Biology of Humans
4. Body Organization and Homeostasis
In the previous chapter, we learned about cells. This chapter begins by describing the variety of cells and their function. It then describes the body’s organization at four levels: cells, tissues, organs, and organ systems. It looks at the functions of the skin as an organ system and discusses how all the body’s systems interact to maintain relatively constant internal conditions, when they can, at every organizational level.
From Cells to Organ Systems
Think for a moment about the multitude of functions taking place in your body at this very instant. Your heart is beating. Your lungs are taking in oxygen and eliminating carbon dioxide. Your eyes are forming an image of these words, and your brain is thinking about them. Your body can carry out these functions and more because its cells are specialized to perform specific tasks. But cell specialization is only the beginning. Specialized cells are organized into tissues, organs, and organ systems.
Tissues
A tissue is a group of cells of similar type that work together to serve a common function. Human tissues come in four primary types: epithelial tissue, connective tissue, muscle tissue, and nervous tissue. Epithelial tissue covers body surfaces, lines body cavities and organs, and forms glands. Connective tissue serves as a storage site for fat, plays an important role in immunity, and provides the body and its organs with protection and support. Muscle tissue is responsible for body movement and for movement of substances through the body. Nervous tissue conducts nerve impulses from one part of the body to another. As you read this chapter, you learn more about each of these types of tissue.
· Cells are arranged in tissues, and tissues, in turn, form organs. The skin, our largest organ, helps protect underlying tissues and helps to regulate body temperature.
Epithelial tissue. All epithelial tissues share two characteristics: a free surface and a basement membrane. The free surface may be specialized for protection, secretion, or absorption. The basement membrane is a noncellular layer that binds the epithelial cells to underlying connective tissue and helps the epithelial tissue resist stretching.
The three basic shapes of epithelial cells are suited to their functions. Squamous (skway'-mus) epithelium is made up of flattened, or scalelike, cells. These cells form linings—in the blood vessels or lungs, for instance—where their flattened shape allows oxygen and carbon dioxide to diffuse across the lining easily. In blood vessels, the smooth surface of the blood vessel lining reduces friction. Cuboidal epithelium is made up of cube-shaped cells. Cuboidal cells are found in many glands and in the lining of kidney tubules, where they provide some protection and are specialized for secretion and absorption. Columnar epithelium, consisting of elongated, column-shaped cells, is specialized for absorption and secretion. The small intestine is lined with columnar cells. These, like many examples of columnar cells, have numerous small, fingerlike folds on their exposed surfaces, greatly increasing the surface area for absorption. The goblet cells of this lining produce mucus to ease the passage of food and protect the cells of the lining.
Squamous, cuboidal, and columnar epithelium can be either simple (a single layer of cells) or stratified (multiple layers of cells). Stratified epithelium often serves a protective role, because its multiple layers provide additional thickness that makes it more difficult for molecules to pass through. Table 4.1 and Figure 4.1 summarize the types of epithelial tissue.
