the oxygen it is carrying before it is delivered to peripheral tissues. In other words, red blood cells do not carry out oxidative phosphorylation to generate ATP. Red blood cells rely entirely on glycolysis for the production of ATP, with lactic acid (arising from fermentation) as the main by-product. Because red blood cells lack nuclei, they are unable to divide. Erythrocytes can live for 120 days in the bloodstream before cells in the liver and spleen phagocytize senescent (old) red blood cells to recycle them for their parts.
In medicine, a complete blood count measures the quantity of each cell type in the blood. For red blood cells, two commonly given measures are the hemoglobin and hematocrit. Hemoglobin, of course, measures the quantity of hemoglobin in the blood, giving a result in grams per deciliter.Hematocrit is a measurement of how much of the blood sample consists of red blood cells, given as a percentage. A normal hemoglobin is considered to be between 13.5 and 17.5 for males and between 12.0 and 16.0 for females. For example, a patient may have a hemoglobin of 13.8![]() with a hematocrit of 41.2%. A normal hematocrit is considered to be between 41 and 53% for males and between 36 and 46% for females.
with a hematocrit of 41.2%. A normal hematocrit is considered to be between 41 and 53% for males and between 36 and 46% for females.
Leukocytes—White Blood Cells
Leukocytes or white blood cells usually comprise less than 1 percent of total blood volume. This translates into about 4500–11,000 leukocytes per microliter of blood, which is a small number relative to the erythrocyte concentration. This number can massively increase under certain conditions when we need more white blood cells, most notably during infection. White blood cells are a crucial part of the immune system, acting as our defenders against pathogens, foreign cells, cancer, and other materials not recognized as self. Let’s briefly discuss five basic types of leukocytes, which are all categorized into two classes: granulocytes and agranulocytes.
The granular leukocytes or granulocytes (neutrophils, eosinophils, and basophils) are so named because they contain cytoplasmic granules that are visible by microscopy. These granules contain a variety of compounds that are toxic to invading microbes, and their contents can be released through exocytosis. Granular leukocytes are involved in inflammatory reactions, allergies, pus formation, and destruction of bacteria and parasites. The specific functions of the three granulocytes are discussed in Chapter 8 of MCAT Biology Review.
The agranulocytes, which do not contain granules that are released by exocytosis, consist of lymphocytes and monocytes. Lymphocytes are important in the specific immune response, the body’s targeted fight against particular pathogens, such as viruses and bacteria. Some lymphocytes act as primary responders against an infection, while others function to maintain a long-term memory bank of pathogen recognition. These cells, in a very real sense, help our body learn from experience and are prepared to mount a fast response upon repeated exposure to familiar pathogens. Many vaccines work by training these cells. Through exposure to a weakened pathogen, or an antigenic protein of the pathogen (a protein that can be recognized by the immune system), memory cells can be created. For example, most children in the United States receive the varicella (chickenpox) vaccine, which includes a live but weakened strain of the varicella–zoster virus that causes chickenpox. When the vaccine is administered, the virus is recognized as foreign and an immune response is activated. During this process, certain immune cells form a memory the virus; in other words, our body learns to remember the virus and prepares itself to ward off the virus if it appears later in life.
Lymphocyte maturation takes place in one of three locations. Those lymphocytes that mature in the spleen or in lymph nodes are referred to as B-cells, and those that mature in the thymus are called T-cells. B-cells are responsible for antibody generation, whereas T-cells kill virally infected cells and activate other immune cells. The details of these two components of the specific immune response are discussed in Chapter 8 of MCAT Biology Review.
The other agranulocytes are monocytes, which phagocytize foreign matter such as bacteria. Most organs of the body contain a collection of these phagocytic cells; once they leave the bloodstream and enter an organ, monocytes are renamed macrophages. Each organ’s macrophage population may have a specific name, as well. In the central nervous system, for example, they are called microglia; in the skin, they are called Langerhans cells; in bone, they are called osteoclasts.
