Biology of Humans
12. The Cardiovascular and Lymphatic Systems
In the previous chapter, we learned about blood—its components and functions. In this chapter, we consider how the blood circulates throughout the body by examining the blood vessels and the heart. We will also learn about the network of vessels and other structures that make up the lymphatic system. Together, the heart and blood vessels and the lymphatic system constitute the circulatory system.
Cardiovascular System
The cardiovascular system consists of the heart—a muscular pump that contracts rhythmically and provides the force that moves the blood—and the blood vessels—a system of tubules through which blood flows (Figure 12.1). The blood delivers a continuous supply of oxygen and nutrients to the cells of the body and carries away metabolic waste products so that they cannot poison the cells.
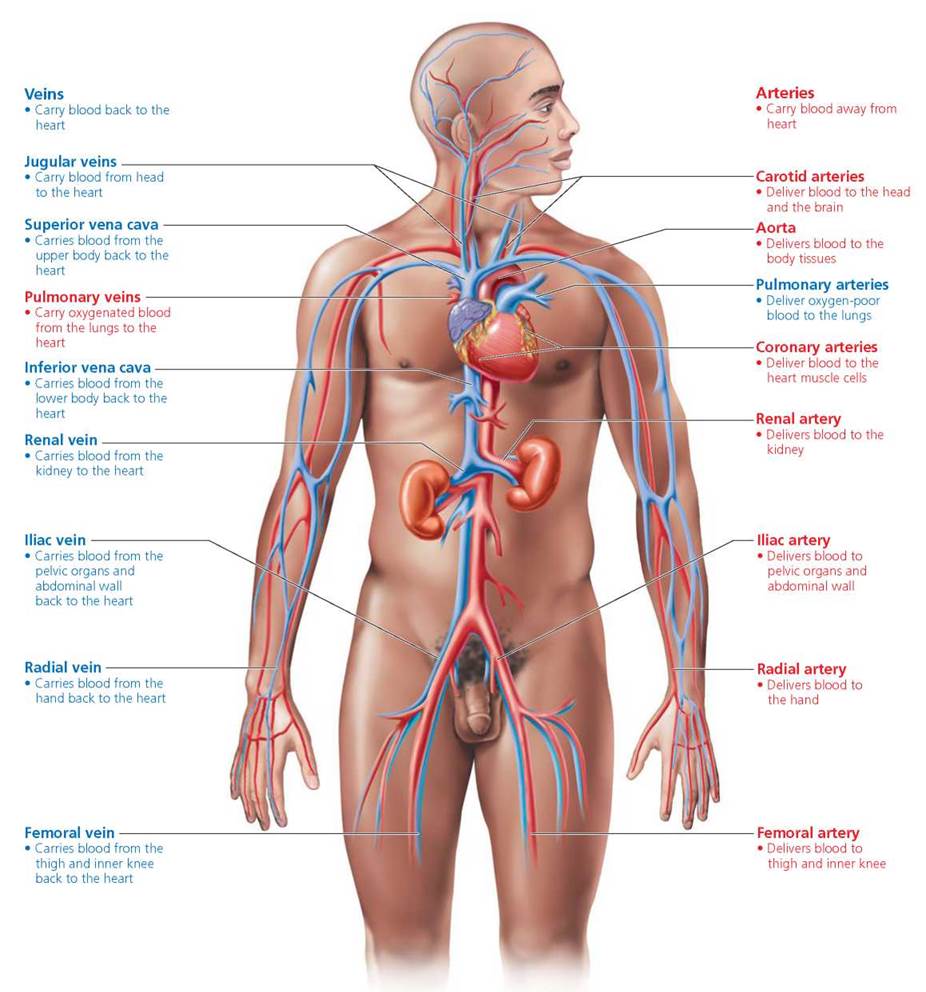
FIGURE 12.1. A diagrammatic view of the cardiovascular system (heart and blood vessels). Throughout this chapter, red indicates blood that is high in oxygen. Blue indicates blood that is low in oxygen.
Why is the cardiovascular system so critical to survival? It is the body's transportation network, similar in some ways to the highways within a country. Our bodies are too large and complex for diffusion alone to distribute materials efficiently. The cardiovascular system provides a means for distributing vital chemicals from one part of the body to another quickly enough to sustain life. The cardiovascular system is more than just a passive system of pipelines, however. The heart rate and the diameter of certain blood vessels are continually being adjusted in prompt response to the body's changing needs.
· The cardiovascular system consists of a pump— the heart—and a loop of blood vessels. All the organs of the body require a continuous supply of blood to deliver oxygen and nutrients, and to remove waste. This blood supply is particularly important for the heart—the hardest working muscle in the body. If the blood vessels of the heart become clogged, steps must be taken to restore adequate blood flow.
Blood Vessels
Once every minute, or about 1440 times each day, the blood moves through a life-sustaining circuit. The circuit of blood vessels is extensive. Indeed, if all the vessels in an average adult's body were placed end to end, they would stretch about 100,000 km (60,000 mi), long enough to circle Earth's equator more than twice!
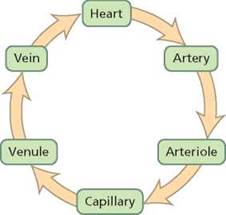
The blood vessels do not form a single long tube. Instead, they are arranged in branching networks. With each circuit through the body, blood is carried away from the heart in arteries, which branch to give rise to narrower vessels called arterioles. Arterioles lead into networks of microscopic vessels called capillaries, which allow the exchange of materials between the blood and body cells. The capillaries eventually merge to form venules, which in turn join to form larger tubes called veins. The venules and veins return the blood to the heart.
All blood vessels share some common features, but each type also has its own traits and is marvelously adapted for its specific function (Figure 12.2). The hollow interior of a blood vessel, through which the blood flows, is called the lumen. The inner lining that comes into contact with the blood flowing through the lumen is composed of simple squamous epithelium (the flattened, tight-fitting cells we encountered in Chapter 4). This lining, called the endothelium, provides a smooth surface that minimizes friction so that the blood flows easily. The lumen and endothelium are characteristic of all blood vessels.
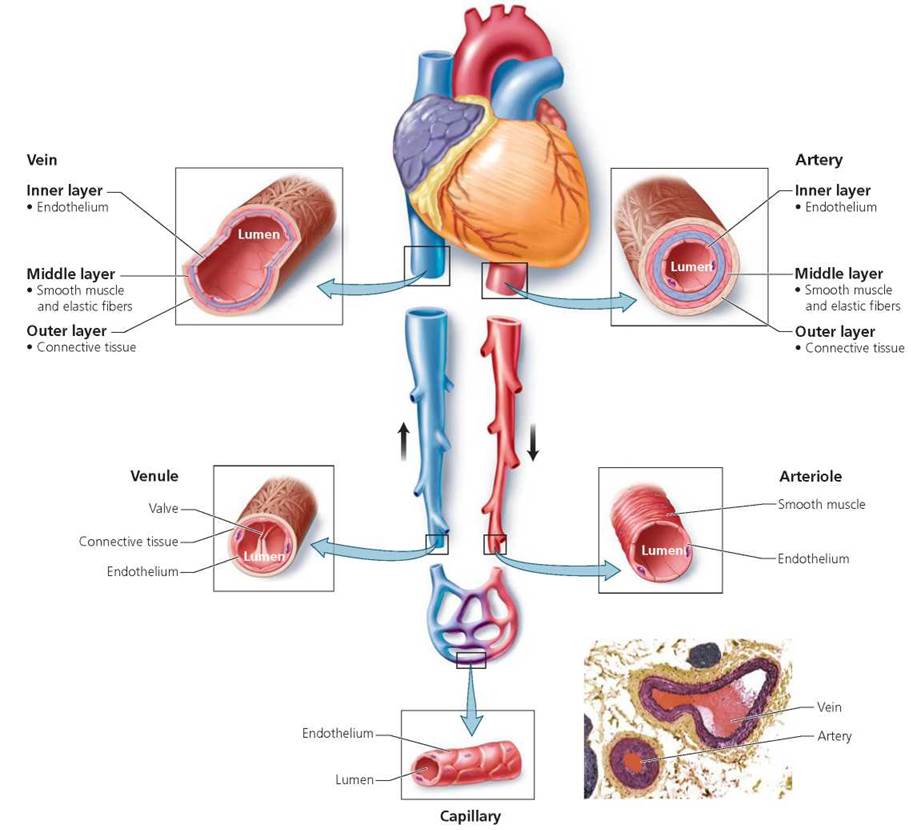
FIGURE 12.2. The structure of blood vessels
Arteries
Arteries are muscular tubes that transport blood away from the heart, delivering it rapidly to the body tissues. As noted, the innermost layer of an arterial wall is the endothelium. Immediately outside the endothelium is a middle layer that contains elastic fibers and circular layers of smooth muscle. The elastic fibers allow an artery to stretch and then return to its original shape. The smooth muscle enables the artery to contract. The outer layer of an arterial wall is a sheath of connective tissue that contains elastic fibers and collagen. This layer adds strength to the arterial wall and anchors the artery to surrounding tissue.