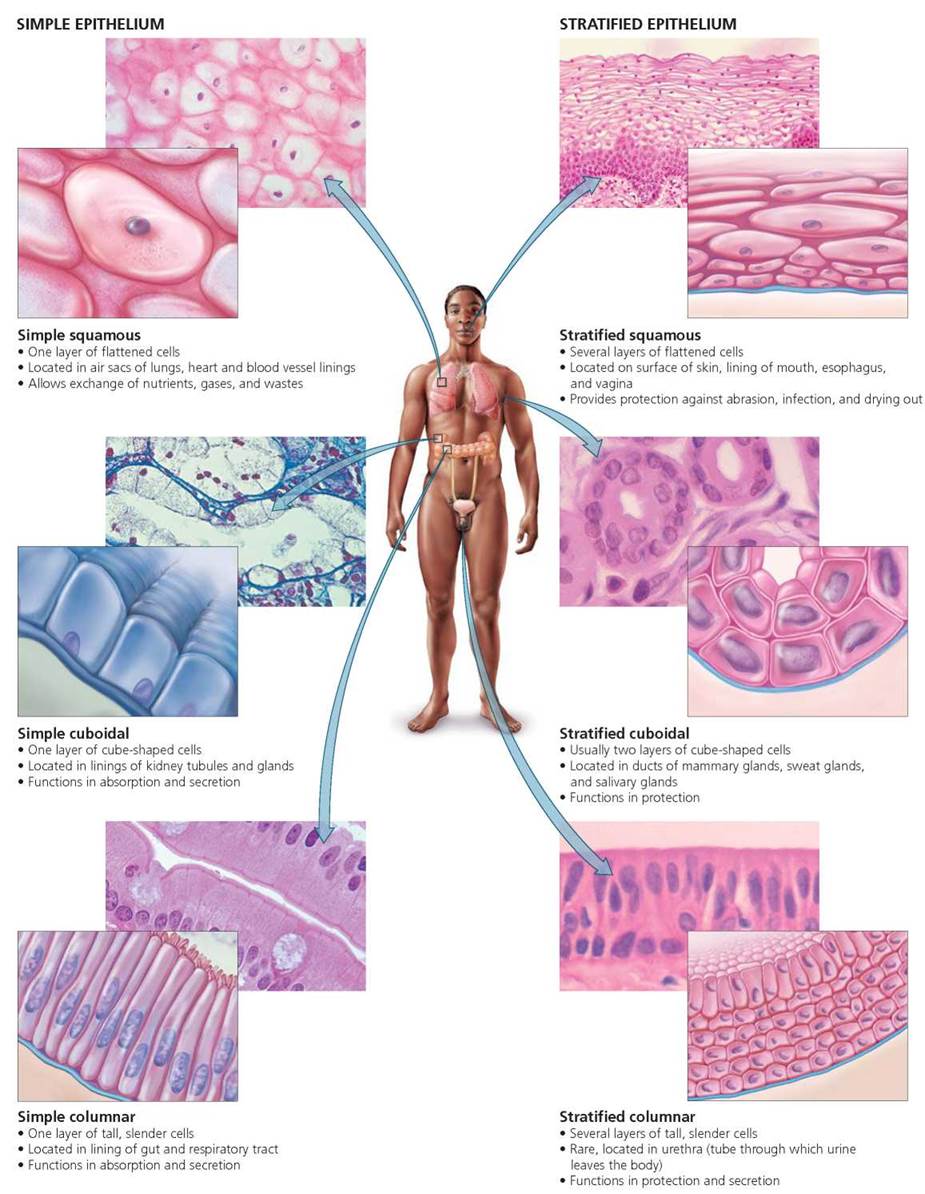
FIGURE 4.1. Types of epithelial tissue. These are named for the shape of the cell and the number of cell layers.
A gland is epithelial tissue that secretes a product. Exocrine glands secrete their products into ducts leading to body surfaces, cavities, or organs. Examples of exocrine glands include the glands that produce digestive enzymes, milk glands, and the oil and sweat glands of the skin. Endocrine glands (covered in more depth in Chapter 10) lack ducts and secrete their products, hormones, into spaces just outside the cells. Ultimately, hormones diffuse into the bloodstream and are carried throughout the body.
TABLE 4.1. Review of Epithelial Tissue
Shape |
Number of Layers |
Example Locations |
Functions |
Squamous (flat, scalelike cells) |
Simple (single layer) |
Lining of heart and blood vessels, air sacs of lungs |
Allows passage of materials by diffusion |
Stratified (more than one layer) |
Linings of mouth, esophagus, and vagina; outer layer of skin |
Protects underlying areas |
|
Cuboidal (cubeshaped cells) |
Simple |
Kidney tubules, secretory portion of glands and their ducts |
Secretes; absorbs |
Stratified |
Ducts of sweat glands, mammary glands, and salivary glands |
Protects underlying areas |
|
Columnar |
Simple |
Most of digestive tract (stomach to anus), air tubes of lungs (bronchi), excretory ducts of some glands, uterus |
Absorbs; secretes mucus, enzymes, and other substances |
Stratified |
Rare; urethra, junction of esophagus and stomach |
Protects underlying areas, secretes |
Connective tissue. Connective tissue has many forms and functions. Sometimes described as the body's glue, its most common role is to bind (tendons and ligaments) and support the other tissues (cartilage and bone). However, certain connective tissues specialize in transport (blood) and energy storage (adipose tissue). Connective tissue is the most abundant and widely distributed tissue in the body.