Thrombocytes— Platelets
Thrombocytes or platelets are cell fragments or shards released from cells in bone marrow known as megakaryocytes. Their function is to assist in blood clotting and they are present in high concentrations (150,000–400,000 per microliter of blood). The enzymatic reactions involved in the formation of a clot (the clotting cascade) will be discussed shortly.
As mentioned above, all of the cellular elements of blood originate in the bone marrow. The production of blood cells and platelets is called hematopoiesis, and is triggered by a number of hormones, growth factors, and cytokines. The most notable of these are erythropoietin, which is secreted by the kidney and stimulates mainly red blood cell development, and thrombopoietin, which is secreted by the liver and kidney and stimulates mainly platelet development. The hematopoietic pathways are shown in Figure 7.7.
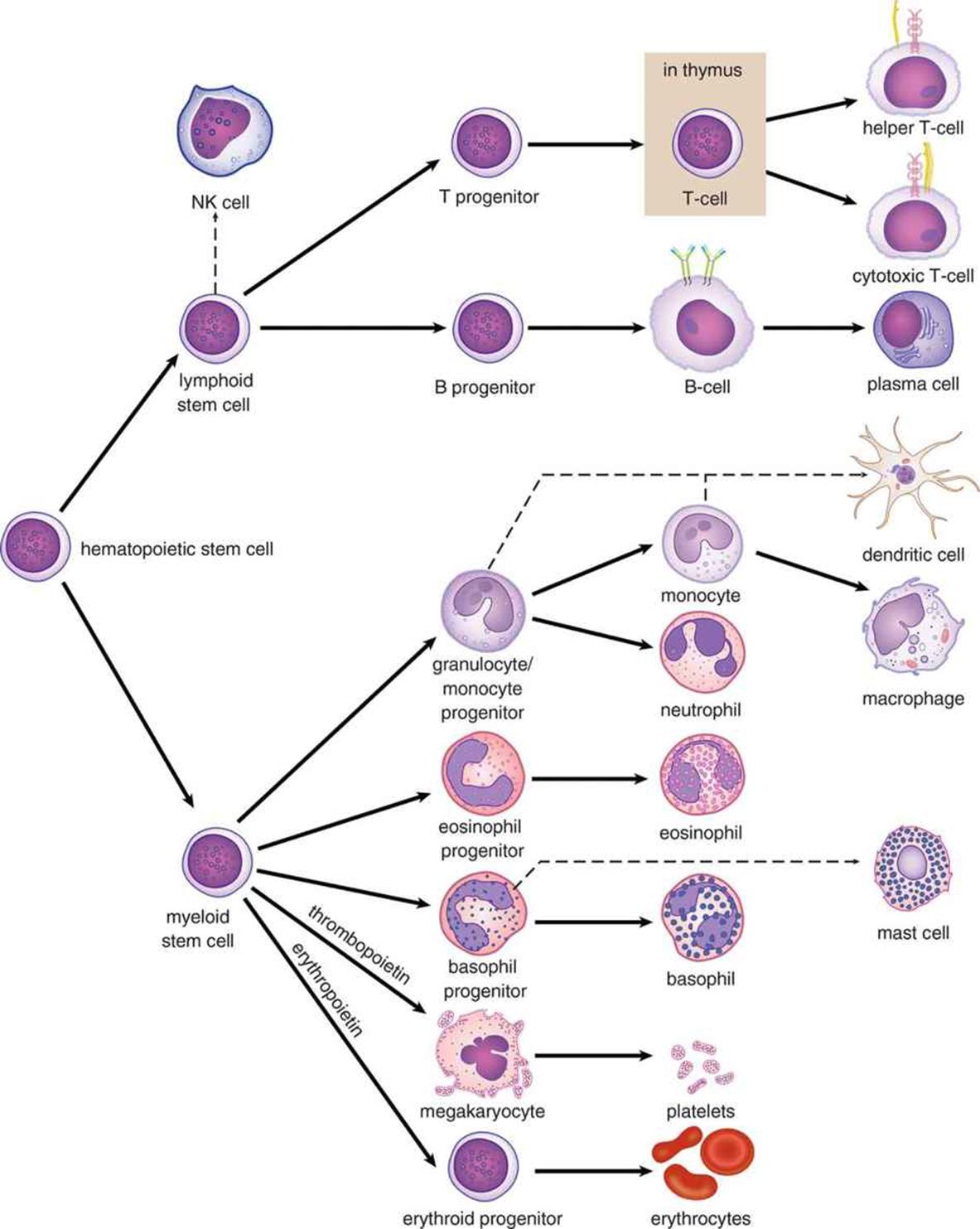 Figure 7.7. Hematopoiesis
Figure 7.7. Hematopoiesis
BLOOD ANTIGENS
Red blood cells express surface proteins called antigens. In general, an antigen is any specific target (usually a protein) to which the immune system can react. The two major antigen families relevant for blood groups are the ABO antigens and the Rh factor.