The elastic fibers in the middle layer of an artery have two important functions: (1) They help the artery tolerate the pressure shock caused by blood surging into it when the heart contracts, and (2) they help maintain a relatively even pressure within the artery, despite large changes in the volume of blood passing through it. Consider, for instance, what happens when the heart contracts and sends blood into the aorta, the body's main artery. Each beat of the heart causes 70 ml (about one- fourth cup) of blood to pound against the wall of the aorta like a tidal wave. A rigid pipe could not withstand the repeated pressure surges, but the elastic walls of the artery stretch with each wave of blood and return to their original size when the surge has moved past; this results in a continuous stream of blood rather than intermittent waves.
The alternate expansion and recoil of arteries create a pressure wave, called a pulse, that moves along the arteries with each heartbeat. Thus, the pulse rate is the same as the heart rate. You can feel the pulse by slightly compressing with your fingers any artery that lies near the body's surface, such as the one at the wrist or the one under the angle of the jaw.
As previously mentioned, the middle layer of an artery wall also contains smooth muscle that enables the artery to contract. When this circular muscle contracts and the diameter of the lumen becomes narrower, a process called vasoconstriction, blood flow through the artery is reduced. On the other hand, when the smooth muscle relaxes and the arterial lumen increases in diameter, a process called vasodilation, blood flow through the artery increases. The smooth muscle is best developed in small- to medium-sized arteries. These arteries serve to regulate the distribution of blood, adjusting flow to suit the needs of the body.
We see the importance of the strength of an artery wall when it becomes weakened, as might occur due to disease, inflammation, injury, or a birth defect. When the arterial wall becomes weakened, the pressure of the blood flowing through the weakened area may cause the wall to swell outward like a balloon, forming an aneurysm. Most aneurysms do not cause symptoms, but the condition can be threatening just the same. The primary risk is that the aneurysm will burst, causing blood loss. The tissues serviced by that vessel will then be deprived of oxygen and nutrients, a situation that can be fatal. Even if the aneurysm does not rupture, it can cause the formation of life-threatening blood clots. A clot can break free from the site of formation and float through the circulatory system until it lodges in a small vessel, where it can block blood flow and cause tissue death beyond that point. In some cases, an aneurysm can be repaired surgically. The risk of blood clots and aneurysms is exacerbated by the nicotine in tobacco products.
The smallest arteries, called arterioles, are barely visible to the unaided eye. Their walls have the same three layers found in arteries; but the middle layer is primarily smooth muscle with only a few elastic fibers, and the outer layer is much thinner.
Arterioles have two extremely important regulatory roles. First, they are the prime controllers of blood pressure, which is the pressure of blood against the vessel walls (discussed later in this chapter). When the muscle in arteriole walls contracts, blood pressure increases. The greater the number of arterioles contracted, the higher the blood pressure. Relaxation of arteriole walls lowers blood pressure. Second, they serve as gatekeepers to the capillary networks. A capillary network can be open or closed, depending on whether the smooth muscle in the walls of the arteriole leading to it allows blood through. In this way, arterioles can regulate the amount of blood sent to cells based on those cell's immediate needs. Arterioles are constantly responding to input from hormones, the nervous system, and local conditions, modifying blood pressure and flow to meet the body's changing needs.
Capillaries
Capillaries are microscopic blood vessels that connect arterioles and venules. The capillaries are well suited to their primary function: the exchange of materials between the blood and the body cells (Figure 12.3). Capillary walls are only one cell layer thick, and so substances move easily between the blood and the fluid surrounding the cells outside the capillary. The plasma membrane of the capillary's endothelial cells is an effective and selective barrier that determines which substances can cross. Some substances that cross the capillary walls do not pass through the endothelial cells. Instead, these substances filter through small slits between adjacent endothelial cells. The slits between the cells are just large enough for some fluids and small dissolved molecules to pass through.
The design of the capillary networks allows blood flow through capillaries to be adjusted to deliver the necessary amount of oxygen and nutrients to meet the needs of particular regions of the body. The network of capillaries servicing you dive into the water and start swimming, the capillary beds of the digestive organs will close down, and those in the skeletal muscles will open.
Collectively, the capillaries provide a tremendous surface area for the rapid exchange of materials between body and blood. Capillary beds bring capillaries very close to nearly every cell. Your fingernails provide windows that allow you to appreciate the efficiency with which capillary networks reach all parts of the body. You may have noticed that the tissue beneath a fingernail normally has a pink tinge. The color results from blood flowing through numerous capillaries there. Gentle pressure on the nail causes the tissue to turn white as the blood is pushed from those capillaries.
A capillary is so narrow that red blood cells must squeeze through single file. Despite their size, there are so many capillaries that their combined cross-sectional area is enormous, much greater than that of the arteries or veins. Because of the large cross-sectional area of the capillaries, the blood flows much more slowly through them than through the arteries or veins. The slower rate of flow in the capillaries provides more time for the exchange of materials (Figure 12.5).
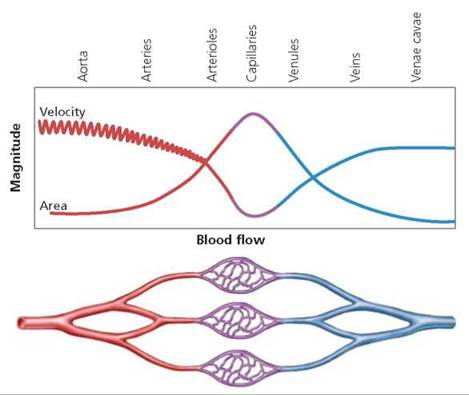
FIGURE 12.5. The capillaries are so numerous that their total crosssectional area is much greater than that of arteries or veins. Thus, blood pressure drops and blood flows more slowly as it passes through a capillary bed. The slower rate of flow allows time for the exchange of materials between the blood and the tissues.
Veins
After the capillary bed, capillaries merge to form the smallest kind of vein, a venule. Venules then join to form larger veins. Veins are blood vessels that return the blood to the heart.
Although veins share some structural features with arteries, there are also some important differences. The walls of veins have the same three layers found in arterial walls, but the walls of veins are thinner and the lumens of veins are larger than those of arteries of equal size (see Figure 12.2). The thin walls and large lumens allow veins to hold a large volume of blood. Indeed, veins serve as blood reservoirs, holding up to 65% of the body's total blood supply.
The same amount of blood that is pumped out of the heart must be conducted back to the heart, but it must be moved through the veins without assistance from the high pressure generated by the heart's contractions. In the head and neck, of course, gravity helps move blood toward the heart. But how is it possible to move blood against the force of gravity—from the foot back to the heart, for instance (unless, by chance, your foot was in your mouth)?
Three mechanisms move blood from lower parts of the body toward the heart:
1. Valves in veins prevent backflow of blood. Veins often contain valves that act as one-way turnstiles, allowing blood to move toward the heart but preventing it from flowing backward. These valves are pockets of connective tissue projecting from the lining of the vein, as shown in Figure 12.6a.
A simple experiment can demonstrate the effectiveness of venous valves. Allow your hand to hang by your side until the veins on the back of your hand become distended. Place two fingertips from the other hand at the end of one of the distended veins nearest to the knuckles. Then, leaving one fingertip pressed on the end of the vein, move the other toward the wrist, pressing firmly and squeezing the blood from the vein. Lift the fingertip near the knuckle and notice that blood immediately fills the vein. Repeat the procedure, but this time lift the fingertip near the wrist. You will see the vein remains flattened, because the valves prevent the backward flow of blood.
2. Contraction of skeletal muscle squeezes veins. Virtually every time a skeletal muscle contracts, it squeezes nearby veins. This pressure pushes blood past the valves toward the heart. The mechanism propelling the blood is similar to the one that causes toothpaste to squirt out of the uncapped end of the tube regardless of where the tube is squeezed; valves in veins ensure that blood flows in only one direction. When skeletal muscles relax, any blood that moves backward fills the valves. As the valves fill with blood, they extend further into the lumen of the vein, closing the vein and preventing the flow of blood from reversing direction (Figure 12.6b). Thus, the skeletal muscles are always squeezing the veins and driving blood toward the heart.
