Biology of Humans
5. The Skeletal System
In the previous chapter, we became familiar with our organ systems. In this chapter, we will consider the skeletal system and see its role in determining our physical appearance. We will examine the structure of bone and see why it is able to support our bodies against gravity. We’ll also consider our joints, places where bones meet, and see how they permit movement. In reading about the structure and properties of bone in this chapter, you may be surprised to learn that bone is a dynamic, living tissue and to discover the number of functions our skeletal system performs.
Bone Functions
The skeleton is a framework of bones and cartilage that performs the following functions for the body:
1. Support. It provides a rigid framework that supports soft tissues. The leg bones and backbone hold our bodies upright, and the pelvic girdle supports the abdominal organs.
2. Movement. It provides places of attachment for muscles. Contraction of muscles allows bones to move at joints.
3. Protection. It shields our internal organs, such as the heart and lungs, which are enclosed within the chest cavity, and the brain, which lies within the skull.
4. Storage of minerals. It stores minerals, particularly calcium and phosphorus, that can be released to the rest of the body when needed.
· The 206 bones of the human body provide support against gravity and protect internal organs. The joints, places where bones meet, determine the type of movement that is possible.
5. Storage of fat. It stores energy-rich fat in yellow bone marrow (the soft tissue within some bones). The fat can be metabolized when the energy is needed.
6. Blood cell production. It produces blood cells in the red marrow of certain bones.
Bone Structure
The 206 bones of the human body come in a range of sizes and a variety of shapes. Most bones contain both compact and spongy bone in proportions that depend on the bone's size and shape.
Compact bone is very dense, with few internal spaces (Figure 5.1). It forms most of the shaft of long bones, such as those of the arms and legs. In the body, compact bone (except for the joint surfaces) is covered by a glovelike membrane, the periosteum, that nourishes the bone. The periosteum contains blood vessels and nerves as well as cells that function in bone growth and repair. The blood vessels pass through the periosteum and extend into the underlying bone. When a bone is bruised or fractured, most of the pain results from injury to the periosteum.
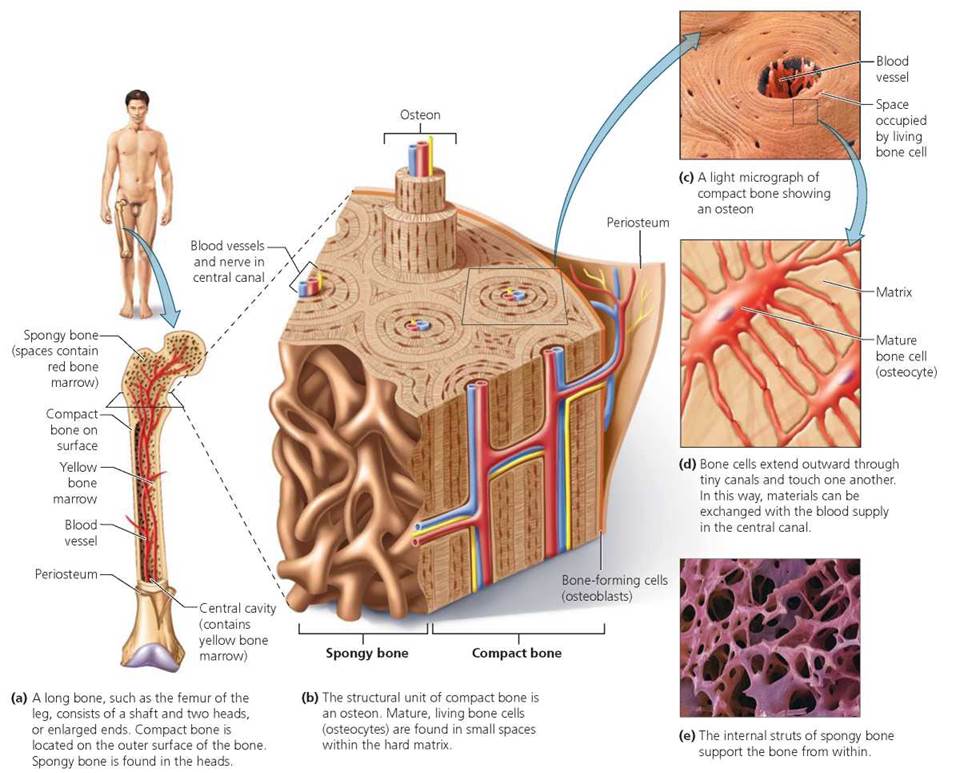
FIGURE 5.1. The structure of bone
Spongy bone is a latticework of tiny beams and thin plates of bone with open areas between. This internal network braces the bone from within. Spongy bone is largely found in small, flat bones, such as most of the bones of the skull, and in the heads (enlarged ends) and near the ends of the shafts of long bones (refer to Figure 5.1). Some of the spongy bone in adults (for example, in the ribs, pelvis, backbone, skull, sternum, and long-bone ends) is filled with red marrow, where blood cells form. The cavity in the shaft of adult long bones is filled with yellow marrow, a fatty tissue used for energy storage.
Bone as a Living Tissue
Compact bone is highly organized living tissue containing a microscopic, repeating structural unit called an osteon (shown in Figure 5.1). Each osteon consists of mature bone cells, called osteocytes (osteo, bone; cyte, cell), arranged in concentric rings around a central canal. Each osteocyte lies within a tiny cavity called a lacuna in the hardened matrix. Tiny canals connect nearby lacunae and eventually connect with the central canal. Similarly, the osteocytes have projections that extend through the tiny canals to touch neighboring cells. Nutrients, oxygen, and wastes pass from cell to cell, traveling to or from the blood vessels in the central canal.
As noted, bone is a living tissue. But its most noticeable characteristics result from its nonliving component, the solid matrix, which makes the bone both hard and resilient. The hardness of the matrix comes from mineral salts, primarily calcium and phosphorus. The resilience comes from strands of the strong, elastic protein collagen that are woven throughout the matrix. Without the calcium and phosphorus salts, bone would be rubbery and flexible like a garden hose. Without the collagen, bone would be brittle and crumbly like chalk. In some disorders, bones do bend, causing bowlegs. An example is rickets, in which the amount of calcium salts in the bones is greatly reduced.
Stop and think
Strontium-90 is a radioactive substance that enters the atmosphere after atomic explosions. Humans may ingest it in milk from cows that grazed on contaminated grass. The strontium-90 can then replace calcium in bone, killing nearby cells or altering their genetic information. Explain why exposure to strontium-90 can lead not just to bone cancer but also to disruption of blood cell formation.
Cartilage Model
During human embryonic development, most of the skeleton is first formed of cartilage, a strong yet flexible connective tissue (Figure 5.2). Unlike mature bone cells, which cannot divide because they are enclosed in a solid matrix, cartilage cells are able to divide and multiply quickly. Thus, the cartilage model can grow as rapidly as the fetus does. Beginning in the third month and continuing through prenatal development, the cartilage is gradually replaced by bone.