All connective tissues contain cells embedded in an extracellular matrix. This matrix consists of protein fibers and a noncellular material called ground substance. The ground substance may be solid (as in bone), fluid (as in blood), or gelatinous (as in cartilage). It is secreted by the connective tissue cells themselves or by other cells nearby. Whereas all other types of tissue consist primarily of cells, connective tissue is made up mostly of its matrix. The cells are distributed in the matrix much like pieces of fruit suspended in a gelatin dessert.
The connective-tissue matrix contains three types of protein fibers in proportions that depend on the type of connective tissue. Collagen fibers are strong and ropelike and can withstand pulling because of their great tensile strength. Elastic fibers contain random coils and can stretch and recoil like a spring. They are common in structures where great elasticity is needed, including the skin, lungs, and blood vessels. Reticular fibers are thin strands of collagen1 that branch extensively, forming interconnecting networks suitable for supporting soft tissues (for example, they support the liver and spleen).
All three types of protein fibers—collagen, elastic, and reticular—are produced by cells called fibroblasts in the connective tissue. Fibroblasts also repair tears in body tissues. For example, when skin is cut, fibroblasts move to the area of the wound and produce collagen fibers that help close the wound, cover the damage, and provide a surface upon which the outer layer of skin can grow back.
There are two broad categories of connective tissue— connective tissue proper (loose and dense connective tissue) and specialized connective tissue (cartilage, bone, and blood). Table 4.2 and Figure 4.2 group the many types of connective tissue and summarize the characteristics of each type. The characteristics of any specific connective tissue are determined more by its matrix than by its cells.
Connective Tissue Proper. Loose and dense connective tissues differ in the ratio of cells to extracellular fibers. Loose connective tissue contains many cells but has fewer and more loosely woven fibers than are seen in the matrix of dense connective tissue (Figure 4.2). One type of loose connective tissue, areolar (ah-ree'-o-lar) connective tissue, functions as a universal packing material between other tissues. Its many cells are embedded in a gelatinous matrix that is soft and easily shaped. Areolar connective tissue is found, for example, between muscles, where it permits one muscle to move freely over another. It also anchors the skin to underlying tissues and organs.
TABLE 4.2. Review of Connective Tissue
Type |
Example Locations |
Functions |
Connective tissue proper |
||
Loose, areolar |
Between muscles, surrounding glands, wrapping small blood vessels and nerves |
Wraps and cushions organs |
Loose, adipose (fat) |
Under skin, around kidneys and heart |
Stores energy, insulates, cushions organs |
Dense |
Tendons, ligaments |
Attaches bone to bone (ligaments) or bone to muscle (tendons) |
Specialized connective tissue |
||
Cartilage (semisolid) |
Nose (tip); rings in respiratory air tubules; external ear |
Provides flexible support, cushions |
Bone (solid) |
Skeleton |
Provides support and protection (by enclosing) and levers for muscles to act on |
Blood (fluid) |
Within blood vessels |
Transports oxygen and carbon dioxide, nutrients, hormones, and wastes; helps fight infections |
The second type of loose connective tissue is adipose (ad-e'-pos) tissue;it contains cells that are specialized for fat storage. Most of the body's long-term energy stores are fat. Fat also serves as insulation and, around certain organs, as a shock absorber.
Dense connective tissue forms strong bands because of its large amounts of tightly woven fibers. It is found in ligaments (structures that join bone to bone), tendons (structures that join muscle to bone), and the dermis (layer of skin below the epidermis).