3. Breathing causes pressure changes that move blood toward the heart. The thoracic (chest) cavity increases in size when we inhale (see Chapter 14). The expansion reduces pressure within the thoracic cavity and at the same time increases pressure in the abdominal cavity. Blood naturally moves toward regions of lower pressure. Thus, the reduced pressure in the thoracic cavity that comes with each breath pulls blood back toward the heart. In addition, the increased pressure in the abdominal cavity squeezes veins, also forcing blood back toward the heart.
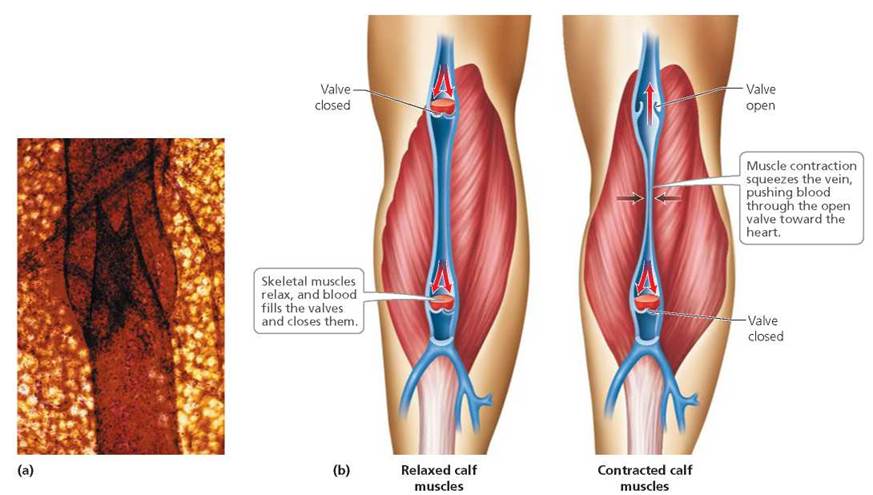
FIGURE 12.6. (a) A micrograph of a vein showing a valve. (b) Pocketlike valves on the inner surface of veins assist the return of blood to the heart against gravity by preventing backflow.
Stop and think
If an artery is cut, blood is lost in rapid spurts. In contrast, blood loss through a cut vein has an even flow. What accounts for these differences?
Heart
The heart is about the size of a fist, but it is an incredible muscular pump that generates the force needed to circulate blood. It beats about 72 times a minute, every hour of every day— although this rate varies with age, physical fitness, and current physical exertion. To appreciate the work done by the heart, alternately clench and relax a fist 70 times a minute. How many minutes does it take before the muscles of your hand are too tired to continue? In contrast, the healthy heart does not fatigue. It beats more than 100,000 times each day, which adds up to about 2 billion beats over a lifetime. The volume of blood pumped by the heart is equally remarkable. It pumps slightly less than 5 liters (10 pt) of blood a minute through its chambers, which adds up to more than 9400 liters (2500 gal) per day.
The heart has three layers, each one contributing to the heart's ability to function as a pump. The wall of the heart, called the myocardium, is mostly cardiac muscle tissue. The myocardium's contractions are responsible for the heart's incredible pumping action. The endocardium is a thin lining in the cavities of the heart. By reducing friction, the endocardium's smooth surface lessens the resistance to blood flow through the heart. The pericardium is a thick, fibrous sac that holds the heart in the center of the chest (thoracic) cavity and slides over the surface of the heart without hampering its movements, even when they are vigorous.
Although the heart appears to be a single structure, it actually has two halves, with the right and left halves functioning as two separate pumps. As we will see shortly, the right side of the heart pumps blood to the lungs, where it picks up oxygen. The left side pumps the blood to the body cells. The two pumps are physically separated by a partition called a septum. Each half of the heart consists of two chambers: an upper chamber, called an atrium (plural, atria), and a lower chamber, called a ventricle (Figure 12.7). The two atria function as receiving chambers for the blood returning to the heart. The two ventricles function as the main pumps of the heart. Contraction of the ventricles forces blood out of the heart under great pressure. When we think about the work of the heart, we are in fact thinking about the work of the ventricles. It should not be surprising, then, that the ventricles are much larger chambers than the atria and have thicker, more muscular walls.
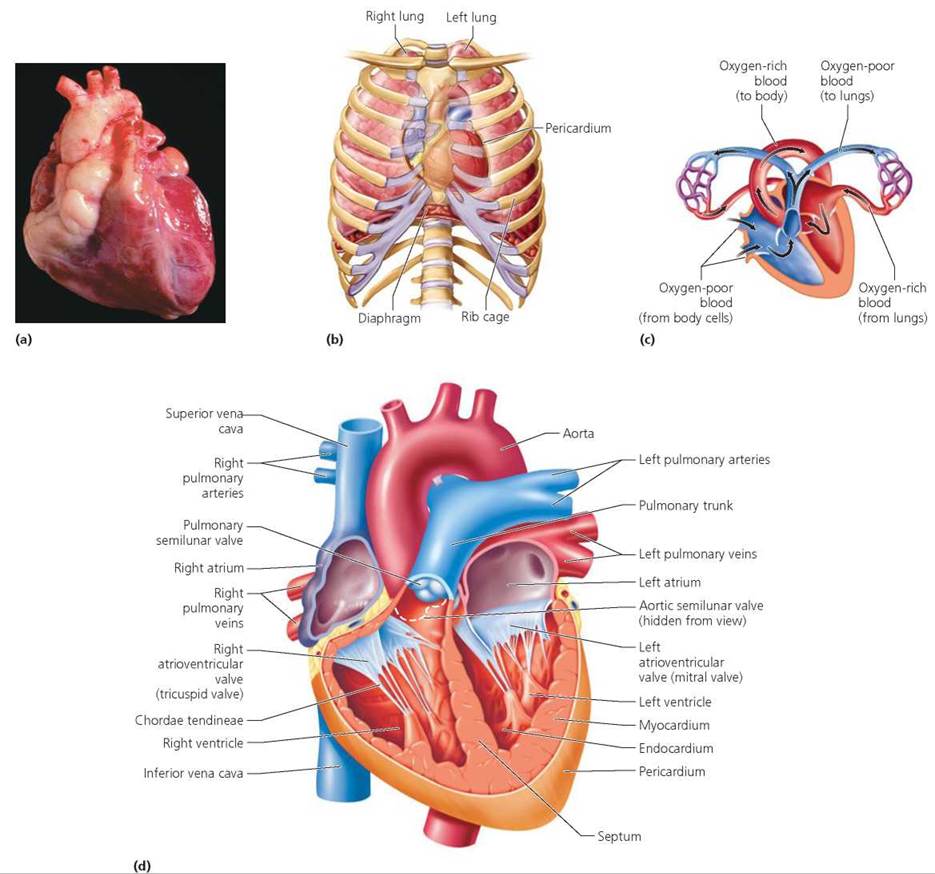
FIGURE 12.7. (a) The human heart, (b) The heart is located in the thoracic (chest) cavity. (c) Blood flows through the heart from the atria to the ventricles, (d) This diagram of a human heart shows the four chambers, the major vessels connecting to the heart, and the two pairs of heart valves.
When the ventricles contract, which valves would open and which valves would close?
The semilunar valves would open and the AV valves would close.
Two pairs of valves ensure that the blood flows in only one direction through the heart. The first pair is the atrioventricular (AV) valves, each leading from an atrium to a ventricle, as shown in Figure 12.8. The AV valves are connective tissue flaps, called cusps, anchored to the wall of the ventricle by strings of connective tissue called the chordae tendineae—the heartstrings. These strings prevent the AV valves from flapping back into the atria under the pressure developed when the ventricles contract. The AV valve on the right side of the heart has three flaps and is called the tricuspid valve. The AV valve on the left side of the heart has two flaps and is called the bicuspid, or mitral, valve.