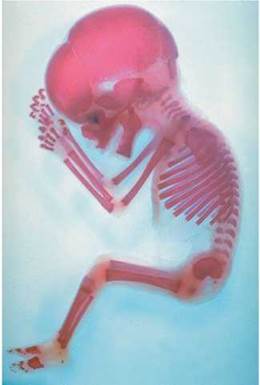
FIGURE 5.2. The fetal skeleton is first made of cartilage and gradually replaced by bone. This image shows the cartilaginous model of the skeleton of a 16-week-old human fetus. The darker areas of this skeleton are regions that have already been replaced with bone.
It is recommended that young adult women consume 1100 to 1300 mg of calcium each day, but that requirement doubles during pregnancy. Explain why.
Calcium is needed for replacing the cartilage with bone in the skeleton of the fetus.
The transformation from cartilage to a mature long bone, such as an arm or leg bone, begins with the formation of a collar of bone around the shaft of the cartilaginous model. The collar is produced by bone-forming cells called osteoblasts (osteo, bone; blast, beginning or bud). Osteoblasts produce the matrix of bone around the shaft by secreting collagen (as well as other organic materials) and then depositing calcium salts on it. The bony collar supports the shaft as the cartilage within it breaks down, leaving the marrow cavity. Blood vessels then carry osteoblasts into the bone cavity, which in turn fill the cavity with spongy bone. Unlike cartilage cells, osteoblasts cannot undergo cell division. Once osteoblasts form the matrix around themselves, they are called osteocytes, which, as we have seen, are mature bone cells and the principal cells in bone tissue.
Near the time of birth, bone growth centers form in the ends of long bones, and spongy bone begins to fill them. Two kinds of structures made of cartilage will remain. One is a cap of cartilage over each end of the bone, where one bone glides over another in a joint. The second is a plate of cartilage, called an epiphyseal plate, that separates each end of the bone from its shaft. The epiphyseal plate is commonly called the growth plate. Cartilage cells within the growth plate divide, forcing the end of the bone farther away from the shaft. As bone replaces the newly formed cartilage in the region closer to the shaft, the bone becomes longer. Note that the diameter of the bone also enlarges as the bone lengthens (Figure 5.3).
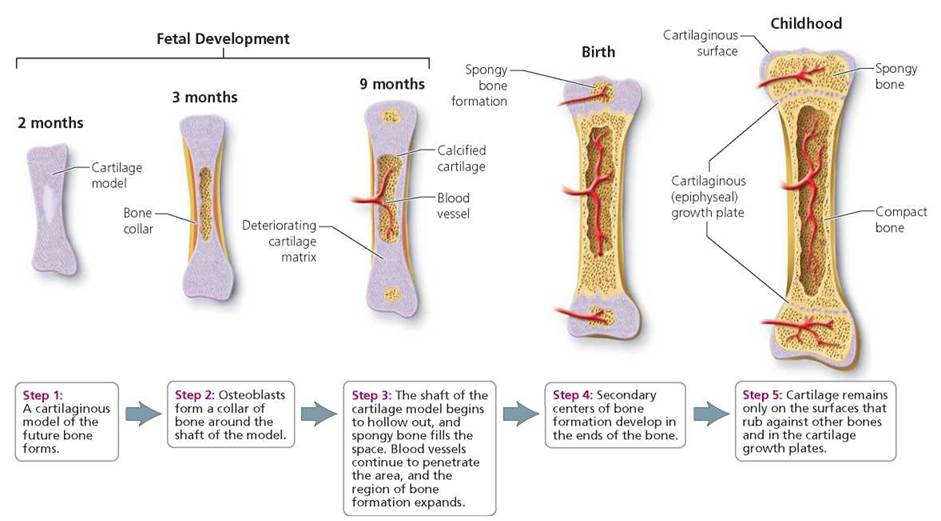
FIGURE 5.3. Steps of bone formation in long and short bones, from an embryo into childhood
Hormones and Bone Growth
During childhood, bone growth is powerfully stimulated by growth hormone, which is released by the anterior pituitary gland (see Chapter 10). Growth hormone prompts the liver to release growth factors that produce a surge of growth in the growth plate. Thyroid hormones modify the activity of growth hormone to ensure that the skeleton grows with the proper proportions.
At puberty, many children experience a growth spurt during which the length of pant legs seems to shrink almost weekly. These dramatic changes are orchestrated by the increasing levels of sex hormones (testosterone and estrogen) produced during puberty. Initially the sex hormones stimulate the cartilage cells of the growth plates into a frenzy of cell division. But this growth generally stops toward the end of the teenage years (about age 18 in females and 21 in males) because of later changes initiated by the sex hormones. The cartilage cells in the growth plates start dividing less frequently. Eventually, the growth plates become thinner as bone replaces cartilage. Finally, the ends of the bone where the growth plates were fuse with the bone in the shaft. Note that even though bones can no longer lengthen at this stage, they can continue to widen.
Stop and think
We have considered the mechanism by which long bones grow and the role of growth hormone in that process. Why would it be ineffective for a short, middle-aged person to be treated with growth hormone to stimulate growth?
The Role of Fibroblasts and Osteoblasts in Repairing Bone Fractures
Despite their great strength, bones occasionally break. Fortunately, bone tissue can heal. When a bone breaks, the first thing that happens is bleeding from blood vessels in the bone and periosteum, followed by formation of a clot (hematoma) at the break (Figure 5.4). Within a few days, connective tissue cells called fibroblasts grow inward from the periosteum and invade the clot. The fibroblasts secrete collagen fibers that form a mass called a callus, which links the broken surfaces of the bone. Some of the fibroblasts then transform into cartilage-producing cells that secrete cartilage into the callus.
Next, osteoblasts from the periosteum invade the callus and begin to transform the newly deposited cartilage into new bone material, changing it into a bony callus. During this transformation, the bony callus becomes thicker than the undamaged part of the bone and protrudes from it. In time, however, the extra material will be broken down, and the healed part of the bone returns to nearly normal size.