Specialized Connective Tissue. Specialized connective tissue, as shown in Figure 4.2, comes in three types: cartilage, bone, and blood. Cartilage (kar'tl-ij) is tough but flexible. It serves as cushioning between certain bones and helps maintain the structure of certain body parts, including the ears and the nose. The cells in cartilage (chondrocytes) sit within spaces in the matrix called lacunae. The protein fibers and somewhat gelatinous ground substance of cartilage are responsible for the tissue's resilience and strength. Cartilage lacks blood vessels and nerves, so nutrients reach cartilage cells by diffusion from nearby capillaries. Because this process is fairly slow, cartilage heals more slowly than bone, which is a tissue with a rich blood supply.
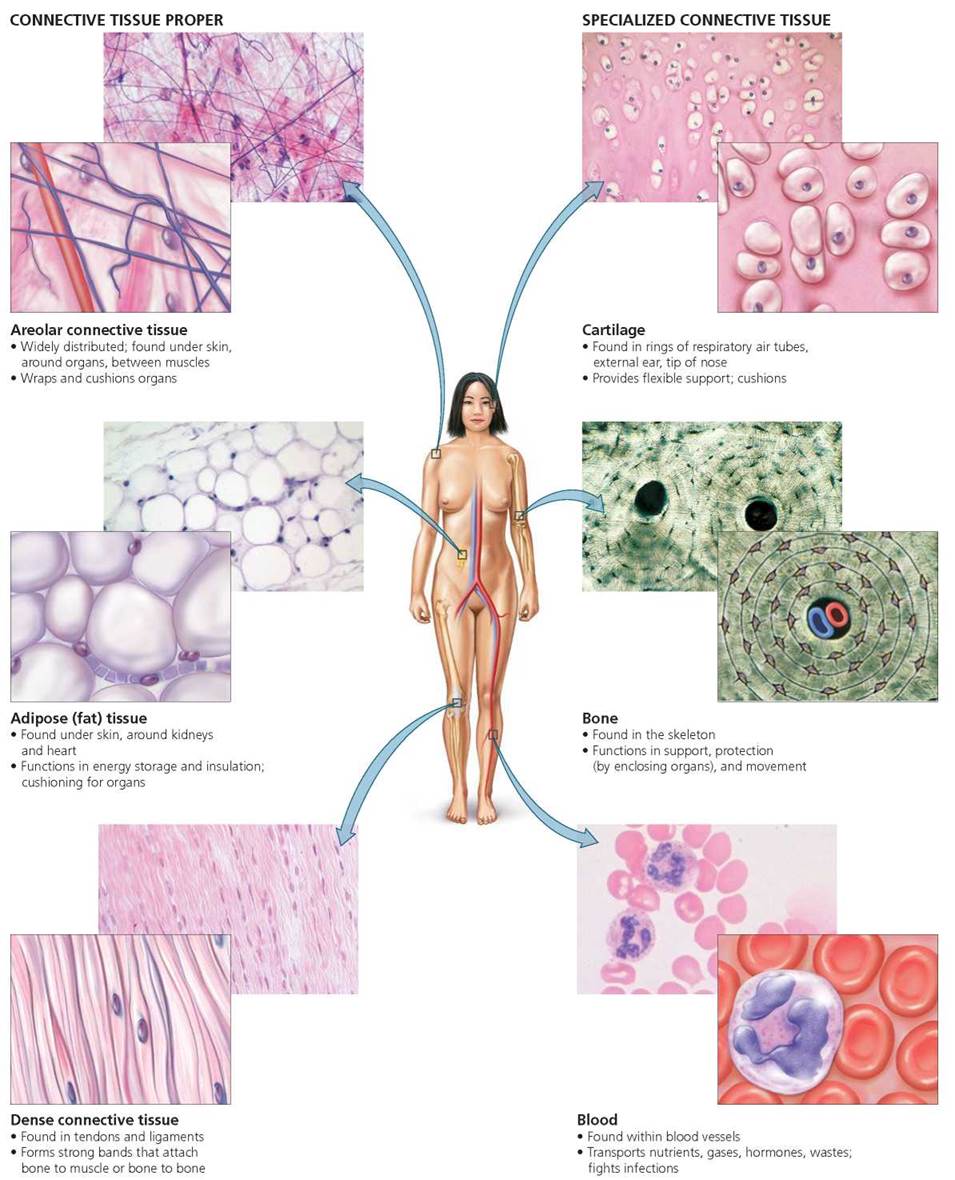
FIGURE 4.2. Types of connective tissue
The human body has three types of cartilage:
• Hyaline cartilage, the most abundant, provides support and flexibility. It contains numerous cartilage cells in a matrix of collagen fibers and a bluish white, gel-like ground substance. Known commonly as gristle, hyaline cartilage is found at the ends of long bones (look carefully at your next drumstick), where it allows one bone to slide easily over another. It also forms part of the nose, ribs, larynx, and trachea.