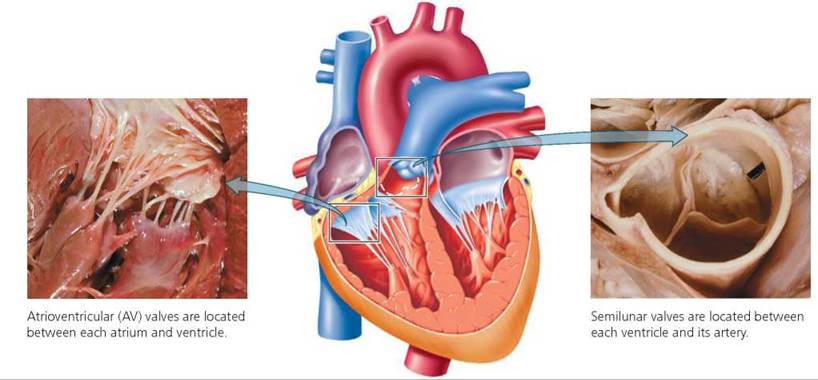
FIGURE 12.8. The valves of the heart keep blood flowing In one direction.
Each of the second pair of valves, the semilunar valves, is located between a ventricle and its connecting artery— either the aorta or the pulmonary artery. The cusps of the semilunar valves are small pockets of tissue attached to the inner wall of the respective artery. When the pressure in the arteries becomes greater than the pressure in the ventricles, these valves fill with blood in a manner similar to a parachute filling with air. In this way, the semilunar valves prevent the backflow of blood into the ventricles from the aorta or pulmonary artery.
Two Circuits of Blood Flow
As we mentioned, the left and right sides of the heart function as two separate pumps, each circulating the blood through a different route, as shown in Figure 12.9. Note that in both circuits the blood moves through the arteries, arterioles, capillaries, and venules before returning to the heart via the veins. The right side of the heart pumps blood through the pulmonary circuit, which transports blood to and from the lungs. The left side of the heart pumps blood through the systemic circuit, which transports blood to and from body tissues. This arrangement prevents oxygenated blood (blood rich in oxygen) from mixing with blood that is low in oxygen.
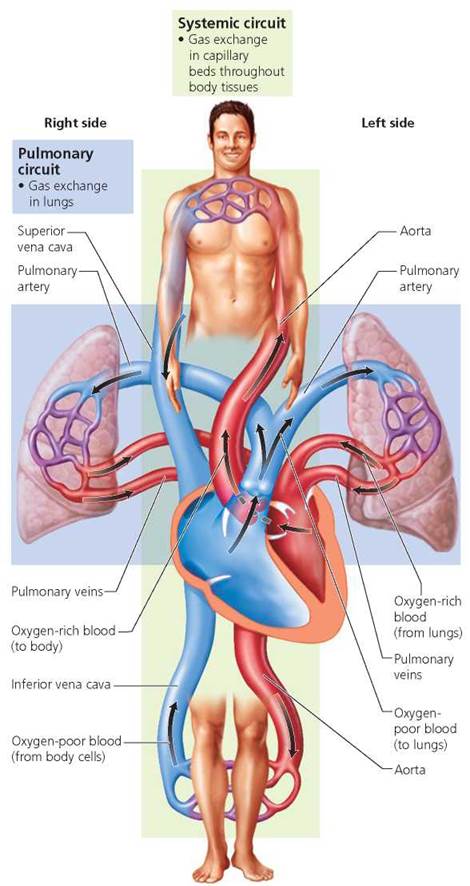
FIGURE 12.9. Circuits of blood flow. The right side of the heart pumps blood through the pulmonary circuit, which carries blood to and from the lungs. The left side of the heart pumps blood through the systemic circuit, which conducts blood to and from the body tissues.
The pulmonary circuit begins in the right atrium, as veins return oxygen-poor blood from the systemic circuit. (You can trace the flow of blood through the heart in the pulmonary and systemic circuits in Figure 12.9 as you read the following description.) The blood then moves from the right atrium to the right ventricle. Contraction of the right ventricle pumps poorly oxygenated blood to the lungs through the pulmonary trunk (main pulmonary artery), which divides to form the left and right pulmonary arteries. In the lungs, oxygen diffuses into the blood, and carbon dioxide diffuses out. The now oxygen- rich blood is delivered to the left atrium through four pulmonary veins, two from each lung. (Note that the pulmonary circulation is an exception to the general rule that arteries carry oxygen-rich blood and veins carry oxygen-poor blood. Exactly the opposite is true of vessels in the pulmonary circulation.) The pathway of blood pumped through the pulmonary circuit by the right side of the heart is
Right atrium → AV valve (tricuspid) → Right ventricle → Pulmonary semilunar valve → Pulmonary trunk → Pulmonary arteries → Lungs → Pulmonary veins → Left atrium
The systemic circuit begins when oxygen-rich blood enters the left atrium (see Figure 12.9). Blood then flows to the left ventricle. When the left ventricle contracts, oxygenated blood is pushed through the largest artery in the body, the aorta. The aorta arches over the top of the heart and gives rise to the smaller arteries that eventually feed the capillary beds of the body tissues. The venous system collects the oxygen-depleted blood and eventually culminates in veins that return the blood to the right atrium. These veins are the superior vena cava, which delivers blood from regions above the heart, and the inferior vena cava, which returns blood from regions below the heart. Thus, the pathway of blood through the systemic circuit pumped by the left side of the heart is
Left atrium → AV (bicuspid or mitral) valve → Left ventricle → Aortic semilunar valve → Aorta → Body tissues → Inferior vena cava or superior vena cava → Right atrium
The familiar sounds of the heart, which are often described as "lub-dup," are associated with the closing of the valves. The first heart sound ("lub") is produced by the turbulent blood flow when the AV valves snap shut as the ventricles begin to contract. The higher-pitched second heart sound ("dup") is produced by the turbulent blood flow when closure of the semilunar valves and the beginning of ventricular relaxation occur.
Heart murmurs, which are swooshing heart sounds other than lub-dup, are created by disturbed blood flow. Although heart murmurs are sometimes heard in normal, healthy people, they can also indicate a heart problem. For instance, malfunctioning valves often disturb blood flow through the heart, causing the swishing or gurgling sounds of heart murmurs. Several conditions can cause valves to malfunction. In some cases, thickening of the valves narrows the opening and impedes blood flow. In other cases, the valves do not close properly and, therefore, allow the backflow of blood. In either case, the heart is strained because it must work harder to move the blood.
Coronary Circulation
Cells of the heart muscle themselves obtain little nourishment from blood flowing through the heart's chambers. Instead, an extensive network of vessels, known as the coronary circulation, services the tissues of the heart. The first two arteries that branch off the aorta are the coronary arteries (Figure 12.10). These arteries give rise to numerous branches, ensuring that the heart receives a rich supply of oxygen and nutrients. After passing through the capillary beds that nourish the heart tissue, blood enters cardiac veins and eventually flows into the right atrium.
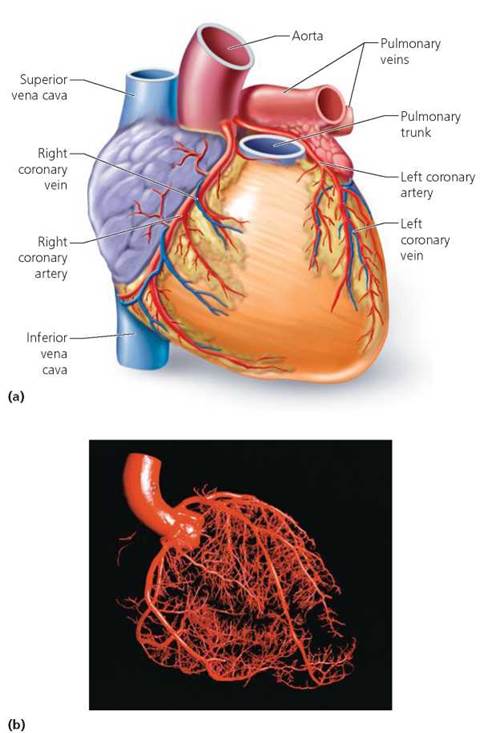
FIGURE 12.10. Coronary circulation, (a) The coronary vessels deliver a rich supply of oxygen and nutrients to the heart muscle cells and remove the metabolic wastes, (b) This cast of the coronary blood vessels reveals the complexity of the coronary circuit.
Cardiac Cycle
Although the two sides of the heart pump blood through different circuits, they work in tandem. The two atria contract simultaneously, and then the two ventricles contract simultaneously.