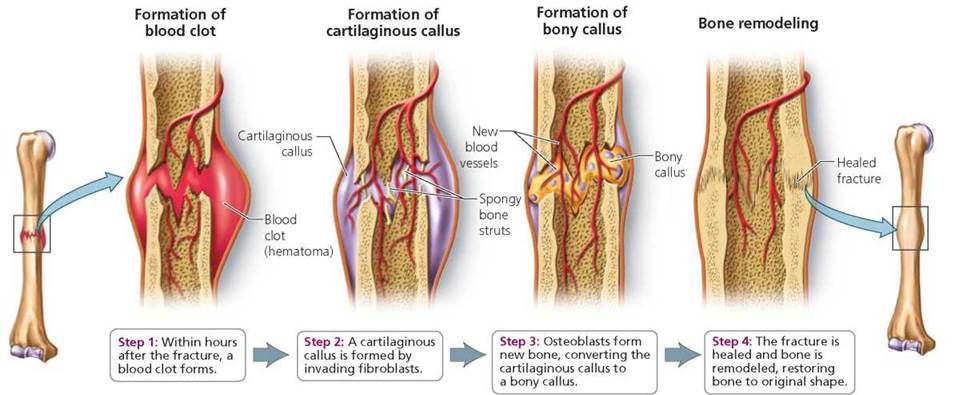
FIGURE 5.4. The progress of healing in a bone
Stop and think
Osteogenesis imperfecta is a condition in which the activities of osteoblasts and fibroblasts are abnormally low. What affects would you expect this to have on the skeletal system?
Bone Remodeling
Even after reaching our full height, we continue to undergo a lifelong process of bone deposition and breakdown called remodeling. Bone remodeling keeps bones strong by repairing tiny cracks in bones, such as might occur if you jump from a high place. We have seen that bone is deposited by osteoblasts. Another kind of bone cell, called an osteoclast, breaks down bone, releasing calcium and other minerals that are reabsorbed by the body. Thus, bone remodeling is also a mechanism for regulating blood calcium levels, which is important because calcium plays a role in the functioning of nerves and muscles as well as blood clotting.
Two hormones, calcitonin and parathyroid hormone, play an important part in both the control of bone remodeling and the regulation of blood levels of calcium. When blood levels of calcium are high, as might occur after a meal, the hormone calcitonin, which is released from the thyroid gland, removes calcium from the blood and causes it to be stored in bone. Calcitonin brings about these effects by stimulating the activities of osteoblasts while inhibiting those of osteoclasts. In contrast, when blood calcium levels are low, parathyroid hormone (PTH), which is released by the parathyroid glands found embedded in the tissues of the thyroid gland, causes calcium to be released from bone and reabsorbed into the blood. PTH accomplishes this by stimulating the activities of osteoclasts. The interplay of these two hormones keeps blood calcium levels fairly steady. (The regulation of blood calcium levels is discussed in more detail in Chapter 10.)
In women, estrogen also plays a role in bone remodeling. It promotes the absorption of calcium from the digestive system, stimulates bone formation, and impairs the ability of osteoclasts to break down bone.
During bone remodeling, new bone forms along the lines of stress on the bone. Bone forms in response to stress and gets absorbed when it is not stressed. Weight-bearing exercise, such as walking or jogging, thickens the layer of compact bone tissue, leading to a stronger bone. Bones that are used frequently may actually change shape. For example, continual practice may enlarge the knuckles of pianists and the big toes of ballet dancers. On the other hand, a few weeks without stress can cause a bone to lose nearly a third of its mass. This is a concern for astronauts living in the weightless environment of space as well as for a person who is using crutches with a leg in a cast.
If the breakdown process occurs faster than the deposition of new tissue, a bone becomes weak and easy to break. This imbalance occurs in osteoporosis, a condition in which there is a progressive loss in bone density. (See the Health Issue essay, Osteoporosis: Fragility and Aging.) Now that we are familiar with factors regulating bone growth and remodeling, we can understand why certain medications are used to treat osteoporosis. The bisphosphonates, such as Fosamax, Actonel, and Boniva, inhibit the osteoclasts that break down bone, but not the osteoblasts that build bone. Evista is an example of another class of drug, called selective estrogen receptor modulators (SERMs), that mimic the effects of estrogen on the bones. The thyroid hormone calcitonin can also be used to treat osteoporosis, because it increases the amount of calcium deposited in bones.
Axial Skeleton
The human skeleton can be divided into two parts: the axial skeleton and the appendicular skeleton (see Figure 5.5). The axial skeleton (shown here in orange) includes the skull, the vertebral column (backbone), and the bones of the chest region (sternum and rib cage). The appendicular skeleton (shown in light brown) includes the pectoral girdle (shoulders), the pelvic girdle (pelvis), and the limbs (arms and legs).
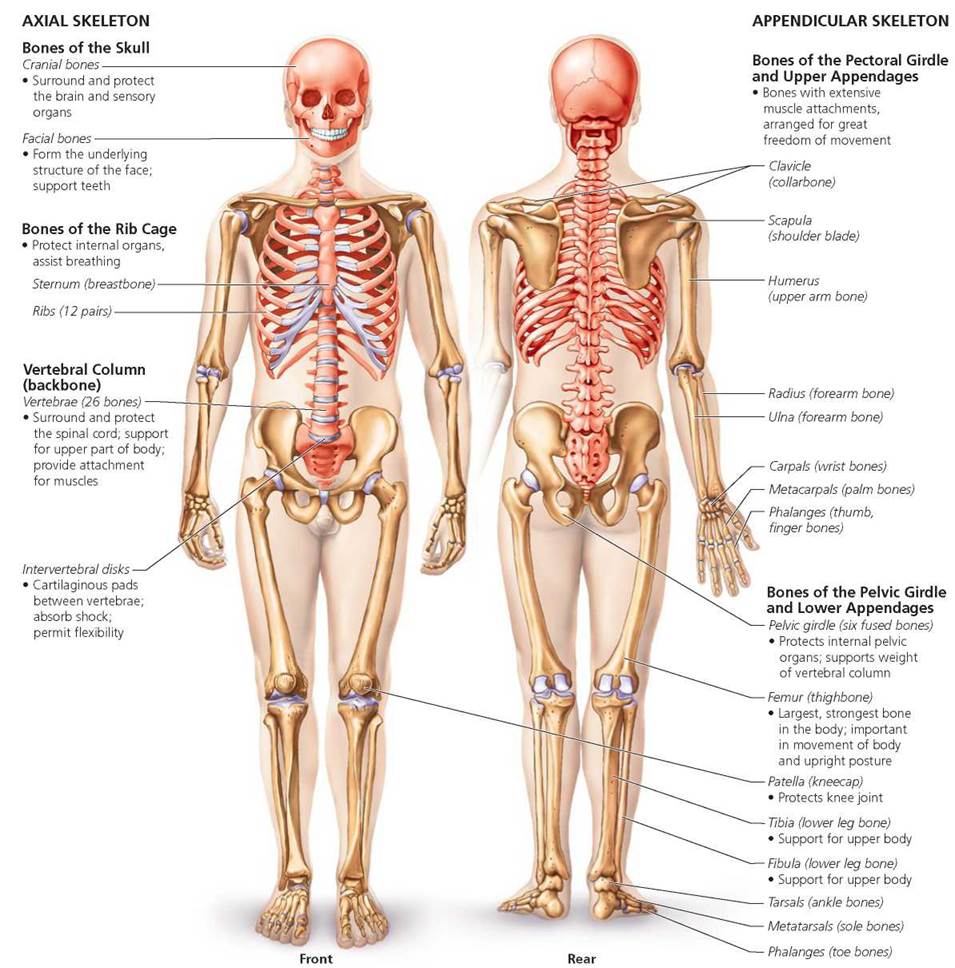
FIGURE 5.5. Major bones of the human body. Bones of the axial skeleton are shown In orange; bones of the appendicular skeleton are shown in light brown. Cartilage is shown in light purple.