ABO Antigens
The ABO system is comprised of three alleles for blood type. In this particular class of erythrocyte cell-surface proteins, the A and B alleles are codominant, which means that a person may express one, both, or none of the ABO antigens. If the A allele (IA or simply A) is present on one chromosome and the B allele (IB or B) is present on the other chromosome, both will be expressed, and the person’s blood type will be AB. The O allele (i or O) is recessive to both the A and B alleles. People with type O blood do not express either variant of this protein and have a homozygous recessive genotype. The naming system of blood types is based on the presence or absence of these protein variants. The four blood types are: A, B, AB, and O. Because the A and B alleles are dominant, the genotypes for A may be IAIA or IAi, while the genotypes for B may be IBIB or IBi.
MCAT EXPERTISE
There are two different ways of writing the ABO alleles: IA, IB, and i; or A, B, and O. Be comfortable using either system because the MCAT could show one or the other. Because the former system is more common in medical practice, we’ll be using it throughout this book.
The ABO classification has important implications for medical practice; it is critical to match blood types for transfusions. It is no exaggeration to say that blood-type matching is a life and death matter, given the severe hemolysis that can result if the donor blood antigen is recognized as foreign by the recipient’s immune system. For example, a person with type A blood will recognize the type A protein as self but the type B protein as foreign and will make antibodies to type B. Because type O blood cells express neither antigen variant, they will not initiate any immune response, regardless of the recipient’s actual blood type; people with type O blood are therefore considered universal donors because their blood will not cause ABO-related hemolysis in any recipient. However, a recipient who is type O will produce both anti-A and anti-B antibodies and can only receive blood from other type O individuals. On the other hand, people with type AB blood are considered universal recipients because they can receive from all blood types: No blood antigen is foreign to AB individuals, so no adverse reactions will occur upon transfusion. A more thorough description of each blood type is given in Table 7.1. Note that whole blood is almost never given in a transfusion; rather, packed red blood cells (with no plasma) are generally given. Thus, we care only about the donor’s red blood cell antigens (and not his or her plasma antibodies) when determining whether hemolysis will occur.
Another important point needs to be made here about antibodies. Antibodies are created in response to an antigen, and they specifically target that antigen. You would not expect to have antibodies to the Ebola virus if you had never been exposed to it. This is true for the Rh factor as well—an Rh-negative individual would not have anti-Rh antibodies prior to exposure to Rh-positive blood. Why, then, does an individual lacking the A allele automatically have an anti-A antibody? The reason may lie in the gut: research has demonstrated that E. coli that inhabit the colon may have proteins that match the A and B alleles. This would serve as a source of exposure and would allow one to develop anti-A (or anti-B) antibodies prior to exposure to another person’s blood. This is why ABO compatibility is so important during blood transfusions—giving the wrong ABO blood type would lead to rapid hemolysis.