We see, then, that a heartbeat is not a single event. Each beat involves contraction, which is called systole (sis'-to-lee) and relaxation, which is called diastole (di-as'-to-lee). All the events associated with the flow of blood through the heart chambers during a single heartbeat are collectively called the cardiac cycle, as illustrated in Figure 12.11. First, all chambers relax (diastole) and blood passes through the atria and enters the ventricles. When the ventricles are about 70% filled, the atria contract (atrial systole) and push their contents into the ventricles. The atria then relax (atrial diastole), and the ventricles begin their contraction phase (ventricular systole). Upon completion of this contraction, the whole heart again relaxes. If we were to add the contraction time of the heart during a day and compare it with the relaxation time during a day, the heart's workday might turn out to be equivalent to yours. In 24 hours, the heart spends a total of about 8 hours working (contracting) and 16 hours relaxing. However, unlike your workday, the heart's day is divided into repeating cycles of work and relaxation.
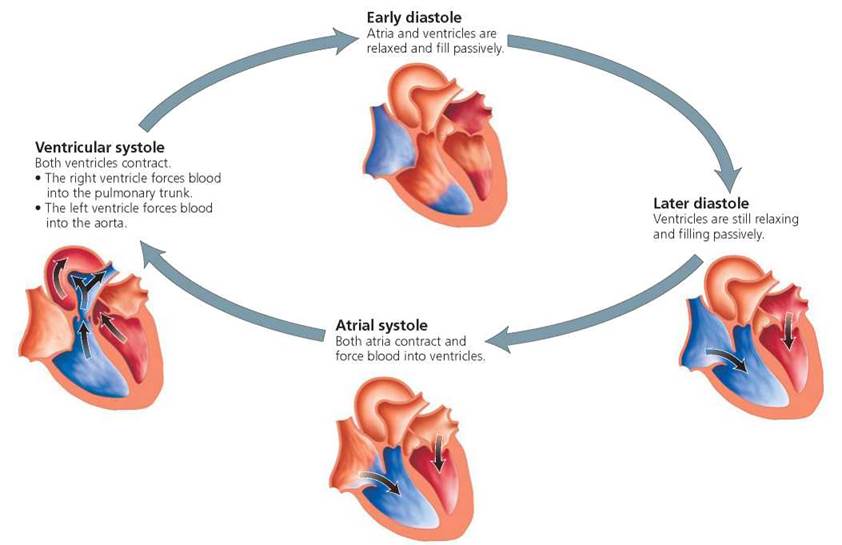
FIGURE 12.11. The cardiac cycle is all of the events associated with the flow of blood through the heart during each heartbeat. The atria contract together, and the ventricles contract together. Red indicates blood high in oxygen. Blue indicates blood low in oxygen.
Internal Conduction System
If a human heart is removed, as in a transplant operation, and placed in a dish, it will continue to beat, keeping a lonely and useless rhythm until its tissues die. In fact, if a few cardiac muscle cells are grown in the laboratory, they, too, will beat on their own, each twitch a reminder of the critical role the intact organ plays. Clearly, then, the heart muscle does not require outside stimulation to beat. Instead, the tendency is intrinsic, within the heart muscle itself.
Another remarkable observation has been made of heart muscle cells grown in a laboratory dish. Although isolated heart cells twitch independently of each other, if two cells should touch, they will begin beating in unison. This, too, is an inherent property of the cells, but it is partly due to the type of connections between heart muscle cells. The cell membranes of adjacent cardiac muscle cells interweave with one another at specialized junctions called intercalated disks. Cell junctions in the intercalated disks mechanically and electrically couple the connected cells. Adjacent cells are held together so tightly that they do not rip apart during contraction but instead transmit the pull of contraction from one cell to the next. At the same time, the junctions permit electrical communication between adjacent cells, allowing the electrical events responsible for contraction to spread rapidly over the heart by passing from cell to cell. Yet even though heart cells contract automatically, they still need some outside control to contract at the proper rate.
The tempo of the heartbeat is set by a cluster of specialized cardiac muscle cells, called the sinoatrial (SA) node, located in the right atrium near the junction of the superior vena cava (Figure 12.12). Because the SA node sends out the impulses that initiate each heartbeat, it is often referred to as the pacemaker. About 70 to 80 times a minute, the SA node sends out an electrical signal that spreads through the muscle cells of the atria, causing them to contract. The signal reaches another cluster of specialized muscle cells called the atrioventricular (AV) node, located in the partition between the two atria, and stimulates it. The AV node then relays the stimulus by means of a bundle of specialized muscle fibers, called the atrioventricular bundle, that runs along the wall between the ventricles. The bundle forks into right and left branches and then divides into many other specialized cardiac muscle cells, called Purkinje fibers, that penetrate the walls of the ventricles. The rapid spread of the impulse through the ventricles ensures that they contract smoothly.
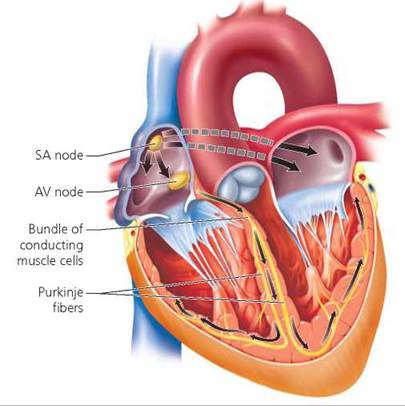
FIGURE 12.12. The conduction system of the heart consists of specialized cardiac muscle cells that speed electrical signals through the heart. The sinoatrial (SA) node serves as the heart’s internal pacemaker and determines the heart rate. Electrical signals from the SA node spread through the walls of the atria, causing them to contract. The signals then stimulate the atrioventricular (AV) node, which in turn sends the signals along the AV bundle to its forks and finally to the many Purkinje fibers that penetrate the ventricular walls. The Purkinje fibers distribute the signals to the walls of the ventricles, causing them to contract.
When the heart's conduction system is faulty, cells may begin to contract independently. Such cellular independence can result in rapid, irregular contractions of the ventricles, called ventricular fibrillation, which render the ventricles useless as pumps and stop circulation. With the brain no longer receiving the blood it needs to function, death will occur unless an effective heartbeat is restored quickly. A method for stopping ventricular fibrillation is to subject the heart to an electric shock; in many cases, the SA node will once again begin to function normally. Although costly, an implantable defibrillator (a device that electrically shocks the heart) can provide a life-saving "jump start" when needed.
Problems with the conduction system of the heart can sometimes be treated with an artificial pacemaker, a small device implanted just below the skin that monitors the heart rate and rhythm and responds to abnormalities if they occur. For instance, if the heart rate becomes too slow, the pacemaker will send an electrical stimulus to the heart through an electrode.
What would you do?
In a heart transplant operation, a person's diseased heart is replaced with a healthy heart from a person who recently died. Not surprisingly, there are thousands more people in need of a heart transplant than there are donor hearts available. Artificial hearts are available, but they are not without risk. If you were in need of a transplant, would you volunteer to participate in the testing of an artificial heart? What criteria would you use to decide?
The pace or rhythm of the heartbeat changes constantly in response to activity or excitement. The autonomic nervous system and certain hormones make the necessary adjustments so that the heart rate suits the body's needs. During times of stress, the sympathetic nervous system increases the rate and force of heart contractions. As part of this response, the adrenal medulla produces the hormone epinephrine, which can prolong the sympathetic nervous system's effects. In contrast, when restful conditions prevail, the parasympathetic nervous system dampens heart activity, in keeping with the body's more modest metabolic needs.
Electrocardiogram
The electrical events that spread through the heart with each heartbeat actually travel throughout the body, because body fluids are good conductors. Electrodes placed on the body surface can detect these electrical events, transmitting them so that they cause deflections (movements) in the tracing made by a recording device. An electrocardiogram (ECG or EKG) is an image of the electrical activities of the heart, generated by such a recording device.
A typical ECG consists of three distinguishable deflection waves, as shown in Figure 12.13. The first wave, called the P wave, accompanies the spread of the electrical signal over the atria and the atrial contraction that follows. The next wave, the QRS wave, reflects the spread of the electrical signal over the ventricles and ventricular contraction. The third wave, the T wave, represents the return of the ventricles to the electrical state that preceded contraction (ventricular repolarization). Because the pattern and timing of these waves are remarkably consistent in a healthy heart, abnormal patterns can indicate heart problems.