• Elastic cartilage is more flexible than hyaline cartilage because of the large amounts of wavy elastic fibers in its matrix. Elastic cartilage is found in the external ear, where it provides strength and elasticity.
• Fibrocartilage contains fewer cells than either hyaline or elastic cartilage. Like hyaline cartilage, its matrix contains collagen fibers. Fibrocartilage forms a cushioning layer in the knee joint as well as the outer part of the shockabsorbing disks between the vertebrae of the spine. It is made to withstand pressure.
Bone, in combination with cartilage and other components of joints, makes up the skeletal system. To many people's surprise, bone is a living, actively metabolizing tissue with a good blood supply that promotes prompt healing. Bone has many functions: protection and support for internal structures; movement, in conjunction with muscles; storage of lipids (in yellow marrow), calcium, and phosphorus; and production of blood cells (in red marrow). The matrix secreted by bone cells is hardened by calcium, enabling bones to provide rigid support. Collagen fibers in bone also lend it strength. You will read more about the structure and function of bones in Chapter 5.
Blood is a specialized connective tissue consisting of a liquid matrix, called plasma, in which so-called formed elements (cells and cell fragments called platelets) are suspended (Figure 4.2). The "fibers" in blood are soluble proteins, visible only when the blood clots. An important function of blood is to transport various substances, many of which are dissolved in the plasma. One kind of formed element, the red blood cell, transports oxygen to cells and also carries some of the carbon dioxide away from cells. The other two kinds of formed elements are white blood cells, which help fight infection, and platelets, which help with clotting. Both white blood cells and platelets help protect the body. You will read more about blood in Chapter 11.
Muscle tissue Muscle tissue is composed of muscle cells (called muscle fibers) that contract when stimulated. As shown in Figure 4.3, there are three types of muscle tissue: skeletal, cardiac, and smooth. Their characteristics are summarized in Table 4.3. You will read more about muscle tissue in Chapters 6 and 12.
TABLE 4.3. Review of Muscle Tissue
Type |
Description |
Example Locations |
Functions |
Skeletal |
Long, cylindrical cells; multiple nuclei per cell; obvious striations |
Muscles attached to bones |
Provides voluntary movement |
Cardiac |
Branching, striated cells; one nucleus; specialized junctions between cells |
Wall of heart |
Contracts and propels blood through the circulatory system |
Smooth |
Cells taper at each end; single nucleus; arranged in sheets; no striations |
Walls of digestive system, blood vessels, and tubules of urinary system |
Propels substances or objects through internal passageways |
• Skeletal muscle tissue is so named because it is usually attached to bones. When skeletal muscle tissue contracts, therefore, it usually moves a part of the body. Because skeletal muscle is under conscious control, it is described as voluntary muscle. Skeletal muscle cells are long, cylindershaped cells, each containing several nuclei. In addition, skeletal muscle cells have striations, which are alternating light and dark bands visible under a light microscope. The striations are caused by the orderly arrangement of the contractile proteins actin and myosin, which interact to cause muscle contraction.
• Cardiac muscle tissue is found only in the walls of the heart, where its contractions are responsible for pumping blood to the rest of the body. Cardiac muscle contractions are not under conscious control; we cannot make them contract by thinking about them. Thus, cardiac muscle is considered involuntary muscle. Cardiac muscle cells resemble branching cylinders and have striations and typically only one nucleus. Special junctions at the plasma membranes of these cells strengthen cardiac tissue and promote rapid conduction of impulses throughout the heart.
• Smooth muscle tissue is involuntary and is found in the walls of blood vessels and airways, where its contraction reduces the flow of blood or air. Smooth muscle is also found in the walls of organs such as the stomach, intestines, and bladder, where it aids in mixing and propelling food through the digestive tract and in eliminating wastes. The cells of smooth muscle tissue taper at each end, contain a single nucleus, and lack striations.
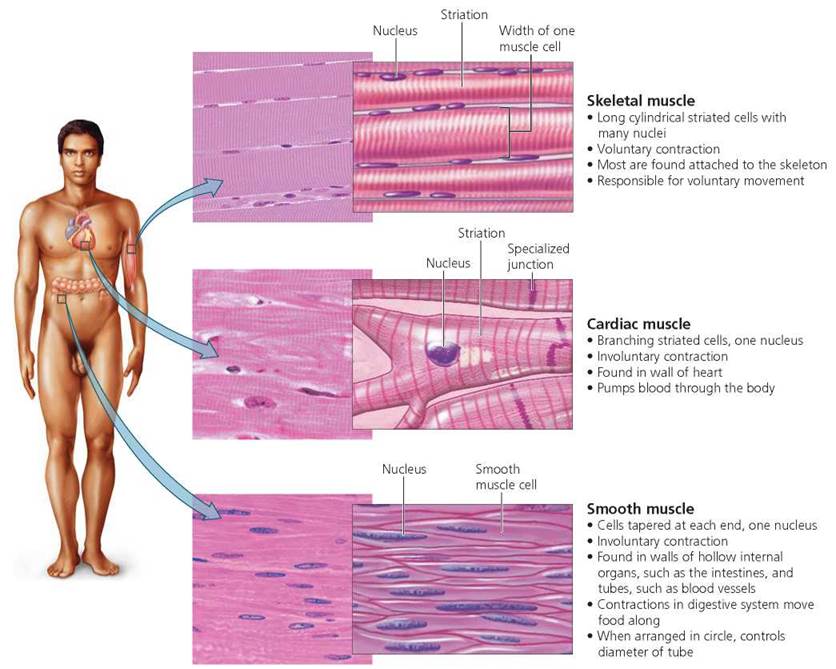
FIGURE 4.3. Types of muscle tissue
Nervous tissue. The final major type of tissue, nervous tissue, makes up the nervous system: brain, spinal cord, and nerves. Nervous tissue consists of two general cell types, neurons and accessory cells called neuroglia (Figure 4.4). Neurons generate and conduct nerve impulses, which they conduct to other neurons, muscle cells, or glands. Although neurons come in many shapes and sizes, most have three parts—the cell body, dendrites, and an axon. The cell body houses the nucleus and most organelles. Dendrites are highly branched processes that provide a large surface area for the reception of signals from other neurons. A neuron generally has one axon, a long extension that usually conducts impulses away from the cell body. Far more numerous than neurons, the neuroglia (or more simply, glial cells) support, insulate, and protect neurons. They increase the rate at which impulses are conducted by neurons and provide neurons with nutrients from nearby blood vessels. Recent studies indicate that glial cells communicate with one another and with neurons. You will read more about nervous tissue in Chapters 7 and 8.
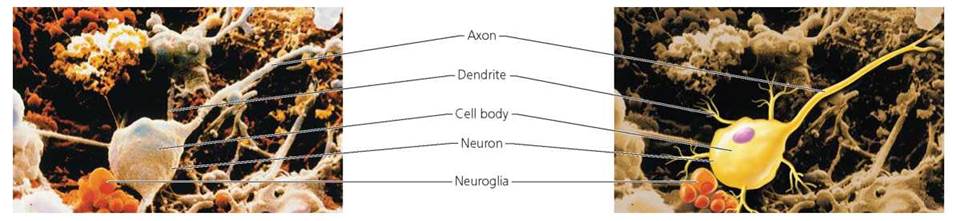
FIGURE 4.4. Neurons and neuroglia
Cell Junctions
In many tissues, especially epithelial tissue, the cell membranes have structures for forming attachments between adjoining cells. There are three kinds of junctions between cells: tight junctions, adhesion junctions, and gap junctions. Each type of junction suits the function of the tissue. In tight junctions (Figure 4.5a), the membranes of neighboring cells are attached so securely that they form a leakproof seal. Tight junctions are found in the linings of the urinary tract and intestines, where secure seals between cells prevent urine or digestive juices from passing through the epithelium. Less rigid than tight junctions, adhesion junctions (also called desmosomes; Figure 4.5b) resemble rivets holding adjacent tissue layers together. The plasma membranes of adjacent cells do not actually touch but are instead bound together by intercellular filaments attached to a thickening in the membrane. Thus, the cells are connected but can still slide slightly relative to one another. Adhesion junctions are common in tissues that must withstand stretching, such as the skin and heart muscle. Gap junctions (Figure 4.5c) connect the cytoplasm of adjacent cells through small holes, allowing certain small molecules and ions to flow directly from one cell into the next. In heart and smooth muscle cells, gap junctions help synchronize electrical activity and thus contraction.
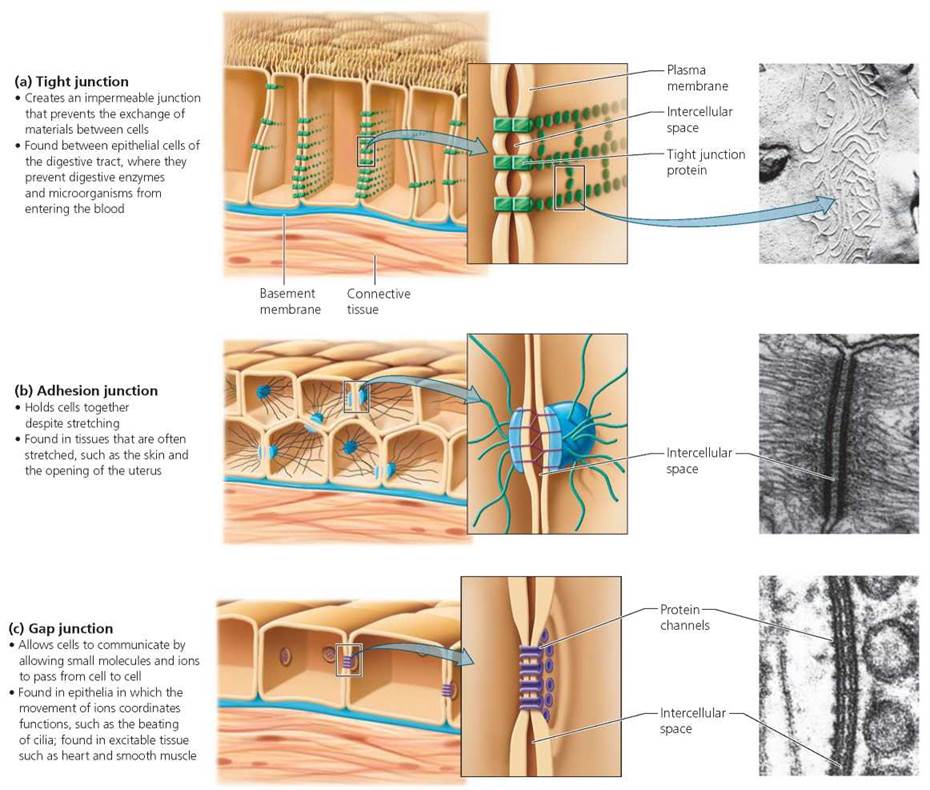
FIGURE 4.5. Specialized cell junctions
Organs and Organ Systems
An organ is a structure composed of two or more different tissues that work together to perform a specific function. Organs themselves do not usually function as independent units but instead form part of an organ system—a group of organs with a common function. For example, organs such as the trachea, bronchi, and lungs constitute the respiratory system. The common function of these organs is to bring oxygen into the body and remove carbon dioxide. The human body includes the 11 major organ systems.