In general, the axial skeleton protects and supports our internal organs. We will focus on only the major bones of the 80 that make up this portion of the skeleton, beginning with the bones of the skull.
Skull
The skull is the most complex bony structure in the body (Figure 5.6). Its principal divisions are the cranium and the face. Several bones of the skull contain air spaces called sinuses, which make the head lighter in weight and serve as resonating chambers for the voice, as discussed in Chapter 14.
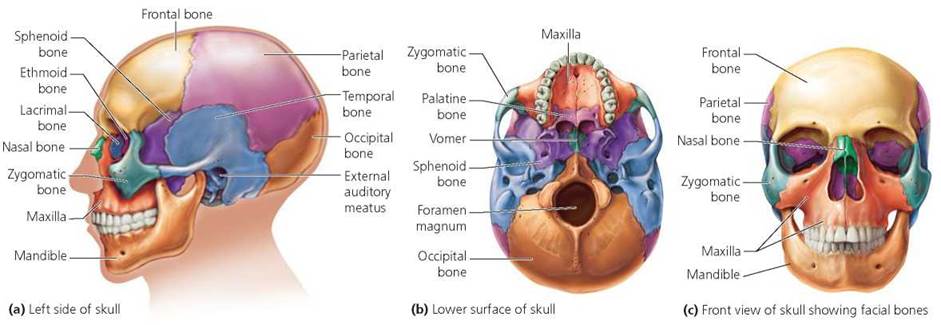
FIGURE 5.6. Major bones of the skull and face
The cranial bones. The cranium protects the brain, houses the structures of hearing, and provides attachment sites for the muscles of the head and neck. It is formed from eight (or sometimes more) flat bones. The single frontal bone forms the forehead and the front of the brain case. Behind it, extending from either side of the midline, the two parietal bones form the top and sides of the skull. The occipital bone lies at the back of the head and surrounds the foramen magnum, the opening through which the spinal cord passes.
Before and shortly after birth, the bones of the cranium are connected by membranous areas called the fontanels, often referred to as soft spots. During birth, the fontanels allow the skull to be compressed, easing the passage of the head through the birth canal. The fontanels also accommodate the rapid enlargement of the brain during fetal growth and infancy (Figure 5.7). They are replaced by bone by the age of 2 years.

FIGURE 5.7. The skull bones of a human newborn are not fused but are instead connected by fibrous connective tissue. These “soft spots" allow the skull bones to move during the birth process, easing the passage of the skull through the birth canal. By 2 years of age, the child’s soft spots have been replaced by bone.
The cranium also contains the temporal bones, part of which form what we think of as our temples. The sphenoid bone, with its bow-tie shape, forms the cranium's floor. The ethmoid bone, the smallest bone in the cranium, separates the cranial cavity from the nasal cavity. The olfactory nerves from the nasal cavity, which are responsible for our sense of smell, communicate with the brain through tiny holes in the ethmoid.
Health Issue
Osteoporosis: Fragility and Aging
About 40 million Americans, most of them elderly white women, suffer from osteoporosis —a decrease in bone density that occurs when the breakdown of bone outpaces the formation of new bone during bone remodeling. The net breakdown causes bones to become thin, brittle, and susceptible to fracture. A person with osteoporosis becomes hunched and shorter as the vertebrae lose mass and compress (Figure 5.A). A fall, blow, or lifting action that would not bruise a person with healthy bones could easily cause a bone to fracture in a person with severe osteoporosis.
As we have seen, bone remodeling occurs throughout life. Until we reach about age 35, bone is formed faster than it is broken down. Our bones are strongest and densest during our mid-thirties, after which they begin to lose density. Peak bone density is influenced by several factors, including sex, race, nutrition (dietary levels of calcium and vitamin D), exercise (we have seen the importance of weight-bearing exercise), and overall health. In men, bone mass is generally 30% higher than in women. The bones of African Americans are generally 10% denser than those of Caucasians and Asians.
Women are at greater risk for developing osteoporosis than are men. This difference is not just because women have less bone mass at peak but also because their rate of bone loss is accelerated for several years after menopause (the time in a woman's life when she stops producing mature eggs or menstruating). The acceleration occurs because menopause is followed by a sharp decline in the hormone estrogen, and estrogen stimulates bone formation and is important in the absorption of calcium from the intestines.
Other factors have been implicated in the onset of osteoporosis. For example, height is important. Short people are at greater risk, perhaps because they generally start with less bone mass. People with a good supply of body fat are less at risk because fat can be converted to estrogen. Heavy drinkers are at higher risk, because alcohol interferes with estrogen function. Smoking is also bad for bones, because it can reduce estrogen levels. We have already noted that people who do not take in enough calcium, or who cannot absorb it because of insufficient vitamin D, have thinner bones because calcium is necessary for bone growth. (Calcium-rich foods include milk products as well as broccoli, spinach, shrimp, and soybean products.) Certain drugs, such as caffeine (a diuretic), tetracycline, and cortisone, can promote osteoporosis. Finally, as mentioned earlier, sedentary people have thinner bones than do active people.
The degree to which our bones will become weakened as we age depends largely on how dense they were at their peak. We can expect osteoporosis and other afflictions associated with aging to become more common as life expectancy increases. Thus, it would seem prudent for each of us to start an early program of prevention. To build strong bones, eat a diet rich in calcium and vitamin D. As adults, we need 1100 to 1300 mg of calcium each day; so eat 3 to 4 servings of foods rich in calcium and vitamin D. Engage in regular weight-bearing exercise, such as walking or jogging, for 30 minutes every day. Avoid drinking alcohol and caffeinated beverages, and don't smoke cigarettes.
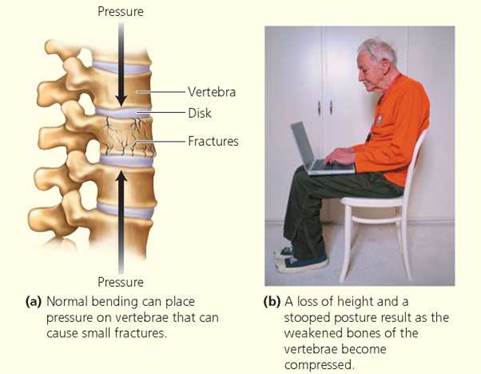
FIGURE 5.A. Osteoporosis is a loss of bone density that occurs when bone destruction outpaces bone deposition during the continuous process of bone remodeling. The bones become brittle and are easily fractured.