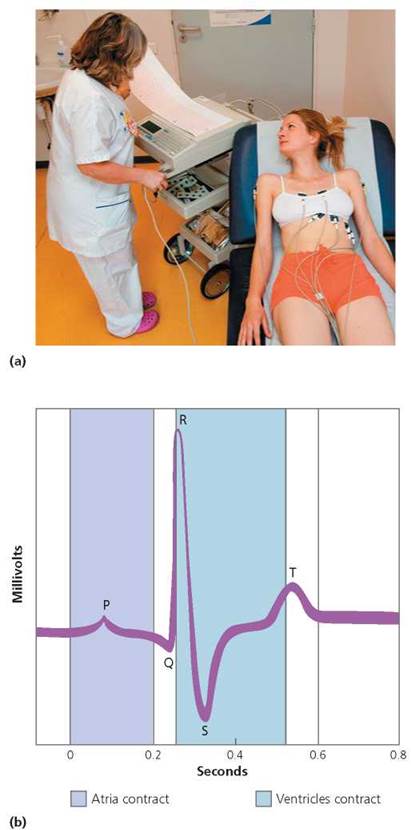
FIGURE 12.13. (a) A person having an electrocardiogram (ECG) recorded, (b) The electrical activity that accompanies each heartbeat can be visualized in an ECG tracing. The P wave is generated as the electrical signals from the SA node spread across the atria and cause them to contract. The QRS wave represents the spread of the signal through the ventricles and ventricular contraction. The T wave occurs as the ventricles recover and return to the electrical state that preceded contraction.
Blood Pressure
We hear a lot about blood pressure, usually when someone worries about having a high blood pressure reading or brags about having a low one. Blood pressure is the force exerted by the blood against the walls of the blood vessels. When the ventricles contract, they push blood into the arteries under great pressure. This pressure is the driving force that moves blood through the body, but it also pushes outward against vessel walls. Ideally, a person's blood pressure should be great enough to circulate the blood but not so great that it stresses the blood vessels and the heart, as we see in Chapter 12a. Many factors influence blood pressure, including gender, age, time of day, physical activity, stress, and lifestyle.
Blood pressure in the arteries varies predictably during each heartbeat. It is highest during the contraction of the ventricles (ventricular systole), when blood is being forced into the arteries. In a typical, healthy adult, the optimal systolic pressure, the highest pressure in the artery during each heartbeat, is 110 mm to 120 mm of mercury (mm Hg).1 Blood pressure is lowest when the ventricles are relaxing (diastole). In a healthy adult, the optimal lowest pressure, or diastolic pressure, is 70 mm to 80 mm Hg. A person's blood pressure is usually expressed as two values—the systolic followed by the diastolic. For instance, optimal adult blood pressure is said to be less than 120/80. (Do you know what your blood pressure is?)
Blood pressure is measured with a device called a sphygmomanometer (sfig-mo-mah-nom'-e-ter), which consists of an inflatable cuff that wraps around the upper arm and is attached to a device that can measure the pressure within the cuff. Figure 12.14 shows how a manually operated sphygmomanometer uses the easily measured pressure of the air pumped into the cuff to measure the blood pressure in the brachial artery (which runs along the inner surface of the arm).
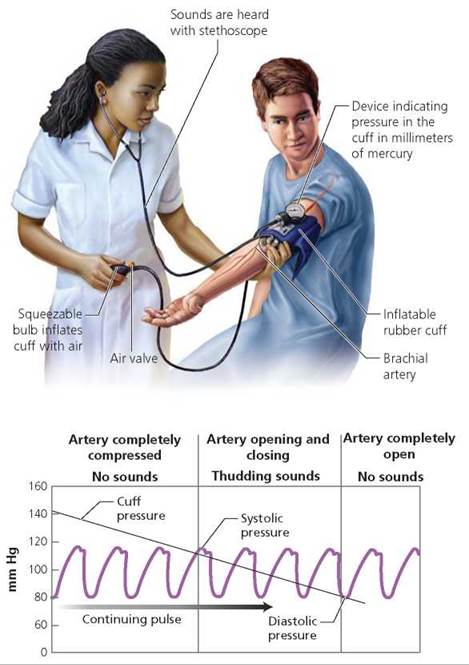
FIGURE 12.14. Blood pressure is measured with a sphygmomanometer, which consists of an inflatable cuff and a means of measuring the pressure within the cuff. The cuff is placed around the upper arm and inflated so that it compresses the brachial artery. The pressure in the cuff is slowly released, and as it descends it reaches a point where blood is able to spurt through the constricted artery only at the moments of highest blood pressure. This pressure, at which “tapping" sounds are first heard, is the systolic pressure, the blood pressure when the heart is contracting. As the pressure in the cuff continues to drop, a point is reached where the sounds disappear. The blood is now flowing continuously through the brachial artery. The pressure in the cuff when the sounds first disappear is the diastolic pressure, the blood pressure when the heart is relaxing.
Health Issue
Benefits of Cardiovascular Exercise
What would you say if you were told there is a simple way to reduce your risk of heart attack, stroke, diabetes, and cancer while controlling your weight, strengthening your bones, relieving anxiety and tension, and improving your memory? “Impossible!" you might say. “What's the catch?" There is none. This key to life is regular aerobic exercise that uses large muscle groups rhythmically and continuously and elevates heart rate and breathing rate for at least 15 to 20 minutes.
Although exercise has many beneficial effects on tire body, here we will consider only the benefits to the cardiovascular system. Exercise benefits the heart by making it a more efficient pump, thus reducing its workload. A well-exercised heart beats more slowly than the heart of a sedentary person—during both exercise and rest. The lower heart rate gives the heart more time to rest between beats. Yet at the same time, the well-exercised heart pumps more blood with each beat.
Exercise also increases the oxygen supply to the heart muscle by widening the coronary arteries, thereby increasing blood flow to the heart. Moreover, because the capillary beds within the heart muscle become more extensive with regular exercise, oxygen and nutrients can be delivered to the heart cells and wastes can be removed more quickly.
Furthermore, exercise helps to ensure continuous blood flow to the heart. One way it accomplishes this benefit is by increasing the body's ability to dissolve blood clots that can lead to heart attacks or strokes. Exercise stimulates the release of a natural enzyme that prevents blood clotting and remains effective for as long as 90 minutes after you stop exercising. Besides this, exercise stimulates the development of collateral circulation, that is, additional blood vessels that provide alternative pathways for blood flow. As a result, blood flows continuously through the heart, even if one vessel becomes blocked.
Exercise affects the blood in ways that allow more oxygen to be delivered to the cells. The amount of hemoglobin, the oxygen-binding protein in red blood cells, increases. In addition, the blood volume and the numbers of red blood cells increase.
Exercise lowers the risk of coronary artery disease by lowering blood pressure and by shifting the balance of lipids in the blood. High- density lipoproteins (HDLs), which are the “good” form of cholesterol-carrying particles that remove cholesterol from the arterial walls, increase with exercise.
To reap cardiovascular benefits, you must exercise hard enough, long enough, and often enough. The exercise must be vigorous enough to elevate your heart rate to the so-called target zone, which is between 70% and 85% of your maximal attainable heart rate. The target zone can be determined by subtracting your age in years from 222 beats per minute. The exercise must continue for at least 20 minutes and be performed at least 3 days a week, with no more than 2 days between sessions.

Questions to Consider
• Do you plan to exercise regularly? What factors will you consider in making this decision?
• Do you think that promoting exercise programs now would result in future savings in medical costs?
Doing something active on a regular basis can improve your quality of life. Moderate activity helps you feel better emotionally and physically. The difference has been likened to traveling first class instead of coach.
Lymphatic System
The lymphatic system consists of lymph, which is a fluid identical to interstitial fluid (the fluid that bathes all the cells of the body); of lymphatic vessels through which the lymph flows; and of various lymphoid tissues and organs scattered throughout the body.
The functions of the lymphatic system are as diverse as they are essential to life:
1. Return excess interstitial fluid to the bloodstream. The lymphatic system maintains blood volume by returning excess interstitial fluid to the bloodstream. Only 85% to 90% of the fluid that leaves the blood capillaries and bathes the body tissues as interstitial fluid is reabsorbed by the capillaries. The rest of that fluid (as much as 3 liters a day) is absorbed by the lymphatic system and then returned to the circulatory system. This job is important. If the surplus interstitial fluid were not drained, it would cause the tissue to swell; the volume of blood would drop to potentially fatal levels; and the blood would become too viscous (thick) for the heart to pump.
A dramatic example of the importance of returning fluid to the blood is provided by elephantiasis, a condition in which parasitic worms block lymphatic vessels (Figure 12.15). The blockage can cause a substantial buildup of fluid in the affected body region, followed by the growth of connective tissue. Elephantiasis is so named because it results in massive swelling and the darkening and thickening of the skin in the affected region, making the region resemble the skin of an elephant. Elephantiasis is a tropical disease that is transmitted by mosquitoes.

FIGURE 12.15. The leg of a person with elephantiasis. In this condition, parasitic worms plug lymphatic vessels and prevent the return of fluid from the tissues to the circulatory system.
2. Transport products of fat digestion from the small intestine to the bloodstream. The products of fat digestion are too large to be absorbed into the capillaries in the small intestine. Instead, these products enter a lymphatic vessel, called a lacteal, and travel in the lymphatic system to be returned to the blood circulatory system.
3. Help defend against disease-causing organisms. The lymphatic system helps protect against disease and cancer. We will learn more about its role in body defense in Chapter 13.
The structure of the lymphatic vessels is central to their ability to absorb the interstitial fluid not carried away by capillaries. The extra fluid enters a branching network of microscopic tubules, called lymphatic capillaries, that penetrate between the cells and the capillaries in almost every tissue of the body (except teeth, bones, bone marrow, and the central nervous system; Figure 12.16). The lymphatic capillaries differ from the blood capillaries in two ways. First, unlike blood capillaries, which form continuous networks, lymphatic capillaries end blindly, like the fingers of a glove. In essence, lymphatic capillaries serve as drainage tubes. Fluid enters at the "fingertips" and moves through the system in only one direction. Second, lymphatic capillaries are much more permeable than blood capillaries, a feature that is crucial to their ability to absorb the digestive products of fats as well as excess interstitial fluid. The lymphatic capillaries drain into larger lymphatic vessels, which merge into progressively larger tubes with thicker walls. Lymph is eventually returned to the blood through one of two large ducts that join with the large veins at the base of the neck.
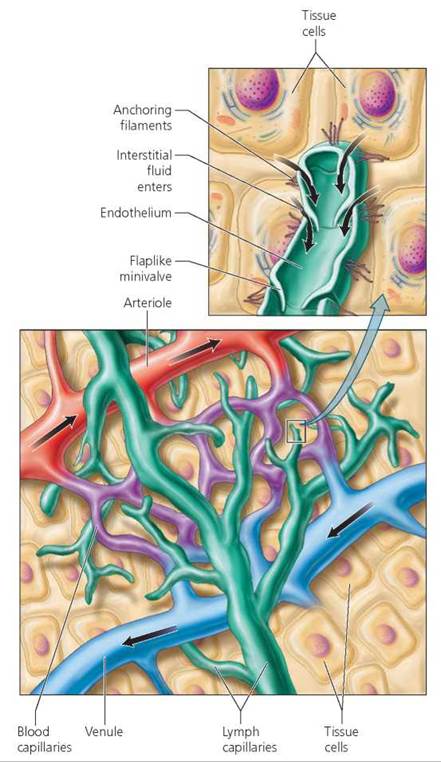
FIGURE 12.16. The lymphatic capillaries are microscopic, blind-ended tubules through which surplus tissue fluid enters the lymphatic system to be returned to the bloodstream.
With no pump to drive it, lymph flows slowly through the lymphatic vessels, propelled by the same forces that move blood through the veins. That is, the contractions of nearby skeletal muscles compress the lymphatic vessels, pushing the lymph along. One-way valves similar to those in veins prevent backflow. And as with the flow of blood back to the heart from the lower part of the body, pressure changes in the thorax (chest cavity) that accompany breathing also help pull the lymph upward from the lower body. Gravity assists the flow from the upper body.
The lymphatic vessels are studded with lymph nodes, small bean-shaped structures that cleanse the lymph as it slowly filters through. The lymph nodes contain macrophages and lymphocytes, white blood cells that play an essential role in the body's defense system. Macrophages engulf bacteria, cancer cells, and other debris, clearing them from the lymph. Lymphocytes serve as the surveillance squad of the immune system. They are continuously on the lookout for specific disease-causing invaders, as we will see in Chapter 13. When lymphocytes detect bacteria or viruses, the lymphocytes are stimulated to divide. The increased number of lymphocytes causes the lymph nodes to swell. Thus, swollen and painful lymph nodes (commonly called "glands") are a symptom of infection.
Besides the lymph nodes, there are several other lymphoid organs (Figure 12.17). Among these are the tonsils, which form a ring around the entrance to the throat, where they help protect against disease organisms that are inhaled or swallowed. The thymus gland, located in the chest, is another lymphoid organ. It plays its part during early childhood by helping the maturation of certain lymphocytes that protect us from specific disease-causing organisms. On the left side of the abdominal region is the largest lymphoid organ, the spleen. Besides containing a reservoir of lymphocytes, the spleen clears the blood of old and damaged red blood cells and platelets. Finally, isolated clusters of lymph nodules along the small intestine, known as Peyer's patches, keep bacteria from breaching the intestinal wall. The red bone marrow, where white blood cells and other formed elements are produced, is a lymphoid organ found in the ends of long bones, ribs, sternum, and vertebrae.
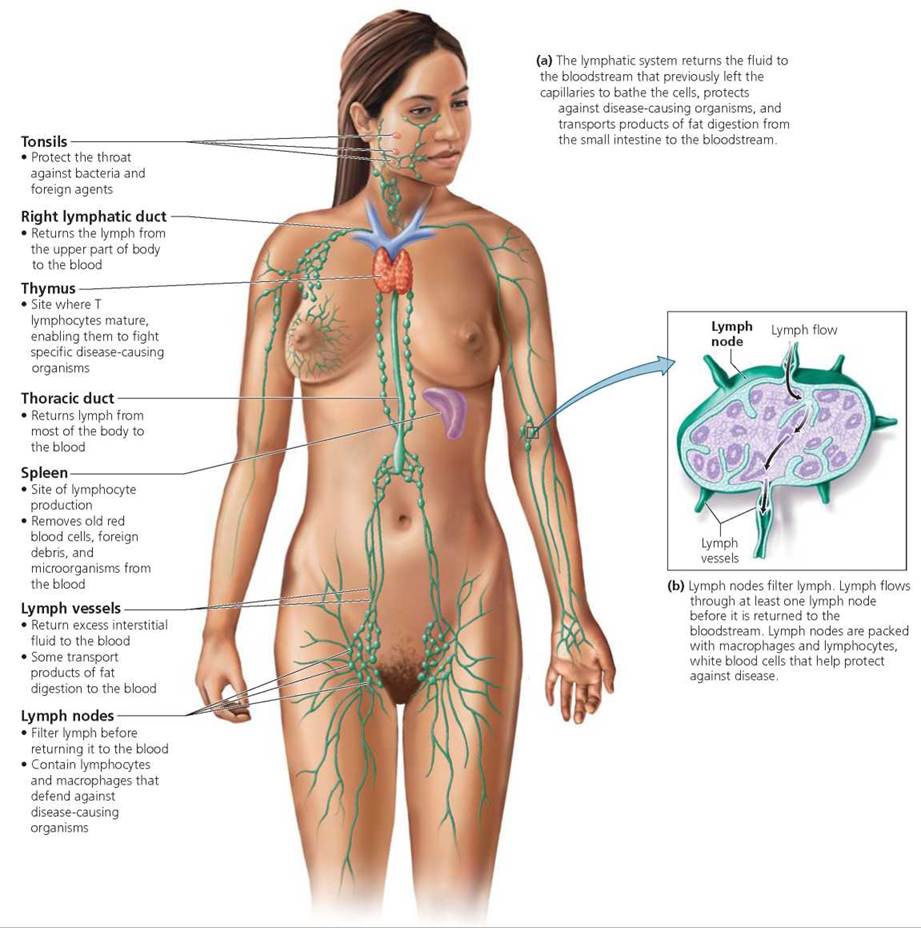
FIGURE 12.17. The lymphatic system is a system of lymphatic vessels containing a clear fluid, called lymph, and various lymphatic tissues and organs located throughout the body. Green indicates lymphatic vessels and nodes.
Stop and think
Cancer cells that break loose from their original site in a process called metastasis have easy access to the highly permeable lymphatic capillaries. The lymphatic vessels then provide a route by which the cancer cells may spread to nearly every part of the body. Why are the lymph nodes often examined to determine whether cancer has spread? Why are the lymph nodes near the original cancer site often removed?
Looking ahead
In this chapter, we learned about the structure and function of the cardiovascular and lymphatic systems as they are in a healthy person. In the next chapter, we will consider some common disorders of the cardiovascular system.
_______________________________________________________
1 Pressure is measured as the height to which that pressure could push a column of mercury (Hg).
Highlighting the Concepts
Cardiovascular System (pp. 214-215)
• The heart serves as a pump that pushes blood through blood vessels.
Blood Vessels (pp. 216-220)
• Blood circulates through a branching network of blood vessels in a path that travels from the heart to arteries to arterioles to capillaries to venules to veins and then back to the heart.
• Arteries are elastic, muscular tubes that carry blood away from the heart. By stretching and then returning to their original shape, they withstand the high pressure of blood as it is pumped from the heart. These changes help maintain a relatively even blood pressure within the arteries despite large changes in the volume of blood within them.
• The pressure change along an artery as it expands and returns to its original size is called a pulse.
• Arteries branch to form narrower tubules called arterioles. Arterioles are important in the regulation of blood pressure, and they regulate blood flow through capillary beds.
• The exchange of materials between the blood and tissues takes place across the thin walls of capillaries. Capillaries are arranged in highly branched networks that provide a tremendous surface area for the exchange. Each network of capillaries is called a capillary bed. Rings of muscle called precapillary sphincters determine whether blood flows into a capillary bed or is channeled through it.
• Capillaries merge to form venules; and these, in turn, merge to form veins, which conduct blood back to the heart. Blood is returned to the heart against gravity by nearby skeletal muscles that contract and push the blood along within the veins. Valves within the veins prevent blood from flowing backward when the skeletal muscles are relaxed. Pressure differences generated by breathing also help draw blood toward the heart from the lower torso.
Heart (pp. 220-225)
• Every minute, the heart beats about 72 times and moves slightly less than 5 liters (10 pt) of blood through its chambers.
• Most of the wall of the heart is composed of cardiac muscle and is called the myocardium. The endocardium is a thin inner lining. The heart is enclosed in a fibrous sac called the pericardium, which allows the heart to beat while still confining it near the midline of the thoracic cavity.
• The right and left halves of the heart function as two separate pumps. Each side consists of two chambers: an upper chamber called the atrium and a lower chamber called the ventricle. The smaller, thin-walled atria function primarily as receiving chambers that accept blood returning to the heart and pump it a short distance to the ventricles. When the larger, thick-walled ventricles contract, they push blood through the arteries to all parts of the body.
• Blood circulates in one direction through the heart due to the action of two pairs of valves. The atrioventricular (AV) valves are located between each atrium and ventricle. The semilunar valves are located between each ventricle and its connecting artery. The heart sounds, lub-dup, are caused by blood turbulence associated with the closing of the heart valves.
• The right side of the heart pumps blood to the lungs through a loop of vessels called the pulmonary circuit. The left side of the heart pumps blood to all parts of the body except the lungs through a loop of vessels called the systemic circuit.
• The heart has its own network of vessels, called the coronary circuit, that services the heart tissue itself.
• Each heartbeat consists of contraction (systole) and relaxation (diastole). The atria contract in unison, and then the ventricles do the same. The events associated with each heartbeat are collectively called the cardiac cycle.
• The rhythmic contraction of the heart is produced by its internal conduction system. A cluster of specialized cardiac muscle cells, called the sinoatrial (SA) node, usually sets the tempo of the heartbeat and is therefore called the pacemaker. When the electrical signal reaches another cluster of specialized muscle cells, called the atrioventricular (AV) node, the stimulus is quickly relayed along the atrioventricular bundle that runs through the wall between the two ventricles and then fans out into the ventricular walls through the Purkinje fibers.
• The rate of heartbeat changes constantly to suit the body's level of activity.
• An electrocardiogram (ECG or EKG) is a recording of the electrical events associated with each heartbeat.
Blood Pressure (pp. 225-227)
• Blood pressure, the force created by the heart to drive the blood around the body, is measured as the force of blood against the walls of blood vessels. The blood pressure in an artery peaks when a ventricle contracts. This is called the systolic pressure. In contrast, the lowest blood pressure of each cardiac cycle, the diastolic pressure, occurs while the heart is relaxing between contractions. Blood pressure is measured with a device called a sphygmomanometer.
Lymphatic System (pp. 227-230)
• The lymphatic system consists of lymph, lymphatic vessels, lymphoid tissue, and lymphoid organs.
• Three vital functions of the lymphatic system are to return interstitial fluid to the bloodstream, to transport products of fat digestion from the digestive system to the bloodstream, and to defend the body against disease-causing organisms or abnormal cells.
• Tissue fluid enters lymphatic capillaries—microscopic tubules that end blindly and are more permeable than blood capillaries. The fluid, then called lymph, is moved along larger lymphatic vessels by contraction of nearby skeletal muscles. The lymphatic vessels have valves to prevent the backflow of lymph.
• Lymph nodes filter lymph and contain cells that actively defend against disease-causing organisms.
• Lymphoid organs include the red bone marrow, lymph nodes, tonsils, thymus gland, spleen, and Peyer's patches of the small intestine.
Reviewing the Concepts
1. Trace the flow of blood from the heart and back to it by naming, in order, the general types of vessels through which the blood flows. p. 216
2. What is a pulse? p. 216
3. What is an aneurysm? Why is it dangerous? p. 216
4. What are two important functions of arterioles? p. 216
5. What determines whether blood flows through any particular capillary bed? p. 218
6. Compare the structure of arteries, capillaries, and veins. Explain how the structure is suited to the function of each type of vessel. pp. 216-231
7. Explain how blood is returned to the heart from the lower torso against the force of gravity. p. 219
8. Describe the structure of the heart valves. Explain how they function. pp. 216-219
9. Describe the structure of the heart. Explain how it functions as two separate pumps. p. 220
10. Trace the path of blood from the left ventricle to the left atrium, naming each major vessel associated with the heart and the heart chambers in the correct sequence. p. 222
11. Describe the cardiac cycle. pp. 223-224
12. Explain how clusters or bundles of specialized cardiac muscle cells coordinate the contraction associated with each heartbeat. pp. 224-225
13. List three important functions of the lymphatic system. p. 227
14. Compare the structure of lymphatic capillaries with the structure of blood capillaries. How does the structure of lymphatic capillaries allow them to absorb tissue fluid? p. 228
15. What is the function of lymph nodes? p. 228
16. The semilunar valves prevent the backflow of blood from the
a. arteries to the ventricles.
b. veins to the atria.
c. ventricles to the atria.
d. arteries to the atria.
17. If you cut all the nerves to the heart but kept the heart alive,
a. the heart would stop beating.
b. the heart would continue beating.
c. only systole would occur.
d. only diastole would occur.
For questions 18 and 19, imagine that you have been miniaturized and are riding through the circulatory system using a red blood cell as a life raft.
18. You are in the big toe traveling toward the heart. The last vessel you pass through before entering the heart is the
a. aorta.
b. inferior vena cava.
c. coronary artery.
d. pulmonary vein.
19. You are nearly deafened by the first heart sound, which is caused by
a. the opening of the atrioventricular valves.
b. the closing of the atrioventricular valves.
c. the opening of the semilunar valves.
d. the closing of the semilunar valves.
20. The _____ is a cluster of specialized heart muscle cells that determines the heart rate by initiating each cardiac cycle.
21. A weakened area on an artery wall that can balloon outward is called _____.
22. Oxygen and nutrients move through the walls of _____ to reach the body cells.
Applying the Concepts
1. Abnormally short (or long) chordae tendineae of the mitral (bicuspid) valve can cause a condition known as mitral valve prolapse, in which the mitral valves do not close properly. Why would mitral valve prolapse cause the heart to produce abnormal heart sounds?
2. Nicotine in cigarette smoke causes vasoconstriction (narrowing of certain blood vessels) and increases heart rate. Explain how these effects lead to high blood pressure. Explain why cigarette smokers are more likely to die of cardiovascular diseases than are nonsmokers.
3. Amelia is a friend of yours. When you call her to ask about dinner plans, she tells you that she is not feeling well. She aches all over and has swollen "glands" in her neck. You explain that these are not really glands, because they do not secrete anything. What are they? Why are they swollen?
Becoming Information Literate
Use at least three reliable sources (books, journals, websites) to plan a program for yourself to increase your cardiovascular fitness. Begin by deciding which aspects of your lifestyle you might change to improve cardiovascular fitness. Examples might include but are not limited to weight loss, change in diet, increased physical activity, and stress reduction. Next, plan a logical progression of changes that considers the type of activities and the foods that you enjoy. List each source you considered, and explain why you chose the three sources you used.