|
Blood Type |
Genotype(s) |
Antigens Produced |
Antibodies Produced |
Can Donate to… |
Can Receive from… |
|
A |
IAIA, IAi |
A |
anti-B |
A, AB |
A, O |
|
B |
IBIB, IBi |
B |
anti-A |
B, AB |
B, O |
|
AB |
IAIB |
A and B |
none |
AB only |
A, B, AB, O (universal recipient) |
|
O |
ii |
none |
anti-A and anti-B |
A, B, AB, O (universal donor) |
O only |
|
Table 7.1 ABO Blood Types |
|||||
MCAT EXPERTISE
You are almost guaranteed to see at least one question on blood groups on Test Day. It is critical that you learn how the system works (IA and IB are codominant, i is recessive).
KEY CONCEPT
Antigens are the stimuli for B-cells to make antibodies. After exposure of a B-cell to its specific antigen, the cell becomes an antibody-producing factory.
REAL WORLD
The most common blood type in the United States is O+. The least common is AB–.
Rh Factor
The Rh factor (so named because it was first described in rhesus monkeys) is also a surface protein expressed on red blood cells. Although at one time it was thought to be a single antigen, it has since been found to exist as several variants. When left unmodified, Rh-positive (Rh+) or Rh-negative (Rh–) refers to the presence or absence of a specific allele called D. The presence or absence of D can also be indicated with a plus or minus subscript on the ABO blood type (such as O+, or AB–). Rh-positivity follows autosomal dominant inheritance; one positive allele is enough for the protein to be expressed.
REAL WORLD
In blood-bank pathology, the Rh factor is often referred to as D. Note that while the A, B, and D proteins are the most important for blood typing, dozens of other antigens can (and should) be matched as well, including C, E, Kell, Lewis, Duffy, and others. The more antigens that are correctly matched, the lower the probability of hemolysis.
The Rh factor status is particularly important in maternal–fetal medicine. During childbirth, no matter how good the obstetrician is, women are exposed to a small amount of fetal blood. If a woman is Rh– and her fetus is Rh+, she will become sensitized to the Rh factor, and her immune system will begin making antibodies against it. This is not a problem for the first child; by the time the mother starts producing antibodies, the child has already been born. However, any subsequent pregnancy in which the fetus is Rh+ will present a problem because maternal anti-Rh antibodies can cross the placenta and attack the fetal blood cells, resulting in hemolysis of the fetal cells. This condition is known as erythroblastosis fetalis and can be fatal to the fetus. Today, we can use medicine to prevent this condition. There is less concern with ABO mismatching between mother and fetus because these maternal antibodies are of a class called IgM, which does not readily cross the placenta (unlike anti-Rh IgG antibodies, which can).
REAL WORLD
When an Rh– woman is pregnant with an Rh+ fetus, the risk of erythroblastosis fetalis in subsequent Rh-mismatched pregnancies can usually be avoided by giving the Rh– mother Rh-immunoglobulin (RhoGAM) during pregnancy and immediately after delivery. Administration of immunoglobulin (which is a type of passive immunization) will absorb the fetus’s Rh+ cells, preventing the production of anti-Rh antibodies.
MCAT Concept Check 7.2:
Before you move on, assess your understanding of the material with these questions.
1. What are the components of plasma?
2. An individual with B+ blood is in an automobile accident and requires a blood transfusion. What blood types could he receive? The same individual is so thankful that, after recovery, he decides to donate blood. To which blood types could he donate?
· Could receive from:
· Could donate to:
3. What does a hematocrit measure? What are the units for hematocrit?
4. Which types of leukocytes are involved in the specific immune response?
5. Where do platelets come from?
6. Which cell type(s) in blood contain nuclei? Which do not?
· Contain nuclei:
· Do not contain nuclei: