Biology of Humans
15. The Digestive System
In the previous chapter, we learned how we obtain oxygen and rid our bodies of carbon dioxide. In this chapter, we learn how we obtain necessary nutrients from the food we eat. We learn that food usually travels in one direction through the digestive system. We see how the digestive system is organized for breaking down food molecules and making them available for use as a source of energy or as raw material for the growth and repair of cells. Food is digested and nutrients and water are absorbed in specialized compartments along a long tube, the GI tract. Undigested materials are then eliminated from the body.
The Gastrointestinal Tract
There is some truth to the saying, "You are what you eat." Rest assured, however, that no matter how many hamburgers you eat, you will never become one. Instead, the hamburger becomes you. This transformation is largely due to the activities of the digestive system. Like an assembly line in reverse, the digestive system takes the food we eat and breaks the complex organic molecules into their chemical subunits. The subunits are molecules small enough to be absorbed into the bloodstream and delivered to body cells, where they either provide fuel for growth and repair of the body or they provide energy for daily activities. Imagine that you just ate a cheeseburger on a bun. The starch in the bun may fuel a jump for joy; the protein in the beef may be used to build muscle; and the fat in the cheese may become myelin sheaths that insulate nerve fibers. The digestive system breaks food into molecules small enough to be absorbed and delivered to the cells that use them. Table 15.1 identifies the structures of the digestive system and describes their roles in both mechanical and chemical digestion. You can refer to the table as you read about each of the following digestive structures.
· The digestive system breaks food into its component subunits that are small enough to absorb. The subunits are then used for energy or as building blocks to make new molecules.
TABLE 15.1. Review of Structures of the Digestive System
Structure |
Description/Functions |
Mechanical Digestion |
Chemical Digestion |
Mouth |
Receives food; contains teeth and tongue; tongue manipulates food and monitors quality |
Teeth tear and crush food into smaller pieces |
Digestion of carbohydrates begins |
Pharynx |
Area that both food and air pass through |
None |
None |
Esophagus |
Tube that transports food from mouth to stomach |
None |
None |
Stomach |
J-shaped muscular sac for food storage |
Churning of stomach mixes food with gastric juice, creating liquid chyme |
Protein digestion begins |
Small intestine |
Long tube where digestion is completed and nutrients are absorbed |
Segmental contractions mix food with intestinal enzymes, pancreatic enzymes, and bile |
Carbohydrate, protein, and fat digestion completed |
Large intestine |
Final tubular region of GI tract; absorbs water and ions; houses bacteria; forms and expels feces |
None |
Some digestion is carried out by bacteria |
Anus |
Terminal outlet of digestive tract |
None |
None |
The digestive system consists of a long, hollow tube, called the gastrointestinal (GI) tract, into which various accessory glands release their secretions (Figure 15.1). The GI tract begins at the mouth and continues to the esophagus, stomach, small intestine, and large intestine. The hollow area of the tube through which food and fluids travel is called the lumen. Along most of its length, the walls of the GI tract have four basic layers.
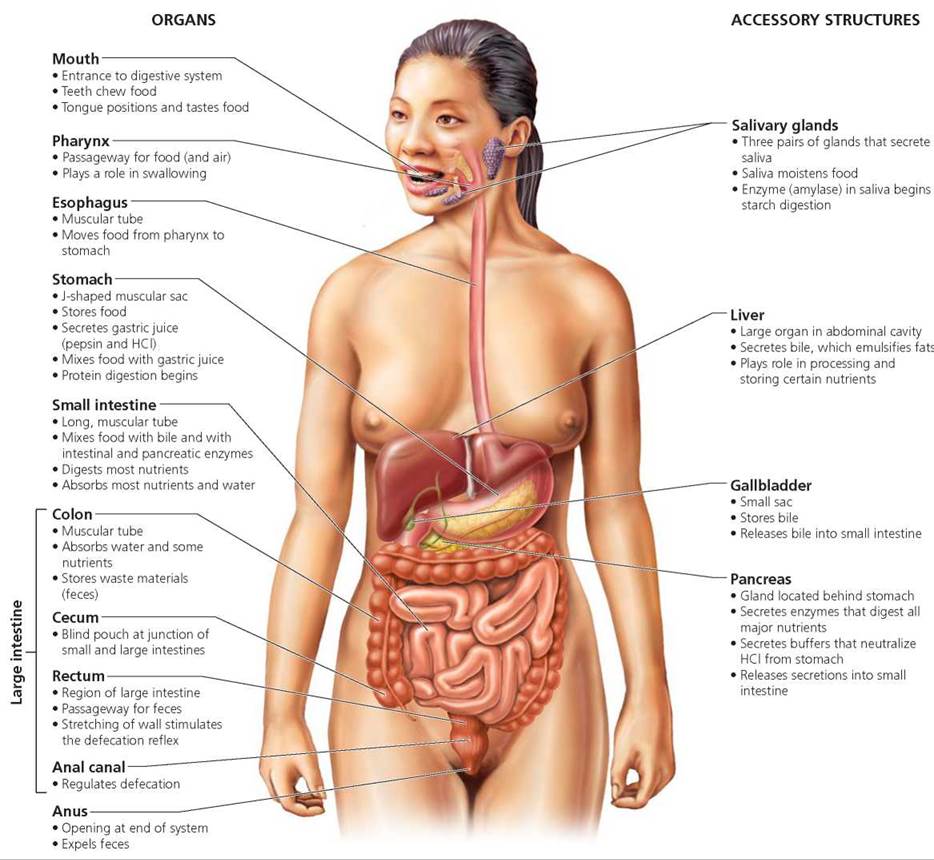
FIGURE 15.1. The digestive system consists of a long tube, called the gastrointestinal tract, into which accessory structures release their secretions.
• Mucosa. The innermost layer of the GI tract is the moist, mucus-secreting layer called the mucosa. The mucus helps lubricate the lumen, allowing food to slide through easily. Mucus also helps protect the cells in the lining of the GI tract from rough substances in the food and from digestive enzymes. In some regions of the digestive system, cells in the mucosa also secrete digestive enzymes. In addition, the mucosa in some parts of the digestive tract is highly folded, which increases the surface area for absorption.
• Submucosa. The next layer, the submucosa, consists of connective tissue containing blood vessels, lymph vessels, and nerves. The blood supply maintains the cells of the digestive system and, in some regions, picks up and transports the products of digestion. The nerves are important in coordinating the contractions of the next layer.
• Muscularis. The next layer, the muscularis, is responsible for movement of materials through the GI tract and for mixing ingested materials with digestive secretions. In most sections of the GI tract, the muscularis is a double layer of smooth muscle. (The stomach, as you will read later, is an exception; it has three layers of muscle.) In the inner, "circular" layer of muscle, the muscle cells encircle the tube, causing a constriction when they contract. In the outer, longitudinal layer, the muscle cells are arranged parallel to the GI tract. Longitudinal muscles shorten the GI tract when they contract. The muscle layers churn the food until it is liquefied, mix the resulting liquid with enzymes, and propel the food along the GI tract in a process called peristalsis, which is discussed later in this chapter. Local muscle contractions in random regions of the GI tract, especially in the small intestine, are called segmental contractions. Segmental contractions mix intestinal contents—food and digestive juices (fluids containing enzymes and other fluids that aid in digestion). Segmental contractions also assist absorption of digested food by moving intestinal contents over the intestinal wall.
• Serosa. The serosa, a thin layer of epithelial tissue supported by connective tissue, wraps around the GI tract. It secretes a fluid that lubricates the outside of the GI tract to reduce friction with contacting surfaces of the intestine and other abdominal organs (Figure 15.2 on page 288). Regions of the GI tract are specialized to process food in particular ways. One aspect of that processing is mechanical digestion, the physical breaking of food into smaller pieces, and another is chemical digestion, the breaking of chemical bonds so that complex molecules are taken apart into smaller subunits. Chemical digestion produces molecules that can be absorbed into the bloodstream and used by the cells. Next we trace the path food travels along the GI tract to see how it is processed and absorbed.
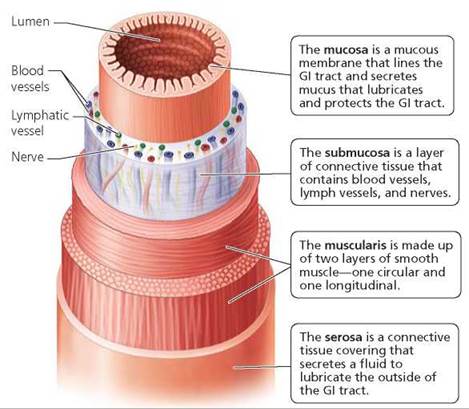
FIGURE 15.2. Along most of its length, the wall of the GI tract has four basic layers: the mucosa, the submucosa, the muscularis, and the serosa.
Specialized Compartments for Food Processing
As food moves along the GI tract, it passes through the mouth, pharynx, esophagus, stomach, small intestine, and large intestine. The salivary glands, liver, and pancreas add secretions along the way. Most nutrients are absorbed from the small intestine. Additional water is absorbed in the large intestine. Undigested and indigestible materials pass out the anus.
Mouth
The entryway to the digestive system and the first stop on food's journey through it is the mouth, also called the oral cavity. The roof of the mouth is called the palate. The region of the palate closest to the front of the mouth, the hard palate, is reinforced with bone. Toward the back of the mouth is the soft palate, which consists only of muscle and prevents food from entering the nose during swallowing. The mouth serves several functions: (1) it begins mechanical and, to some extent, chemical digestion; (2) it monitors food quality; and (3) it moistens and manipulates food so that it can be swallowed. The teeth, salivary glands, and tongue all contribute to these functions.
Teeth and mechanical digestion. As we chew, our teeth break solid foods into smaller fragments that are easier to swallow and digest. The sharp, chisel-like incisors in the front of the mouth (see Figure 15.3a) slice the food as we bite into it. At the same time, the pointed canines to the sides of the incisors tear the food. Then the food is ground, crushed, and pulverized by the premolars and molars, which lie along the sides of the mouth.
Teeth are alive. In the center of each tooth is the pulp, which contains the tooth's life-support systems—blood vessels that nourish the tooth and nerves that sense heat, cold, pressure, and pain (Figure 15.3b). Surrounding the pulp is a hard, bonelike substance, called dentin. The crown of the tooth (the part visible above the gum line) is covered with enamel, a nonliving material that is hardened with calcium salts. The root of the tooth (the part below the gum line) is covered with a calcified, yet living and sensitive connective tissue called cemen- tum. The roots of the teeth fit into sockets in the jawbone. Blood vessels and nerves reach the pulp through a tiny tunnel through the root, called the root canal.
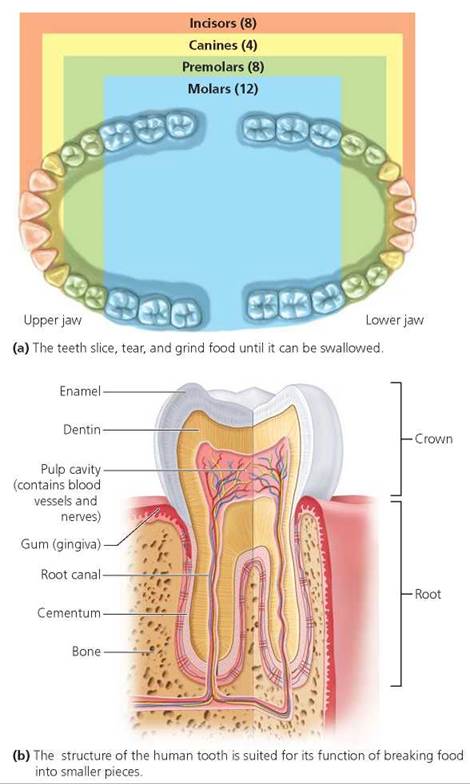
FIGURE 15.3. Adult human teeth
Tooth decay is caused by acid produced by bacteria living in the mouth. When you eat, food particles become trapped between the teeth, in the small spaces where the teeth meet the gums, and in the hollows of molars. Bacteria in the mouth are nourished by the sugar in these food particles. As bacteria digest the sugar, acid is produced that erodes the enamel and causes a cavity to form. Blood vessels in the pulp widen in response to this erosion, allowing greater numbers of white bloods cells to reach the area and fight infection. The widened blood vessels may press on nerves, causing a toothache. When the enamel has been penetrated, bacteria can invade the softer dentin beneath. If a dentist does not fill the cavity, the bacteria can infect the pulp. Plaque, an invisible film of bacteria, mucus, and food particles, promotes tooth decay because it holds the acid against the enamel. Daily brushing and flossing helps remove plaque, reducing the chance of tooth decay.
Gum disease, which affects two of three middle-aged people in the United States, is a major cause of tooth loss in adults. Gingivitis (gingiv-, the gums; -itis, inflammation of), an early stage of gum disease, occurs when plaque that has formed along the gum line causes the gums to become inflamed and swollen. The swollen gums can bleed and do not fit as tightly around the teeth as they should. The pocket that forms between the tooth and the gum traps additional plaque. The bacteria in the plaque can then attack the bone and soft tissues around the tooth, a condition called periodontitis (peri-, around; dont, teeth; -itis, inflammation of). As the tooth's bony socket and the tissues that hold the tooth in place are eroded, the tooth becomes loose.
What would you do?
For the past 50 years, some communities whose water is not naturally fluoridated have added low doses of fluoride to the public water supply to reduce tooth decay. Nearly 98% of Americans have, or have had, tooth decay. Over 6 million teeth are removed each year. Proponents of fluoridation point out that the incidence of tooth decay has declined after the addition of fluoride to drinking water. Opponents of the practice argue that (1) fluoridation of the water supply is a form of forced medication; (2) the dosage cannot be properly controlled because of differences in people's body weight and the amount of water people consume; and (3) excessive fluoride intake causes teeth to become brown and mottled. If you had to vote on fluoridation of your public water supply, what additional information would you want before voting? How would you vote at present?
Salivary glands and chemical digestion. Three pairs of salivary glands—the sublingual (below the tongue), submandibular (below the jaw), and parotid (in front of the ears)—release their secretions, collectively called saliva, into the mouth (Figure 15.4). As we chew, food is mixed with saliva. Water in saliva moistens food, and mucus binds food particles together, making it easier for the food to pass through the GI tract.
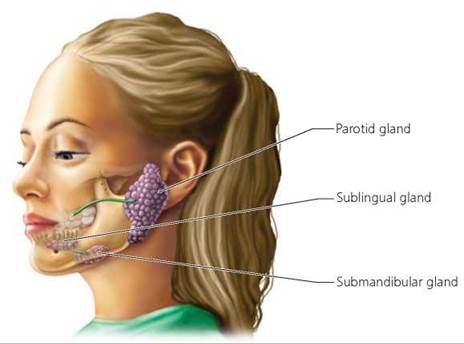
FIGURE 15.4. Three pairs of salivary glands release their secretions into the mouth. These secretions, collectively called saliva, make food easier to swallow, dissolve substances so they can be tasted, and begin the chemical digestion of starch.
Saliva also contains an enzyme, called salivary amylase, that begins to chemically digest starches into shorter chains of sugar. You will notice the result of salivary amylase activity if you chew a piece of bread for several minutes: The bread will begin to taste sweet. Try it.
Tongue: Taste and food manipulation The tongue is a large skeletal muscle studded with taste buds. Our ability to control the position and movement of the tongue is critical to both speech and the manipulation of food within the mouth. Once food molecules are dissolved in saliva, the chemicals in the food can stimulate receptors in taste buds located primarily on the tongue. Information from the taste buds, along with input from the olfactory receptors in the nose, helps us to monitor the quality of food. For instance, spoiled or poisonous food usually tastes and smells bad, so we can spit it out before swallowing. The tongue moves food to position it for crushing and grinding by the teeth, to mix it with saliva, and to shape it into a small, soft mass, called a bolus, that is easily swallowed. The tongue also initiates swallowing by pushing the bolus to the back of the mouth.
Pharynx
The pharynx, which is the passageway commonly called the throat, is shared by the respiratory and digestive systems. When we swallow, food is pushed from the mouth, through the pharynx, and into the esophagus, the tube that connects the pharynx to the stomach.
Swallowing consists of a voluntary component followed by an involuntary one. When a person begins to swallow, the tongue pushes the bolus of softened and moistened food into the pharynx (Figure 15.5). Once food is in the pharynx, it is too late to change one's mind about swallowing. Sensory receptors in the wall of the pharynx detect the presence of food and stimulate the involuntary swallowing reflex. Reflex movements of the soft palate prevent food from entering the nasal cavities. Other involuntary muscle contractions push the larynx (the voice box, commonly called the Adam's apple) upward. As we learned in Chapter 14, the movement of the larynx causes a cartilaginous flap called the epiglottis to move, covering the opening to the airways of the respiratory system (the glottis). The movement of the epiglottis prevents food from entering the airways. Instead, food is pushed into the esophagus.
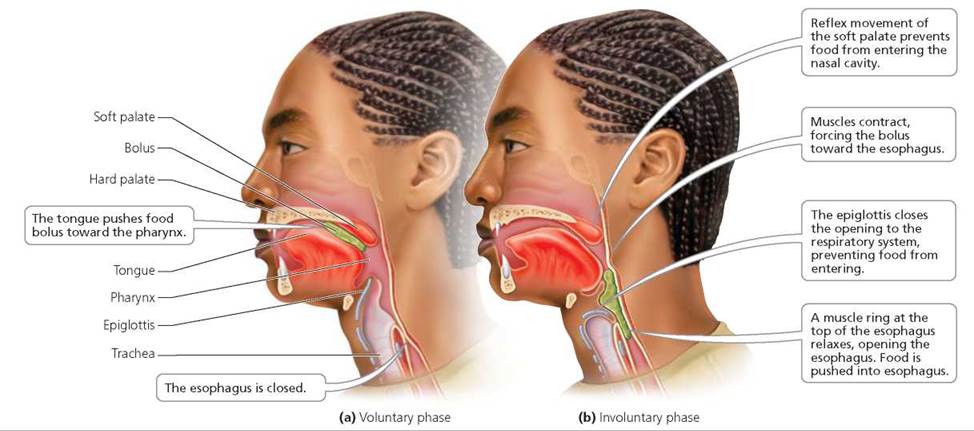
FIGURE 15.5. Swallowing consists of (a) voluntary and (b) involuntary phases.
Esophagus
The esophagus is a muscular tube that conducts food from the pharynx to the stomach. Food is moved along the esophagus and all the rest of the GI tract by rhythmic waves of muscle contraction called peristalsis. In the esophagus, small intestine, and large intestine, peristalsis is produced by the two layers of muscle in the muscularis. The muscles of the inner layer circle the tube, causing a constriction when they contract. The muscles in the outer layer run lengthwise, causing a shortening of the region where they contract. The presence of food stretches the walls in one region of the tube, and this triggers the contraction of circular muscles in the region of the tube immediately behind the food mass. When these circular muscles contract, that region of the tube pinches inward, pushing food forward. The food then stretches the next adjacent region of the tube, again stimulating contraction of circular muscles behind it. At the same time, longitudinal muscles in front of the food contract, shortening this region and widening its walls to receive the food. We see, then, that gravity is not important in moving food along the digestive tract. It is possible, therefore, to swallow while standing on your head or in the weightless conditions of outer space (Figure 15.6).
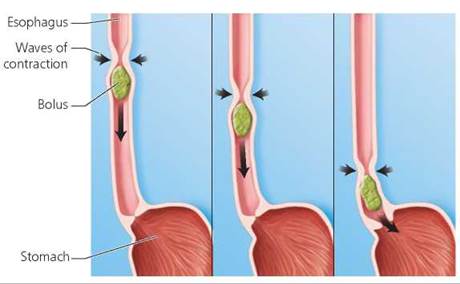
FIGURE 15.6. Peristalsis is a wave of muscle contraction that pushes food along the esophagus and the entire remaining GI tract. When circular muscles contract, the tube is narrowed and food is pushed forward. The longitudinal muscles in front of the bolus contract, shortening that region.
Stomach
The stomach is a muscular sac that is well designed to carry out its three important functions: (1) storing food and regulating the release of food to the small intestine, (2) liquefying food, and (3) carrying out the initial chemical digestion of proteins. The structure of the stomach is shown in Figure 15.7.
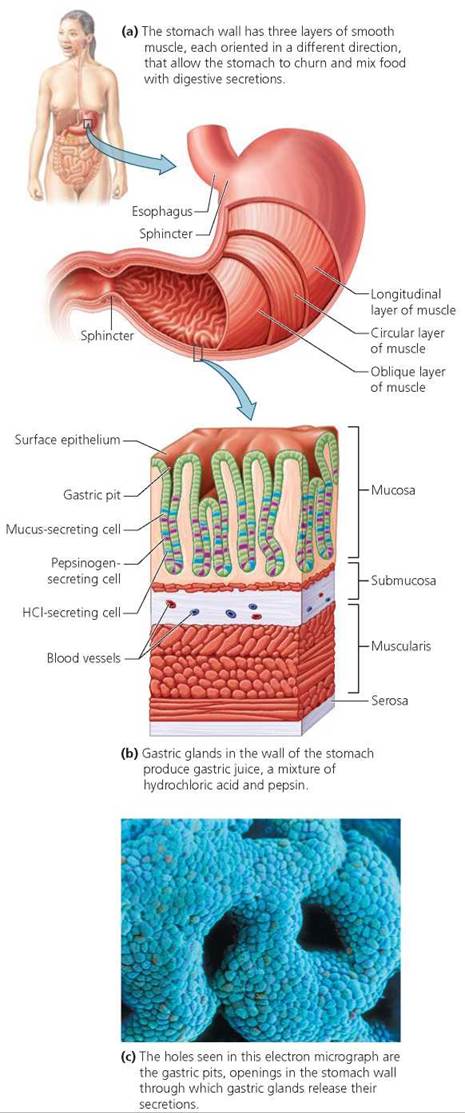
FIGURE 15.7. The structure of the stomach is well suited to its functions of churning food with digestive secretions, storing food, and beginning protein digestion.
Storage of food and regulation of the release of food to the small intestine Like any good storage compartment, the stomach is expandable and has openings that can close to seal the contents within as well as open for filling and emptying. When empty, the stomach is a small, J-shaped sac that can hold only about 50 ml (a quarter of a cup) without stretching. However, the wall of the empty stomach has folds that can spread out, allowing the stomach to expand as it fills. When fully expanded, as after a large meal, the stomach can hold several liters of food. Bands of circular muscle called sphincters guard the openings at each end of the stomach and regulate the release of food to the small intestine. Contraction of a sphincter closes the opening, and relaxation of a sphincter allows material to pass through.
Heartburn occurs when the pressure of the stomach contents overwhelms the sphincter at the lower end of the esophagus, causing a burning sensation behind the breastbone. In some people, this sphincter is weak and unable to keep stomach contents out of the esophagus. A person with a normal esophageal sphincter will experience heartburn when the stomach contents exert a greater pressure than usual against the sphincter, as might occur after a large meal, during pregnancy, when lying down, or when constipated.
People who have chronic heartburn—at least one attack per week—have an increased risk of developing cancer of the esophagus. The risk increases with the frequency of attacks and the number of years of experiencing heartburn. Those who have one attack per week have a risk eight times higher than normal. Esophageal cancer is particularly aggressive and has become more common in recent years. It is detected using a test called endoscopy, in which a thin, lighted tube is snaked down the throat. A more recently developed means of detecting potentially harmful changes in the esophagus is the PillCam. The patient swallows a camera that is about the size of a vitamin pill. As the camera moves through the esophagus, it takes thousands of pictures and sends them to a small recording device worn by the patient.
Liquefaction of food. Food is generally stored and processed within the stomach for 2 to 6 hours. The stomach wall has three layers of smooth muscle, each oriented in a different direction. The coordinated contractions of these layers twist, knead, and compress the stomach contents, physically breaking food into smaller pieces. This additional mechanical digestion occurs as the food is churned and mixed with secretions produced by the glands of the stomach until it is a soupy mixture called chyme.
Initial chemical digestion of proteins. Chemical digestion in the stomach is limited to the initial breakdown of proteins. The lining of the stomach has millions of gastric pits, within which are gastric glands containing several types of secretory cells. Certain secretory cells produce hydrochloric acid (HCl), which kills most of the bacteria swallowed with food or drink. Hydrochloric acid also breaks down the connective tissue of meat and activates pepsinogen, which is secreted by other cells in the gastric glands. Once activated by HCl, pepsinogen becomes pepsin, a protein-digesting enzyme. When the mixture of pepsin and HCl, called gastric juice, is released into the stomach, the pepsin begins the chemical digestion of the protein in food. Still other cells within the gastric glands secrete mucus, which helps protect the stomach wall from the action of gastric juice. Although not related to the digestive function of the stomach, a very important material secreted by the gastric glands is intrinsic factor, a protein necessary for the absorption of vitamin B12 from the small intestine. The stomach wall is composed of the same materials that gastric juice is able to attack, so various protections are in place to keep the stomach from digesting itself. One, mentioned previously, is the presence of mucus. Mucus forms a thick, protective coat that prevents gastric juice from reaching the cells of the stomach wall. The alkalinity of mucus helps to neutralize the HCl. Another protection is that pepsin is produced in an inactive form (pepsinogen) that cannot digest the cells that produce it. In addition, neural and hormonal reflexes regulate the production of gastric juice so that little is released unless food is present to absorb and dilute it. Finally, if the stomach lining is damaged, it is quickly repaired. The high rate of cell division in the stomach lining replaces a half million cells every minute. As a result, you have a new stomach lining every 3 days!
Very little absorption of food and other ingested materials occurs in the stomach because food simply has not been broken down into molecules small enough to be absorbed. Notable exceptions are alcohol and aspirin. The absorption of alcohol from the stomach is the reason its effects can be felt very quickly, especially if there is no food present to dilute it. The absorption of aspirin can cause bleeding of the wall of the stomach, which is the reason aspirin should be avoided by people who have stomach ulcers (see the Health Issue essay, Peptic Ulcers).
Small Intestine
The next region of the digestive tract, the small intestine, has two major functions: chemical digestion and absorption. As food moves along this twisted tube, it passes through three specialized regions: the duodenum, the jejunum, and the ileum. Chyme from the stomach enters the duodenum, the first region of the small intestine, in squirts, so that only a small amount enters the small intestine at one time. Digestive juices also enter the duodenum from the pancreas and liver. However, most chemical digestion and absorption occur in the jejunum and the ileum.
Chemical digestion within the small intestine. Within the small intestine, a battery of enzymes completes the chemical digestion of virtually all the carbohydrates, proteins, fats, and nucleic acids in food. Although both the small intestine and the pancreas contribute enzymes, most of the digestion that occurs in the small intestine is actually performed by pancreatic enzymes (Table 15.2).
TABLE 15.2. Major Digestive Enzymes
Enzyme |
Site of Production |
Site of Action |
Substrate and Products |
Carbohydrate digestion |
|||
Salivary amylase |
Mouth Salivary glands |
Mouth |
Polysaccharides into shorter molecules |
Amylase |
Pancreas |
Small intestine |
Polysaccharides into disaccharides |
Maltase |
Small intestine |
Small intestine |
Maltose into glucose units |
Sucrase |
Small intestine |
Small intestine |
Sucrose into glucose and fructose |
Lactase |
Small intestine |
Small intestine |
Lactose into glucose and galactose |
Protein digestion |
|||
Pepsin |
Stomach |
Stomach |
Proteins into protein fragments (polypeptides) |
Trypsin |
Pancreas |
Small intestine |
Proteins and polypeptides into smaller fragments |
Chymotrypsin |
Pancreas |
Small intestine |
Proteins and polypeptides into smaller fragments |
Carboxypeptidase |
Pancreas |
Small intestine |
Polypeptides into amino acids |
Lipid digestion |
|||
Lipase |
Pancreas |
Small intestine |
Triglycerides (fats) into fatty acids and glycerol |
Fats present a special digestive challenge because they are insoluble in water. You have observed this when the oil (a fat) quickly separates from the vinegar (a water solution) in your salad dressing. In water, droplets of fat tend to coalesce into large globules. This poses a problem for digestion because lipase, the enzyme that chemically breaks down fats, is soluble in water and not in fats. As a result, lipase can work only at the surface of a fat globule. Large fat globules have less combined surface area than do smaller droplets, so their digestion by lipase proceeds more slowly.
Bile, a mixture of water, ions, cholesterol, bile pigments, and bile salts, plays an important role in the mechanical digestion of fats, which assists lipase in chemically digesting fats. The bile salts emulsify fats; that is, they keep fats separated into small droplets that disperse in liquid. This separation exposes a larger combined surface area to lipase, making the chemical digestion and absorption of fats faster and more complete. Bile is produced by the liver, is stored in the gallbladder, and acts in the small intestine.
We have more to say about the pancreas, liver, and gallbladder shortly.
Structure of the small intestine. The small intestine, the primary site of absorption in the digestive system, is extremely effective at its task because it is long and has several structural specializations that vastly increase its surface area (Figure 15.8). First, the entire lining of the small intestine is pleated, like an accordion, into circular folds. These circular folds increase the surface area for absorption and cause chyme to flow through the small intestine in a spiral pattern. The spiral flow helps mix the chyme with digestive enzymes and increases its contact with the absorptive surfaces. Covering the entire lining surface are tiny 1-mm projections called villi (singular, villus). The villi give the lining a velvety appearance and, like the pile on a bath towel, increase the absorptive surface. Indeed, the villi increase the surface area of the small intestine tenfold. In addition, the absorptive epithelial cells covering the surface of each villus contain thousands of microscopic projections, called microvilli, that increase the surface area of the small intestine by another 20 times. The microvilli form a fuzzy surface, known as a brush border. The circular folds, villi, and microvilli create a surface area of 300 to 600 m2—greater than the size of a tennis court!
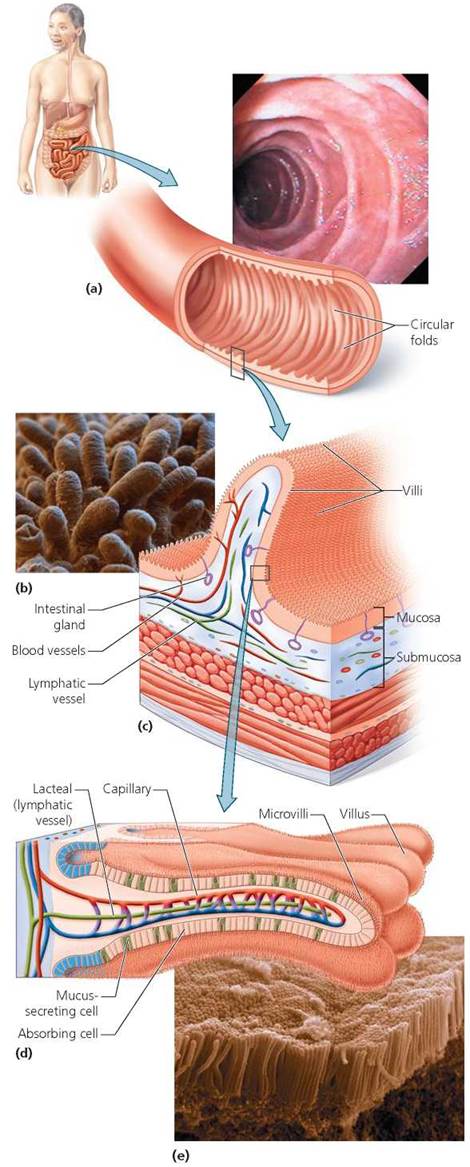
FIGURE 15.8. The small intestine is specialized for the absorption of nutrients by structural modifications that increase its surface area.
(a) Its wall contains accordion-like pleats called circular folds, (b) This electron micrograph shows the intestinal villi, the numerous fingerlike projections on the intestinal lining (the mucosa in part c). (d) The surface of each villus bristles with thousands of microscopic projections (of cell membranes) called microvilli. In the center of each villus, a network of blood capillaries, which carries away absorbed products of protein and carbohydrate digestion as well as ions and water, surrounds a lacteal (a small vessel of the lymphatic system) that carries away the absorbed products of fat digestion, (e) An electron micrograph of the microvilli that cover each villus.
List three structural adaptations of the small intestine that increase its surface area for absorption of digested nutrients.
Circular folds, villi, and microvilli.
The core of each villus is penetrated by a network of capillaries and a lacteal, which is a lymphatic vessel. As substances are absorbed from the small intestine, they cross only two cell layers: the epithelial cells of the villi and the wall of either a capillary or a lacteal. Most materials enter the epithelial cells by active transport, facilitated diffusion, or simple diffusion (Figure 15.9; see Chapter 3). Monosaccharides, amino acids, water, ions, vitamins, and minerals diffuse across the capillary wall into the bloodstream and are delivered to body cells. The products of fat digestion, glycerol and fatty acids, combine with bile salts in the small intestine, creating particles called micelles (my-cells). When a micelle contacts an epithelial cell of a villus, the products of fat digestion easily diffuse into the cell. Within an epithelial cell, the glycerol and fatty acids are reassembled into triglycerides, mixed with cholesterol and phospholipids, and coated with special proteins, thus becoming part of a complex known as a chylomicron (kI-lo-mI-,kran). The protein coating makes the fat soluble in water, allowing it to be transported throughout the body. The chylomicrons leave the epithelial cell by exocytosis (see Chapter 3). Chylomicrons are too large to pass through capillary walls. However, they easily diffuse into the more porous lacteal and enter the lymphatic system, which carries them to the bloodstream.
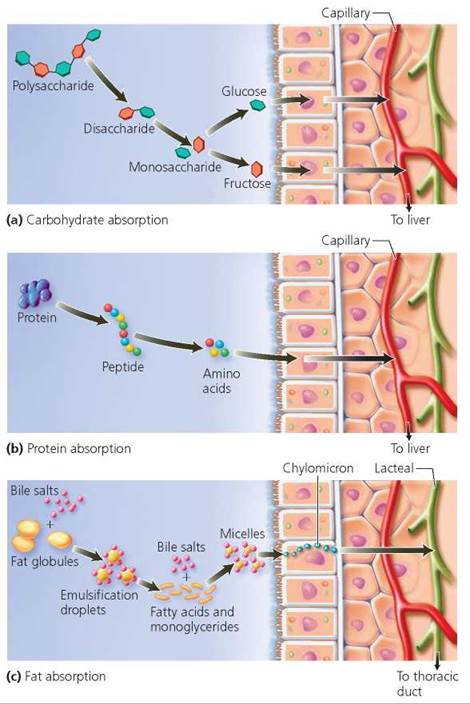
FIGURE 15.9. The small intestine is the primary site for chemical digestion and absorption. The digestive products, such as monosaccharides, amino acids, fatty acids, and glycerol, enter absorptive epithelial cells of villi by active transport, facilitated diffusion, or diffusion. Monosaccharides and amino acids, along with water, ions, and vitamins, then enter the capillaries within the villus and are carried to body cells by the bloodstream. The products of fat digestion diffuse into the lacteal within the villus.
Accessory Organs: Pancreas, Liver, and Gallbladder
The pancreas, liver, and gallbladder are not part of the GI tract. However, they play vital roles in digestion by releasing their secretions into the small intestine. The functions of the secretions of the accessory organs are summarized in Table 15.3.
TABLE 15.3. Review of Accessory Structures of the Digestive System
Structure |
Secretions/Functions |
Site of Action of Chemical Secretions |
Salivary glands (sublingual, submandibular, parotid) |
Secrete saliva, a liquid that moistens food and contains an enzyme (amylase) for digesting carbohydrates |
Mouth |
Pancreas |
Digestive secretions include bicarbonate ions that neutralize acidic chyme and enzymes that digest carbohydrates, proteins, fats, and nucleic acids |
Small intestine |
Liver |
Digestive function is to produce bile, a liquid that emulsifies fats, making chemical digestion easier and facilitating absorption |
Small intestine |
Gallbladder |
Stores bile and releases it into small intestine |
Small intestine |
Pancreas. The pancreas is an accessory organ that lies behind the stomach, extending toward the person's left from the small intestine. Pancreatic juice drains from the pancreas into the pancreatic duct, which fuses with the common bile duct from the liver just before entering the duodenum of the small intestine (Figure 15.10). In addition to enzymes, pancreatic juice contains water and ions, including bicarbonate ions that are important in neutralizing the acid in chyme when it emerges from the stomach. Neutralization is essential for optimal enzyme activity in the small intestine.
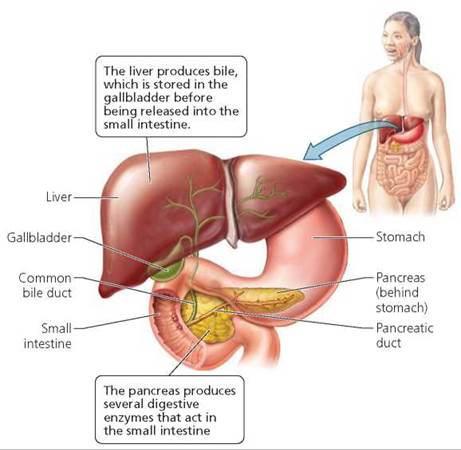
FIGURE 15.10. The pancreas, liver, and gallbladder are accessory organs of the digestive system.
Collectively, the pancreatic enzymes and intestinal enzymes break nutrients into their component building blocks: proteins to amino acids, carbohydrates to monosaccharides, and triglycerides (a type of lipid) to fatty acids and glycerol.
Liver. The nutrient-laden blood from the capillaries in the villi travels through the hepatic portal vein to the liver, the largest internal organ in the body, which has a variety of metabolic and regulatory roles. A portal system consists of the blood vessels that link two capillary beds. The hepatic portal system delivers blood from a capillary bed in the small intestine to a second capillary bed in the liver (Figure 15.11).
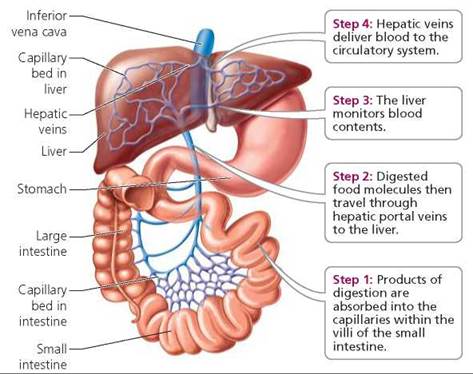
FIGURE 15.11. A portal system transports blood from one capillary bed to another. In the hepatic portal system the hepatic portal vein carries blood from the capillary network of the villi of the small intestine to the capillary beds of the liver. The liver monitors blood content and processes nutrients before they are delivered to the bloodstream.
Where are the two capillary beds in the hepatic portal system? What does the liver do in this system?
The small intestine and the liver. The liver monitors and adjusts blood content.
We have already seen that the liver's primary role in digestion is to produce bile. One of its other roles is to control the glucose level of the blood, either removing excess glucose and storing it as glycogen or breaking down glycogen to raise blood glucose levels. Thus, the liver keeps the glucose levels of the blood within the proper range. The liver also packages lipids with protein carrier molecules to form lipoproteins, which transport lipids in the blood. After the liver adjusts the blood composition, the blood is returned to the general circulation through the hepatic veins. In addition, the liver stores iron and vitamins A, D, E, K, B12, and folate.
The liver also removes poisonous substances, including lead, mercury, and pesticides, from the blood and in some cases breaks them down into less harmful chemicals. What's more, the liver converts the breakdown products of amino acids into urea, which can then be excreted by the kidney. These are but a few of the approximately 500 functions of the liver.
Considering the liver's many vital functions, it is no surprise that diseases of the liver can be serious and life threatening. Cirrhosis is a condition in which the liver becomes fatty and gradually deteriorates, its cells eventually being replaced by scar tissue. Because cirrhosis is sometimes caused by prolonged, excessive alcohol use, it is discussed in Chapter 8a.
Hepatitis is inflammation of the liver. It is most commonly caused by one of six viruses, designated as A, B, C, D, E, and G. Although all the hepatitis viruses attack the liver and destroy liver cells, there are differences in their means of transmission and their symptoms, as well as their severity. Healthy liver cells remove bilirubin, a yellowish pigment produced by the breakdown of red blood cells, from the bloodstream and use it to make bile. All forms of hepatitis do have one symptom in common: liver cells injured by hepatitis viruses stop filtering bilirubin from the blood. The accumulating bilirubin is deposited in the skin and the whites of the eyes, giving them a yellowish tint. This condition, called jaundice, is characteristic of any disease that damages the liver.
Currently, about 4 million people in the United States have hepatitis C, and most of them have no idea that they are infected. For years, the disease has spread silently because it has no outward warning signs or very mild symptoms—vague fatigue, or flu-like muscle and joint pain. It is spread primarily through contaminated blood. Hundreds of thousands of intravenous drug users have been infected by sharing contaminated needles. Hepatitis C can also be spread through contaminated needles used in body piercing or tattooing. Before there was a way to test for the virus, many people became infected when they received transfusions with contaminated blood.
Health Issue
Peptic Ulcers
At some point in their lives, nearly 13% of Americans experience a failure of the mechanisms that protect the stomach and duodenum from their acidic contents, so that the lining of some region in the GI tract becomes eroded. The resulting sore resembles a canker sore of the mouth and is called a peptic ulcer (Figure 15.A). Although a peptic ulcer may form in the esophagus or the stomach, the most common site is the duodenum of the small intestine. Ulcers are usually between 10 and 25 mm (0.33 and 1 in.) in diameter and may occur singly or in multiple locations.
The symptoms of an ulcer are variable. A common symptom is abdominal pain, which can be quite severe. Vomiting, loss of appetite, bloating, indigestion, and heartburn are other common symptoms. However, some people with ulcers, especially those who are taking nonsteroidal antiinflammatory drugs (NSAIDs), have no pain. Unfortunately, the degree of pain is a poor indicator of the severity of ulceration. Often, people with no symptoms are unaware of their ulcers until serious complications develop. Gastric juice can erode the lining of the GI tract until it bleeds. In some cases, the ulcer can eat a hole completely through the wall of the GI tract (a condition called perforated ulcer). Recurrent ulcers can cause scar tissue to form, which may narrow or block the lower end of the stomach or duodenum.
Although acidic gastric juice is the direct cause of peptic ulcers, factors that interfere with the mechanisms that normally protect the lining of the GI tract from the acid are considered to be the real causes. For example, NSAIDs, which include aspirin, ibuprofen, and naproxen, can cause ulcers because they slow the production of chemicals called prostaglandins, which normally help protect the lining of the GI tract from damage by acid.
The leading cause of peptic ulcers, however, is an infection with the bacterium Helicobacter pylori. More than 80% of persons with ulcers in the stomach or duodenum are infected with H. pylori. This bacterium produces an alkaline compound that neutralizes the stomach acid. These corkscrew-shaped bacteria live in the layer of mucus that protects the lining of the GI tract. Here, the bacteria attract body defense cells—specifically, macrophages and neutrophils—that cause inflammation, leading to ulcer formation. Toxic chemicals produced by the bacteria also contribute to ulcers.
H. pylori infections may last for years. These bacteria affect more than a billion people throughout the world and approximately 50% of the people in the United States who are over 60 years of age. For some reason, however, only about 10% to 15% of those who are infected actually develop peptic ulcers. Besides ulcers, an H. pylori infection is a risk factor for esophageal and stomach cancer. However, it may soon be possible to vaccinate children against this bacterium, thereby reducing the risk of both peptic ulcers and stomach cancer.
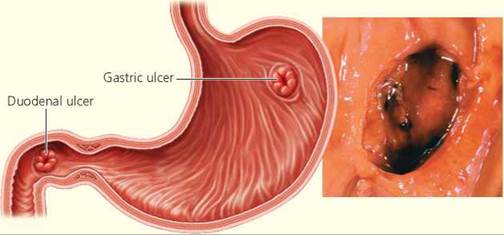
FIGURE 15.A. A peptic ulcer is an open sore that forms when gastric juice erodes the lining of the esophagus, stomach, or, most commonly, the duodenum. The ulcer shown in this stomach wall is bleeding. The most common symptom is abdominal pain that occurs when the stomach is empty.
Questions to Consider
• If you were going to have an endoscopy, a procedure in which a long flexible tube with a camera is used to view your esophagus or stomach, would you request that the physician test for the presence of H. pylori at the same time?
• The Korean- and Japanese-American populations have an exceptionally high rate of stomach cancer. Would you recommend that people in these populations be routinely screened for the presence of H. pylori?
Gallbladder. After it is produced by the liver, bile is stored, modified, and concentrated in a muscular, pear-shaped sac called the gallbladder. When chyme enters the small intestine, a hormone causes the gallbladder to contract, squirting bile through the common bile duct into the duodenum of the small intestine.
Bile is rich in cholesterol. Sometimes, if the balance of dissolved substances in bile becomes upset, a tiny crystalline particle precipitates out of solution. Cholesterol and other substances can then build up around the particle to form a gallstone (Figure 15.12). Many people develop several gallstones, which can cause problems if they block the flow of bile and may necessitate surgical removal of the gallbladder.
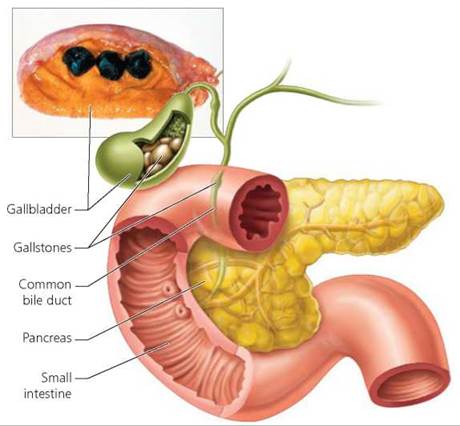
FIGURE 15.12. Gallstones consist primarily of cholesterol that has precipitated from bile during storage in the gallbladder. A gallstone can intermittently or continuously block the ducts that drain bile into the small intestine. The photograph shows a gallbladder and several gallstones.
Large Intestine
Now that we have discussed the accessory organs that assist digestion and absorption in the small intestine, we go back to following the movement of ingested substances through the GI tract. The material that was not absorbed in the small intestine moves into the final major structure of the digestive system, the large intestine. The principal functions of the large intestine are (1) to absorb most of the water remaining in the indigestible food residue, thereby adjusting the consistency of the waste material, or feces; (2) to store the feces; and (3) to eliminate them from the body. The large intestine is home to many types of bacteria, some of which produce vitamins that may be absorbed for use by the body.
Regions of the large intestine. The large intestine has four regions: the cecum, colon, rectum, and anal canal, as shown in Figure 15.13. The cecum is a pouch that hangs below the junction of the small and large intestines. Extending from the cecum is another slender, wormlike pouch, called the appendix. The appendix has no digestive function. Some scientists believe the appendix plays a role in the immune system, which protects the body against disease.
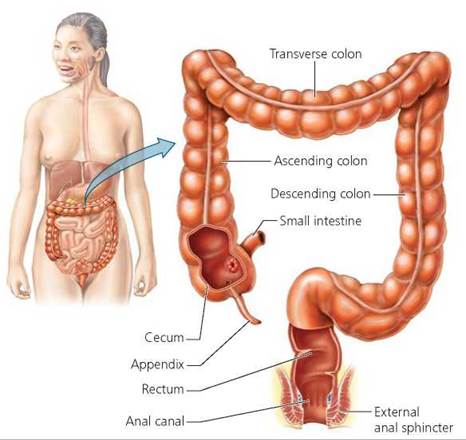
FIGURE 15.13. The large intestine consists of the cecum, colon, rectum, and anal canal. It absorbs water from undigested material, forming the feces, and houses bacteria.
Each year, about 1 in 500 people develops appendicitis, inflammation of the appendix. Appendicitis is usually caused by an infection that arises in the appendix after it becomes blocked by a piece of hardened stool from the cecum, food, or a tumor. After the blockage occurs, bacteria that are normally present in the appendix can multiply and cause an infection. At first, appendicitis is usually experienced as vague bloating, indigestion, and a mild pain in the region of the navel (bellybutton). As the condition worsens, the pain becomes more severe and is localized in the region of the appendix, the lower right abdomen. The pain is typically accompanied by fever, nausea, and vomiting. When appendicitis is diagnosed, antibiotics are administered and the infected appendix is surgically removed. Untreated infection in the appendix usually causes the appendix to rupture, allowing its infected contents to spill into the abdominal cavity. Spillage from the appendix generally leads to infection and inflammation throughout the abdomen (a condition called peritonitis), which is potentially fatal.
The largest region of the large intestine, the colon, is composed of the ascending colon on the right side of the abdomen, the transverse colon across the top of the abdominal cavity, and the descending colon on the left side (see Figure 15.13). Although much of the water that is originally in chyme is absorbed in the small intestine, the material entering the colon is still quite liquid. The colon absorbs 90% of the remaining water and sodium and potassium ions. The material left in the large intestine after passing through the colon is called feces and consists primarily of undigested food, sloughed-off epithelial cells, water, and millions of bacteria. The brown color of feces comes from bile pigments.
The bacteria in the colon are not normally disease causing and, in fact, are beneficial. Intestinal bacteria produce several vitamins that we are unable to produce on our own, including vitamin K and some of the B vitamins. Some of these vitamins are then absorbed from the colon for our own use. There are roughly 50 species of bacteria, including the well-known Escherichia coli (E. coli) that live in the healthy colon. Bacteria are nourished by undigested food and by material that we are unable to digest, including certain components of plant cells. When the intestinal bacteria use the undigested and indigestible food for their own nutrition, their metabolic processes liberate gas that sometimes has a foul odor. Although most of the gas is absorbed through the intestinal walls, the remaining gas can produce some embarrassing moments when released as flatus.
People who are lactose intolerant lack the enzyme lactase, which is normally produced by and acts in the small intestine. Lactase breaks down lactose, the primary sugar in milk, into its component monosaccharides. Without lactase, then, lactose moves intact into the colon, where it provides a nutritional bonanza for the bacteria living there. As a result, when people who are lactose intolerant consume milk products, the intestinal bacteria ferment the lactose and produce the gases carbon dioxide and methane that, in turn, produces bloating, gas, and abdominal discomfort. Although lactose intolerance is common in adults, it is not dangerous. Problems can usually be avoided by swallowing capsules or tablets of lactase or by modifying the diet to avoid dairy products.
Stop and think
Certain foods—beans, for instance—are notorious for producing intestinal gas. Beans contain large amounts of certain shortchain carbohydrates that our bodies are unable to digest. How is the nutritional content of beans related to flatulence?
Periodic peristaltic contractions move material through the large intestine, but these contractions are slower than the contractions in the small intestine. Slower contractions allow for adequate water absorption as material moves through the large intestine. Eventually, the feces are pushed into the rectum, stretching the rectal wall and initiating the defecation reflex. Nerve impulses from the stretch receptors in the rectal wall travel to the spinal cord, which sends motor impulses back to the rectal wall, stimulating muscles there to contract and propel the feces into the anal canal. Two rings of muscles, called sphincters, must relax to allow defecation, the expulsion of feces. The internal sphincter relaxes automatically as part of the defecation reflex. The external sphincter is under voluntary control, allowing the person to decide whether to defecate. Conscious contraction of the abdominal muscles can increase abdominal pressure and help expel the feces.
Disorders of the colon. The water absorption that occurs in the colon adjusts the consistency of feces. When material passes through the colon too rapidly, as might occur when colon contractions are stimulated by toxins from microorganisms or by excess food or alcoholic drink, too little water is absorbed. As a result, the feces are very liquid. This condition, which results in frequent loose stools, is called diarrhea. Persistent diarrhea can be dangerous, especially in an infant or young child, because it can lead to dehydration. Diarrhea is a major cause of death worldwide.
On the other hand, if material passes through the colon too slowly, too much water is absorbed, resulting in infrequent, hard stools—a condition called constipation. People who are constipated may need to strain during bowel movements. Straining increases pressure within veins in the rectum and anus, causing them to stretch and enlarge. The wall of the large intestine also experiences great pressure during a strained bowel movement. Then, like the inner tube of an old tire, the weaker spots in the intestinal wall can begin to bulge outward, forming small pouches called diverticula (singular, diverticulum; Figure 15.14). Diverticula are very common in people older than age 50. When diverticula do not cause problems or symptoms, the condition is called diverticulosis. But if the diverticula become infected with bacteria and inflamed, the condition is then called diverticulitis, which can cause abrupt, cramping abdominal pain, a change in bowel habits, fever, and rectal bleeding. Diverticulitis can be treated by changing the diet (increasing fiber, avoiding nuts), taking drugs that reduce muscle spasms, or having surgery.
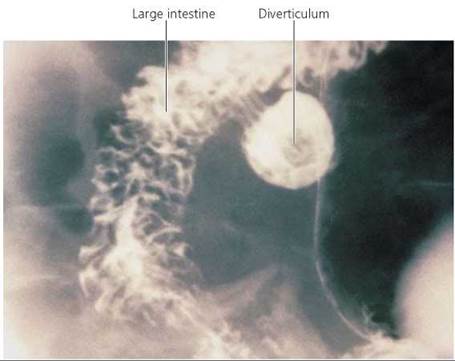
FIGURE 15.14. A diverticulum is a small pouch that forms in the wall of the large intestine and is usually caused by repeated straining during bowel movements. A high-fiber diet results in softer, bulkier stools that are easier to pass, thus making it less likely that diverticula will form.
Stop and think
Stimulant laxatives enhance peristalsis in the large intestine but do not affect the small intestine. Some people with eating disorders use laxatives to speed the movement of food through the digestive system, thinking that the calories in the food will not be absorbed. Are they correct in their thinking? After purging in this way, the person may weigh less on the bathroom scale. What accounts for the weight loss? Could laxative use help a person lose body fat?
Cancers of the colon or rectum are common and can be deadly. Colorectal cancer is the second leading cause of cancer deaths. Early detection and treatment cut the risk of death dramatically.
Colorectal cancer begins with a small, noncancerous growth called a polyp. If the polyp continues to grow, genetic mutations accumulate in it that can transform a cell into a cancerous tumor. Polyps may take as long as 10 years to grow and turn cancerous, generally allowing plenty of time for detection. Sometimes polyps bleed, so one sign of colorectal polyps and perhaps cancer is blood in the stool. However, the blood is not usually visible and must be detected with a diagnostic test. Because many polyps do not bleed, screening methods that allow a direct view of the wall of the rectum and colon are generally more effective. A long, flexible fiberoptic tube is threaded through the first third of the colon in a procedure known as a sigmoidoscopy, or through the entire colon in a procedure called a colonoscopy. If a polyp is detected, it can be removed and biopsied to determine whether it is cancerous (see Chapter 21a).
Nerves and Hormones in Digestion
As we have seen, ingested material moves along the GI tract, stopping for specific kinds of treatment along the way. For digestion to occur, enzymes must be present in the right place at the right time. However, because the body is composed of many of the same substances found in food, digestive enzymes should not be released until food is present (otherwise the enzymes might start digesting the digestive system). Both nerves and hormones play a role in orchestrating the release of digestive secretions, timing the release of each to the presence of food at each stop.
Food spends little time in the mouth; so to be effective, saliva must be secreted quickly. Because nervous stimulation is faster than hormonal stimulation, it is not surprising to learn that the nervous system controls salivation. Some saliva is released before food even enters the mouth, which may begin to "water" simply at the thought of food—and certainly begins at the sight or smell of food. The major trigger for salivation, however, is the presence of food in the mouth—its flavor and pressure. Salivary juices continue to flow for some time after the food is swallowed, helping to rinse out the mouth.
While food is still being chewed, neural reflexes stimulate the stomach lining to begin secreting gastric juice and mucus. Distention of the stomach by swallowed food, along with the presence of partially digested proteins, stimulates cells in the stomach lining to release the hormone gastrin. Gastrin enters the bloodstream and circulates throughout the body and back to the stomach, where it increases the production of gastric juice.
The presence of acidic chyme in the small intestine, which triggers local nerve reflexes, is the most important stimulus for the release of enzymes from both the small intestine and the pancreas, as well as bile from the gallbladder. Acid chyme also causes the small intestine to release several hormones that, in turn, are responsible for the release of digestive enzymes and bile. For instance, one hormone, vasoactive intestinal peptide, is released from the small intestine into the bloodstream and is carried back to the small intestine, where it causes the release of intestinal juices. At the same time, the small intestine releases a second hormone, secretin, which stimulates the release of sodium bicarbonate from the pancreas into the small intestine to help neutralize the acidity of chyme. A third hormone from the small intestine is cholecystokinin (ko'li-s/s-td-fa'-nin), which causes the pancreas to release its digestive enzymes and causes the gallbladder to contract and release bile. The neural and hormonal controls of the digestive system are summarized in Tables 15.4 and 15.5, respectively.
Looking ahead
In this chapter, we have seen how the digestive system is organized to break down food molecules for energy or building materials. In the next chapter, we learn about our body's use of specific nutrients and consider how what we eat affects our health.
TABLE 15.4. Examples of Neural Controls on Digestive Activity
Stimulus |
Effect |
Sight of food, thought of food, presence of food in mouth |
Release of saliva from salivary glands |
Chewing food |
Release of gastric juice (enzymes from stomach and HCl) and mucus from cells of stomach lining |
Presence of acidic chyme in small intestine |
Release of enzymes from small intestine and pancreas into the small intestine; release of bile from gallbladder into small intestine; increased motility in small intestine |
TABLE 15.5. Examples of Hormonal Control on Digestive Activity
Hormone |
Stimulus |
Origin |
Target |
Effects |
|
Gastrin |
Distention of stomach by food; presence of partially digested proteins in stomach |
Stomach |
Stomach |
Release of gastric juice (enzymes from stomach and HCl) |
|
Vasoactive intestinal peptide |
Presence of acidic chyme in small intestine |
Small intestine |
Small intestine |
Release of enzymes from small intestine |
|
Secretin |
Presence of acidic chyme in small intestine |
Small intestine |
Pancreas |
Release of sodium bicarbonate from pancreas into small intestine to neutralize acidic chyme |
|
Cholecystokinin |
Arrival of chyme-containing lipids |
Small intestine |
Pancreas |
Release of enzymes from pancreas |
|
|
Gall bladder |
Contraction of gallbladder and release of bile |
|||
Highlighting the Concepts
The Gastrointestinal Tract (pp. 285-286)
• The digestive system consists of a long tube called the gastrointestinal (GI) tract, which starts at the mouth and continues through the pharynx, esophagus, stomach, small intestine, and large intestine. The digestive system also includes several accessory organs (salivary glands, pancreas, liver, and gallbladder).
• The GI tract has four layers. Moving from the inside out, they are the mucosa, submucosa, muscularis, and serosa.
Specialized Compartments for Food Processing (pp. 286-298)
• The mouth serves several functions. Teeth tear and grind food, making it easier to swallow. The salivary glands produce salivary amylase, which is released into the mouth to begin the chemical breakdown of starches. Taste buds help monitor the quality of food. Finally, the tongue manipulates food so that it can be swallowed.
• The pharynx is shared by the digestive and respiratory systems. Food swallowed moves from the mouth through the pharynx and into the esophagus.
• The esophagus is a tube that leads to the stomach. When we swallow, food is pushed from the mouth, and waves of muscle contraction called peristalsis push the food along the esophagus.
• The stomach stores food and regulates its release to the small intestine, liquefies it by mixing it with gastric juice, begins the chemical digestion of proteins, and regulates the release of chyme into the small intestine. Gastric juice consists of hydrochloric acid (HCl) and pepsin, a protein-splitting enzyme. Pepsin is produced in an inactive form, called pepsinogen, that is activated by HCl.
• The small intestine is the primary site of digestion and absorption, where enzymes produced by the small intestine and pancreas work to chemically digest carbohydrates, proteins, and fats into their component subunits.
• Bile emulsifies fat (breaks it into tiny droplets) in the small intestine, thereby increasing the combined surface area of fat droplets. Bile's action makes fat digestion by water-soluble lipase faster and more complete.
• The small intestine's surface area for absorption is increased by circular folds in its lining, fingerlike projections called villi, and microscopic projections covering the villi, called microvilli.
• Products of digestion are absorbed into the epithelial cells of villi by active transport, facilitated diffusion, or simple diffusion. Most materials, including monosaccharides, amino acids, water, and ions, then enter the capillary blood network in the center of each villus. However, fatty acids and glycerol are resynthesized into triglycerides, combined with cholesterol and phospholipids, and covered in protein, forming droplets called chylomicrons. The chylomicrons diffuse into a lymphatic vessel called a lacteal in the core of each villus. They are then delivered to the bloodstream by way of lymphatic vessels.
• The pancreas, liver, and gallbladder are accessory organs that aid in digestion and absorption within the small intestine. The pancreas secretes enzymes to digest most nutrients. The liver produces bile, which is then stored in the gallbladder.
• The large intestine consists of the cecum, colon, rectum, and anal canal. The large intestine absorbs water, ions, and vitamins. It is home to millions of beneficial bacteria that live on undigested material that has passed from the small intestine. The bacteria produce several vitamins, some of which we then absorb for our own use.
• Material left in the large intestine after passing through the colon is called feces. Feces consist of undigested or indigestible material, bacteria, sloughed-off cells, and water. Defecation is the discharge of feces from the rectum through the anus.
Nerves and Hormones in Digestion (p. 298)
• Neural and hormonal mechanisms regulate the release of digestive secretions. Neural reflexes trigger the release of saliva, initiate the secretion of some gastric juice, and are the most important factors regulating the release of intestinal secretions. Gastrin, vasoactive intestinal peptide, secretin, and cholecystokinin are hormones that regulate digestive activities.
Reviewing the Concepts
1. List the structures of the GI tract, in the order that food passes through them. p. 286
2. Describe how food is processed in the mouth. What are the functions of the teeth and tongue? pp. 286-289
3. Describe the structures of a tooth that are involved in tooth decay. What causes tooth decay? pp. 287-288
4. What are the three primary functions of the stomach? What are the functions of gastric juice? pp. 290-291
5. Why are so few substances absorbed from the stomach? p. 291
6. How does bile assist in the digestion and absorption of fats? p. 291
7. Where are carbohydrates digested? Proteins? Fats? pp. 291-292
8. Describe the structural features that increase the surface area for absorption in the small intestine. pp. 291-292
9. Which structures produce the digestive enzymes that act in the small intestine? p. 291
10. What are the functions of the large intestine? p. 295
11. Describe the neural or hormonal mechanisms that regulate the release of digestive juices from each structure involved in digestion. p. 298
12. The villi in the wall of the small intestine function to
a. increase the surface area for absorption.
b. help mix the food with digestive enzymes.
c. secrete bile.
d. secrete digestive enzymes.
13. It is possible to swallow while standing on one's hands because
a. valves in the digestive system keep food from moving backward.
b. peristalsis pushes food along the digestive tract in the right direction.
c. bacteria clog the digestive tube and prevent food from moving in the wrong direction.
d. of a wave of muscle contraction called emulsification.
14. The most important function of the stomach is
a. absorption of nutrients.
b. chemical digestion.
c. mucus secretion.
d. storage of food.
15. You go out with your friends to celebrate your birthday and share a sausage pizza. The digestion of the oil begins in the
a. mouth.
b. esophagus.
c. stomach.
d. small intestine.
16. _____ is a liquid mixture of food and gastric juices found in the stomach.
17. The _____ is the organ that produces bile.
18. Saliva contains an enzyme that begins the chemical digestion of _____.
19. _____ is a hormone produced by the small intestine that causes the gallbladder to contract and release bile.
Applying the Concepts
1. Barbara is a 20-year-old woman with cystic fibrosis, a genetic disease in which abnormally thick mucus is produced. The thick mucus sometimes blocks the pancreatic duct that allows pancreatic juice to enter the small intestine. Explain why cystic fibrosis has caused Barbara to be malnourished.
2. Dehydration occurs when too much body fluid is lost. It can be a serious, even fatal, condition. Doctors worry about dehydration if a person, especially an infant, has severe diarrhea lasting several days. Why?
3. A 35-year-old man sporting a tattoo visits the dermatologist to have the tattoo removed. Noticing that the patient's skin has a yellowish tint, the dermatologist strongly recommends that the patient visit a physician. Why? What is the dermatologist concerned about?
4. You spend the day with your Aunt Sally on her 55th birthday. She has a salad for lunch and suffers no ill effects. However, she indulges in fried chicken and French fries for dinner. A few hours later, she is rushed to the emergency room with a severe pain on the right side of her abdomen. She reports that she has had bouts of pain over the last month or so. What do you think is Aunt Sally's problem? Why isn't the pain continuous?
Becoming Information Literate
The PillCam is a small camera that is swallowed by the patient and takes pictures of the GI tract as it moves through the body. Write a short article for the health section of a local newspaper, describing the PillCam in more detail and answering the following questions in easily understood words. How does a PillCam differ from a traditional endoscope? What conditions and diseases can be diagnosed using the PillCam? Compared with endoscopy, what are the advantages and disadvantages of the PillCam?
Use at least three reliable sources (books, journals, or websites). List each source you considered, and explain why you chose the three sources you used.