Questions to Consider
• Would diving or cross-country skiing on a regular basis be more likely to build bone density?
• If your mother were approaching menopause, what advice would you give her to help her maintain bone density?
Facial bones. The 14 bones of the face (Figure 5.6c) support several sensory structures and serve as attachments for most facial muscles.
The nasal bones form the bridge of the nose. They are paired and fused at the midline. Inside the nose, a partition called the nasal septum (composed of the vomer and part of the ethmoid bone) divides the left and right chambers of the nasal cavity.
Cheekbones are formed largely from the paired zygomatic bones. Flat areas of these bones form part of the bottom of the eye sockets. Each zygomatic bone has an extension that joins with an extension from the temporal bone to form the zygomatic arch (the "cheekbone").
The smallest facial bones are the two lacrimal bones, located at the inner corners of the eyes, near the nose. A duct passes through each lacrimal bone and drains tears from the eyes into the nasal chambers; this connection explains why our nose runs when we cry.
The jaw is formed by two pairs of bones, the maxillae and the pair that forms the mandible. The maxillae form the upper jaw. Most of the other facial bones are joined to them, giving the upper jaw an important role in facial structure. The maxillae also form part of the hard palate, or roof of the mouth, the rest of which is formed by the two palatine bones that lie behind. When the maxillae fail to fuse to one another at the midline of the face below the nasal septum, the mouth cavity and nasal cavity do not fully separate, and a cleft palate results. This condition is easily corrected by surgery.
The lower jaw, called the mandible, is also formed from two bones connected at the midline. The mandible is connected to the skull at the temporal bone, forming a hinge called the temporomandibular joint. (Joints are discussed later in this chapter.) This joint allows the mouth to open and close. Emotional stress causes some people to clench or grind their teeth, sometimes unconsciously. This clenching can cause physical stress on the temporomandibular joint, causing headaches, toothaches, or even earaches. The condition is known as temporomandibular joint (or TMJ) syndrome.
Vertebral Column
The vertebral column, known more familiarly as the backbone or spine, is a series of bones through which the spinal cord passes as it descends the back (Figure 5.8). Each of these bones is called a vertebra. The vertebrae (plural of vertebra) are classified according to where they lie along the vertebral column. The vertebral column includes 26 vertebrae, organized as follows:
• 7 cervical (neck) vertebrae (C1-C7)
• 12 thoracic (chest) vertebrae (T1-T12)
• 5 lumbar (lower back) vertebrae (L1-L5)
• 1 sacrum (formed by the fusion of five sacral vertebrae)
• 1 coccyx (or tailbone, formed by fusion of four vertebrae)
Scoliosis, which means "twisted disease," is an abnormal curvature of the spine to the left or right. The most common form has no known cause and affects over 1.5 million adolescents, primarily females. It usually begins during, and progresses through, the adolescent growth spurt. Treatment, if needed, may consist of a brace or surgery to straighten the spine.
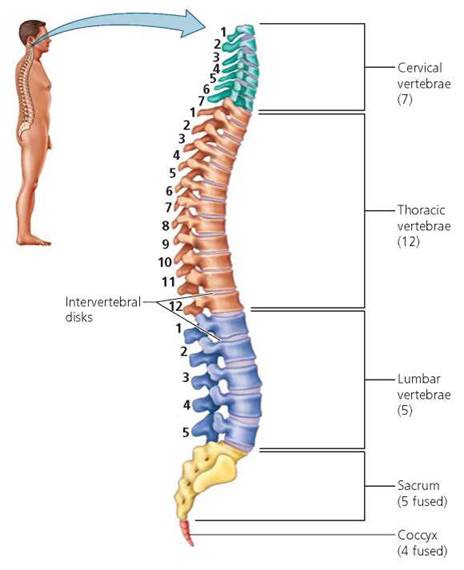
FIGURE 5.8. A side view of the vertebral column
The fusion of the sacral vertebrae into a single sacrum gives additional strength to the backbone in the region where the sacrum joins the pelvic girdle. This reinforcement is necessary because of the great stress placed on the sacrum by the weight of the vertebral column and the powerful movements of the leg. The coccyx, on the other hand, serves no function and is regarded as a vestigial tail (vestigial means "an evolutionary relic") whose bones may have joined as a side effect of growth without movement. (The upper part of the coccyx, however, is supplied with nerves and can be extremely painful when injured.)
Above the sacrum, the vertebrae are separated from one another by intervertebral disks, pads of fibrocartilage that help cushion the bones of the vertebral column. The smooth, lubricated surfaces of these disks help give the column flexibility. As the intervertebral disks become compressed over the years, the person may become shorter. This compression, alone or coupled with osteoporosis, can have a pronounced effect on an aging person's height.
Excessive pressure on the disks, as might occur during improper lifting, can cause various problems. The term slipped disk is a misnomer, because a disk doesn't actually move out of place. Instead, it bulges. If a disk bulges inward, it can press against the spinal cord, interfering with muscle control and perception of incoming stimuli. On the other hand, a disk that presses outward against a spinal nerve branching from the spinal cord can be a source of great pain. The sciatic nerve, a large nerve that extends down the back of the leg, is one of the nerves most frequently affected in this way. Sciatica, the resulting inflammation, can be cripplingly painful.
Lower back pain is a particularly mysterious human ailment that accounts for more missed workdays than does any medical problem besides colds. The source of the pain is notoriously difficult to pinpoint. A person with a slipped disk in the region may or may not have pain, whereas a person whose back looks perfectly normal may complain of terrible pain. Part of the diagnostic problem seems to be that the pain may originate solely from muscle rather than bone, and muscles do not show up on x-rays. Some cases may occur because of weak abdominal muscles that cannot counteract the pull of the powerful back muscles and therefore cause the vertebrae to misalign.
Rib Cage
Twelve pairs of ribs attach at the back of the rib cage to the thoracic vertebrae (Figure 5.9). At the front, the upper 10 pairs of ribs are attached by cartilage either directly or indirectly to the sternum (breastbone). Their flexibility permits the ribs to take some blows without breaking and to move during breathing. The last two pairs of ribs do not attach to the sternum and are called floating ribs (although they are attached at the back to the thoracic vertebrae).
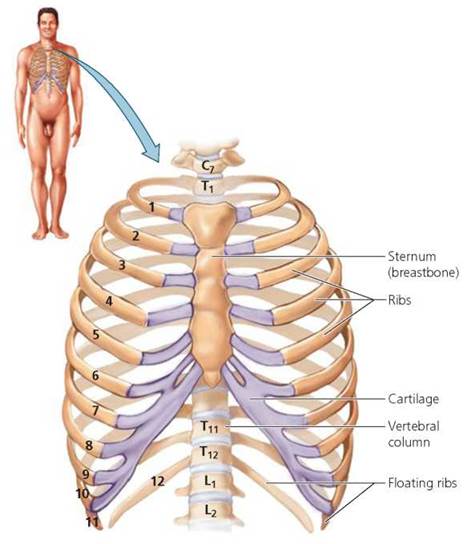
FIGURE 5.9. The bones of the rib cage. Cartilage is shown in light purple.
Appendicular Skeleton
The appendicular skeleton consists of the pectoral and pelvic girdles and the attached limbs. A girdle is a skeletal structure that supports the arms, in the case of the pectoral girdle, or the legs, in the case of the pelvic girdle. The pectoral girdle connects the arms to the rib cage. The pelvic girdle connects the legs to the vertebral column, enabling the body to move from one place to another.
Pectoral Girdle
The pectoral girdle is composed of the scapulae (shoulder blades) and the clavicles (collarbones; Figure 5.10). The clavicles are more curved in males than in females (one way to tell the sex of a skeleton), and each forms a relatively rigid bridge between a scapula and the sternum. One corner of the roughly triangular scapula has a socket into which fits one end of the humerus, the upper arm bone. The other end of the humerus joins, at the elbow, the radius and ulna—the bones of the lower arm, or forearm. The elbow is formed by the extension of the ulna past the junction with the humerus. The radius and ulna meet the eight carpals at the wrist, and these join with the five metacarpals, which are the bones of the hand. Each finger includes three phalanges, and the thumb includes two.
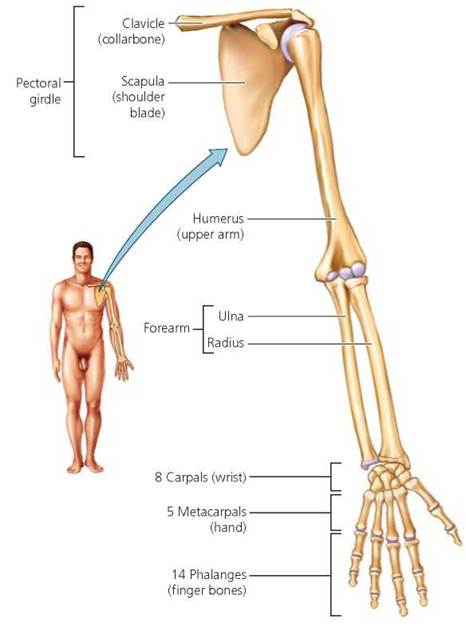
FIGURE 5.10. The pectoral girdle and arm
The carpal tunnel is a narrow opening through the carpal bones that form the wrist, and through it passes a nerve that controls sensations in the fingers and in some of the muscles in the hand. Tendons, bands of connective tissue that attach muscles to bones, also pass through the carpal tunnel. Repetitive motion in the hand or wrist can cause these tendons to become inflamed and press against the nerve, resulting in numbness or tingling in the hand and pain that may affect the wrist, hand, and fingers. This condition, known as carpal tunnel syndrome, has been experienced by barbers, cab drivers, and pianists. It is increasingly common as people spend more time operating computer keyboards and playing video games. The computer industry has responded by redesigning the keyboards and games. Employers have responded, too, by providing adjustable workstations and rest and exercise periods.
What would you do?
People who have developed carpal tunnel syndrome after endless hours of using keyboards and video game controllers are bringing a rash of lawsuits against computer manufacturers and video game designers. If you developed carpal tunnel syndrome from using a keyboard or video game, would you sue the manufacturer? What criteria would you use to decide?
Pelvic Girdle
The pelvic girdle is much more rigid than the pectoral girdle (as you know if you have ever tried to shrug your hips). The two pelvic bones that make up the pelvic girdle (Figure 5.11) attach in back to the sacrum. The pelvic bones curve down and around to the front, where they join to a cartilage disk at the pubic symphysis. The male and female hips are easily distinguishable because the opening of the pelvic girdle in the female is wider to facilitate childbirth.
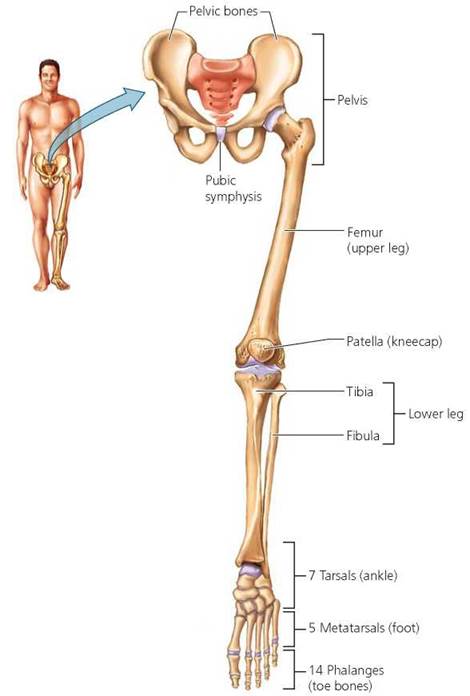
FIGURE 5.11. The pelvic girdle and leg
The femur, or thighbone, rotates within a socket in the pelvis. At the knee, the femur joins the tibia (the shinbone). The fibula is a smaller bone running down the side of the tibia. The junction where the tibia joins the femur is covered by a patella (kneecap). At the ankle, the lower leg bones meet the tarsals, or ankle bones. These are connected to the metatarsals, or foot bones, which in turn are connected to the toe bones, called phalanges (as with finger bones).
Joints
Joints are the places where bones meet. They can be classified as fibrous, cartilaginous, or synovial, depending on their components and structure. Some joints allow no movement; others permit slight movement; and still others are freely movable.
Fibrous joints are held together by fibrous connective tissue. They have no joint cavity, and most fibrous joints do not permit movement. For example, the joints between the skull bones of an adult, called sutures, are considered to be immovable because the bones are interlocked and held together tightly by fibrous connective tissue (Figure 5.12). In fact, the sutures can actually move ever so slightly. This ability is fortunate, because the movements serve as a shock absorber when you hit your head.
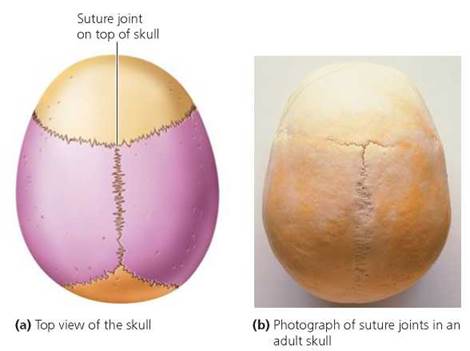
FIGURE 5.12. The bones of the skull are joined by suture joints.
Cartilage, which is rather rigid, holds bones together in cartilaginous joints. Some cartilaginous joints are immovable, and others allow slight movement. We find cartilaginous joints between vertebrae; in the attachment of ribs to the sternum; and in the pubic symphysis, the joint between the two pelvic bones. In a pregnant woman, hormones loosen the cartilage of the pubic symphysis, allowing the pelvis to widen to ease childbirth.
Synovial Joints
Most of the joints of the body are freely movable synovial joints. Because of these joints, muscles can maneuver the body into thousands of positions. All synovial joints share certain common features. One is that the surfaces that move past one another in the joints have a thin layer of cartilage. The cartilage reduces friction, so the bones slide over one another without grating and grinding. In addition, a two-layered joint capsule surrounds synovial joints. The inner layer of the capsule, the synovial membrane, secretes viscous, clear fluid (synovial fluid) into the space, or joint cavity, between the two bones. The synovial fluid lubricates and cushions the joint. The outer layer of the capsule is continuous with the covering membranes of the bones forming the joint. The entire synovial joint is reinforced with ligaments, strong straps of connective tissue that hold the bones together, support the joint, and direct the movement of the bones.
All synovial joints share these features but may differ in the type and range of motion they permit (Figure 5.13). As the name implies, hinge joints, such as at the knee and elbow, resemble a hinge on a door in that they permit motion in only one plane. A ball-and-socket joint, such as the shoulder and hip, allows movement in all planes: the ball at the head of one bone fits into a socket on another bone. Notice that you can swing your arm around in a complete circle. Some of the ways that body parts move at synovial joints are shown in Figure 5.14.
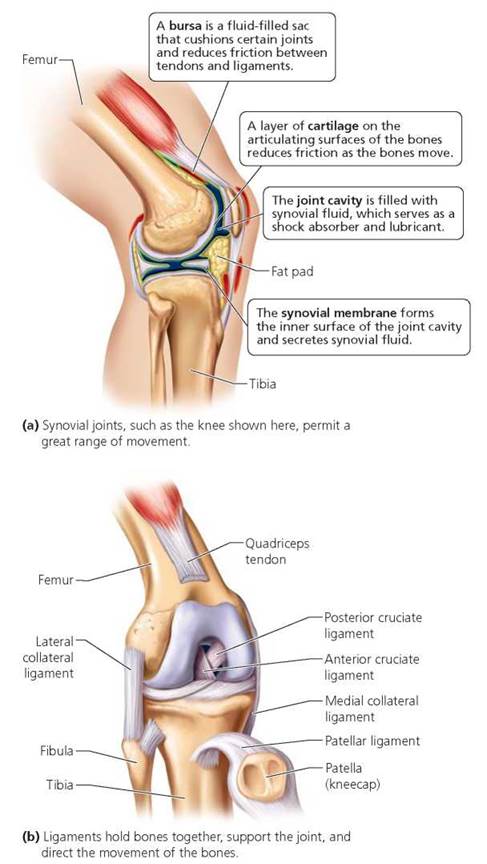
FIGURE 5.13. The knee is a synovial joint.
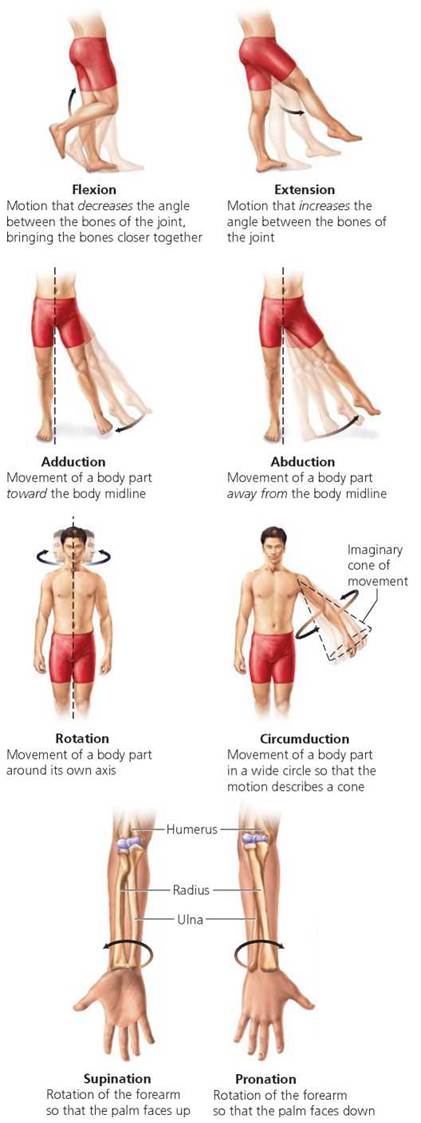
FIGURE 5.14. Types of movement at synovial joints
Damage to Joints
Damage to a ligament is called a sprain and may range from slight, caused by overstretching, to serious, caused by tearing of the ligament. A torn ligament results in swelling and enough pain to inhibit movement. Sometimes, because ligaments are covered with a concentration of pain receptors that are very sensitive to stretching and swelling, the injury is not as severe as the pain would suggest. As with most musculoskeletal swelling, the initial treatment is likely to be an ice pack to reduce the swelling. Ice constricts underlying blood vessels and reduces bleeding. Bleeding would stop by the next day. Then, heat would be applied to dilate blood vessels, allowing blood to carry in the nutrients, oxygen, and anti-inflammatory chemicals that assist healing. Like tendons, ligaments have few blood vessels and therefore heal slowly.
A common knee injury among athletes, especially gymnasts and football and soccer players, is a tear in the anterior cruciate ligament (ACL) (Figure 5.15). Why is this ligament so vulnerable? When the knee is bent, the ACL acts as a restraining wire that restricts front-to-back twisting movement between the thighbone (femur) and the shinbone (tibia). An external blow to a bent knee—as may occur during a tackle or a hard landing—can stretch the ACL. If the force applied to the two bones is greater than the strength of the ligament, the ACL can tear.

FIGURE 5.15. A common sports injury is a tear in the anterior cruciate ligament of the knee.
In synovial joints and certain other locations where movement might cause friction between moving parts, the body has its own "ball bearings" in the form of fluid-filled sacs called bursae (singular, bursa; meaning "pouch or purse"). Bursae are lined with synovial membranes. They are found in places where skin rubs over bone as the joint moves and between tendons and bones, muscles and bones, and ligaments and bones.
Joint injury or repeated pressure can cause bursae to become inflamed and swell with excess fluid, a condition called bursitis (-itis means "an inflammation"). For example, the repetitive movement of throwing a baseball or swinging a tennis racket may cause bursitis in the elbow. Bursitis is characterized by intense pain that becomes worse when the joint is moved and that cannot be relieved by resting in any position. Nonetheless, bursitis is not serious and usually subsides on its own within a week or two. In severe cases, a physician may drain some of the excess fluid to remove the pressure.
Arthritis
Arthritis is a general term referring to joint inflammation. Some of the more than 100 kinds of arthritis are far more serious than others. Osteoarthritis is a degeneration of the surfaces of a joint, caused by wear and tear. Eventually the slippery cartilage at the ends of the affected bones begins to disintegrate until the bones themselves come into contact and grind against each other, causing intense pain and stiffness. Any joint surface that undergoes friction is bound to wear down, but osteoarthritis is most likely to occur in weight-bearing joints, such as the hip, knee, and spine. It is also occasionally seen in the finger joints or wrist.
Prevention is always better than treatment. One tip for preventing osteoarthritis is to control your weight to avoid overburdening your knees and hips. Another tip is to exercise. Lifting weights will strengthen the muscles that help support your joints. Stretching will give you a greater range of movement.
A far more threatening form of arthritis is rheumatoid arthritis. Rheumatoid arthritis is marked by inflammation of the synovial membrane. The resulting accumulation of synovial fluid in the joint causes swelling, pain, and stiffness. Eventually, the constant irritation can destroy the cartilage, which may then be replaced by fibrous connective tissue that further impedes joint movement.
Rheumatoid arthritis differs from other types of arthritis in that it is an autoimmune disease. That is, the body mistakenly attacks its own synovial membranes just as it would some invasive foreign matter. Rheumatoid arthritis can vary in severity over time, but it is a permanent condition. It normally affects the joints of the fingers, wrist, knees, neck, ankles, and hips. Sometimes the only effective treatment is to replace the damaged joint with an artificial one (Figure 5.16).

FIGURE 5.16. Replacement prosthesis of the hip
Looking ahead
In this chapter, we learned about our bony framework. In the next chapter, we will consider how muscles put flesh on our bones and attach to bones so that when our muscles contract, we can move.
Highlighting the Concepts
Bone Functions (pp. 88-89)
• The skeleton is a framework of bone and cartilage that supports and protects the internal organs and has a role in movement. It also serves as a storage site for minerals (calcium and phospho rus) and fat. Blood cells are produced in the red marrow of certain bones.
Bone Structure (p. 89)
• Compact bone is dense bone tissue found on the outside of all bones. It is covered by the periosteum, a membrane that nourishes the bone cells. Spongy bone is a latticework of tiny, bony beams found in flat bones and near the knobby ends, or heads, of long bones.
• The shaft of an adult long bone has a cavity filled with fatty yellow marrow. The spongy bone of certain bones in adults is filled with red marrow.
Bone as a Living Tissue (pp. 90-91)
• The structural unit of bone, called an osteon, consists of a central canal surrounded by concentric circles made of bone cells (osteocytes) in a hard matrix. Cellular extensions of the osteocytes touch one another through tiny canals in the matrix, allowing exchange of materials between cells and the central canal. Bone matrix is hardened by calcium and phosphorous salts and strengthened by strands of collagen.
• In an embryo, most of the skeleton forms first as cartilage and is gradually replaced by bone. In the replacement process, osteoblasts form a bony collar around the shaft of the cartilaginous model. Next, cartilage within the shaft begins to break down and is replaced by bone, after which the cartilage in the heads (epiphyses) is replaced. Epiphyseal growth plates of cartilage remain and allow bones to grow in length until the person is fully grown.
• Growth hormone from the anterior pituitary gland stimulates bone growth. Sex hormones (estrogen and testosterone) initially stimulate growth, but later they cause the growth plates to disappear, and bones cease to lengthen.
The Role of Fibroblasts and Osteoblasts in Repairing Bone Fractures (p. 91)
• In bone-fracture repair, blood clot formation is followed by a cartilaginous callus that links the broken ends and is gradually replaced by bone.
Bone Remodeling (p. 92)
• Bone is constantly being remodeled. Osteoblasts deposit new bone in response to stress, and osteoclasts break bone down when it is not stressed.
Axial Skeleton (pp. 92-96)
• The skeleton is described as consisting of two parts. One part, the axial skeleton, protects and supports internal organs; it includes the skull, backbone, rib cage, and sternum.
Appendicular Skeleton (p. 97)
• The other part, the appendicular skeleton, allows you to move from place to place; it includes the shoulders, pelvis, arms, and legs.
Joints (pp. 97-100)
• Joints, the places where bones meet, are classified by composition and degree of movement they allow. Some joints, such as the sutures between the skull bones, are considered to be immoveable.
• Synovial joints are freely movable. They have cartilage on the adjoining bone surfaces, are surrounded by a synovial cavity filled with synovial fluid, and are held together by ligaments.
• Damage to a ligament is called a sprain, which is often less serious than the pain.
• Arthritis is inflammation of a joint. Osteoarthritis occurs when the surface of a joint degenerates because of use. Rheumatoid arthritis is an autoimmune disease.
Reviewing the Concepts
1. List six functions of the skeleton. pp. 88-89
2. Compare compact and spongy bone. p. 89
3. Describe the structure of a long bone. Where are the yellow and red marrow found in adults? p. 89
4. Describe the structure of an osteon, and explain the function of osteocytes and the central canal. p. 90
5. Describe the formation of bone in a fetus. Explain how bone growth continues after birth. p. 90
6. Explain how a bone heals after it has been fractured. p. 91
7. What is bone remodeling? Explain the role of osteoblasts and osteoclasts. How does stress on the bones affect remodeling? p. 92
8. Describe the axial and appendicular parts of the skeleton. pp. 92-97
9. Describe a synovial joint. p. 98
10. The functional units of compact bone are called
a. osteoblasts.
b. striations.
c. osteons.
d. osteocytes.
11. Of the following persons, the one you would expect to have the densest bones is
a. an elderly woman whose favorite pastime is knitting.
b. a 16-year-old female who swims regularly.
c. a 33-year-old male who loves to drink milk and plays basketball regularly.
d. a 50-year-old male workaholic with a desk job.
12. The skull, vertebral column, sternum, and rib cage constitute the _____ skeleton.
13. Bone is hardened by the minerals _____ and _____.
14. The cells that form bone are called _____.
15. A _____ is the overstretching or tear in a ligament that may cause pain after the injury.
Applying the Concepts
1. Edith is a 64-year-old woman who has been confined to a wheelchair since she was 35 because of a car accident that left her legs paralyzed. Her leg bones are very thin and weak. Why?
2. Hannah and Becca are fraternal twins. They are both athletic. Hannah is a swimmer, and Becca is a runner. Which sister would have the densest bones?
3. A forensic scientist is examining skeletal remains that include a femur (thighbone) and a tibia (lower leg bone). By measuring the length of the bones, she determines that these leg bones could have belonged to a tall child or a short adult. What should the scientist look for to determine whether the bones were from a child or short adult?
Becoming Information Literate
Mihoko is a 43-year-old woman with osteoporosis. It is uncommon for someone so young to have osteoporosis. Use reliable references to develop a plan for diagnosing the cause(s) of Mihoko's osteoporosis.
Develop a list of hypotheses for the cause. For each hypothesis, formulate a list of information you would need to know to test each hypothesis. What questions would you ask Mihoko? What medical tests would you want to perform? List each source you considered, and explain why you chose the sources you used.