Body Cavities Lined with Membranes
Most of our organs are suspended in internal body cavities. These cavities have two important functions. First, they help protect the vital organs from being damaged when we walk or jump. Second, they allow organs to slide past one another and change shape. Sliding and changing shape are important when the lungs fill with air, the stomach fills with food, the urinary bladder fills with urine, or when our bodies bend or stretch.
There are two main body cavities—the ventral and dorsal cavities—each of which is further subdivided. The ventral (toward the abdomen) cavity is divided into the thoracic (chest) cavity and the abdominal cavity. The thoracic cavity is subdivided again into the pleural cavities, which house the lungs, and the pericardial cavity, which holds the heart. The abdominal cavity contains the digestive system, the urinary system, and the reproductive system. A muscle sheet called the diaphragm separates the thoracic and abdominal cavities. The dorsal (toward the back) cavity is subdivided into the cranial cavity, which encloses the brain, and the spinal cavity, which houses the spinal cord.
Body cavities and organ surfaces are covered with membranes—sheets of epithelium supported by connective tissue. Membranes form physical barriers that protect underlying tissues. The body has four types of membrane.
1. Mucous membranes line passageways that open to the exterior of the body, such as those of the respiratory, digestive, reproductive, and urinary systems. Some mucous membranes, including the mucous membrane of the small intestine, are specialized for absorption. Others, like those of the respiratory system, for instance, secrete mucus that traps bacteria and viruses that could cause illness.
2. Serous membranes line the thoracic and abdominal cavities and the organs within them. They secrete a fluid that lubricates the organs within these cavities.
3. Synovial membranes line the cavities of freely movable joints, such as the knee. These membranes secrete a fluid that lubricates the joint, easing movement.
4. Cutaneous membrane, or skin, covers the outside of the body. Unlike other membranes, it is thick, relatively waterproof, and relatively dry.
The body cavities of the human body are shown in Figure 4.6. We will consider the structure and function of the skin in the next section. Details about the structure and functions of the other organ systems, shown and described in Figure 4.7, are presented in subsequent chapters.
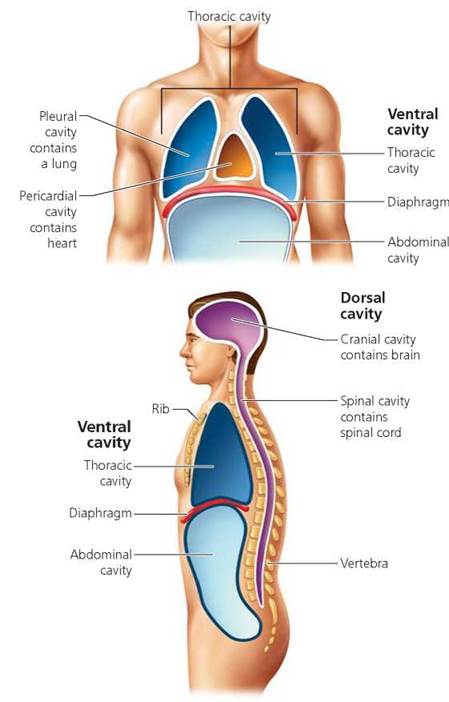
FIGURE 4.6. Body cavities. The internal organs are suspended in body cavities that protect the organs and allow organs to slide past one another as the body moves. Ventral means “toward the abdomen," and dorsal means “toward the back."
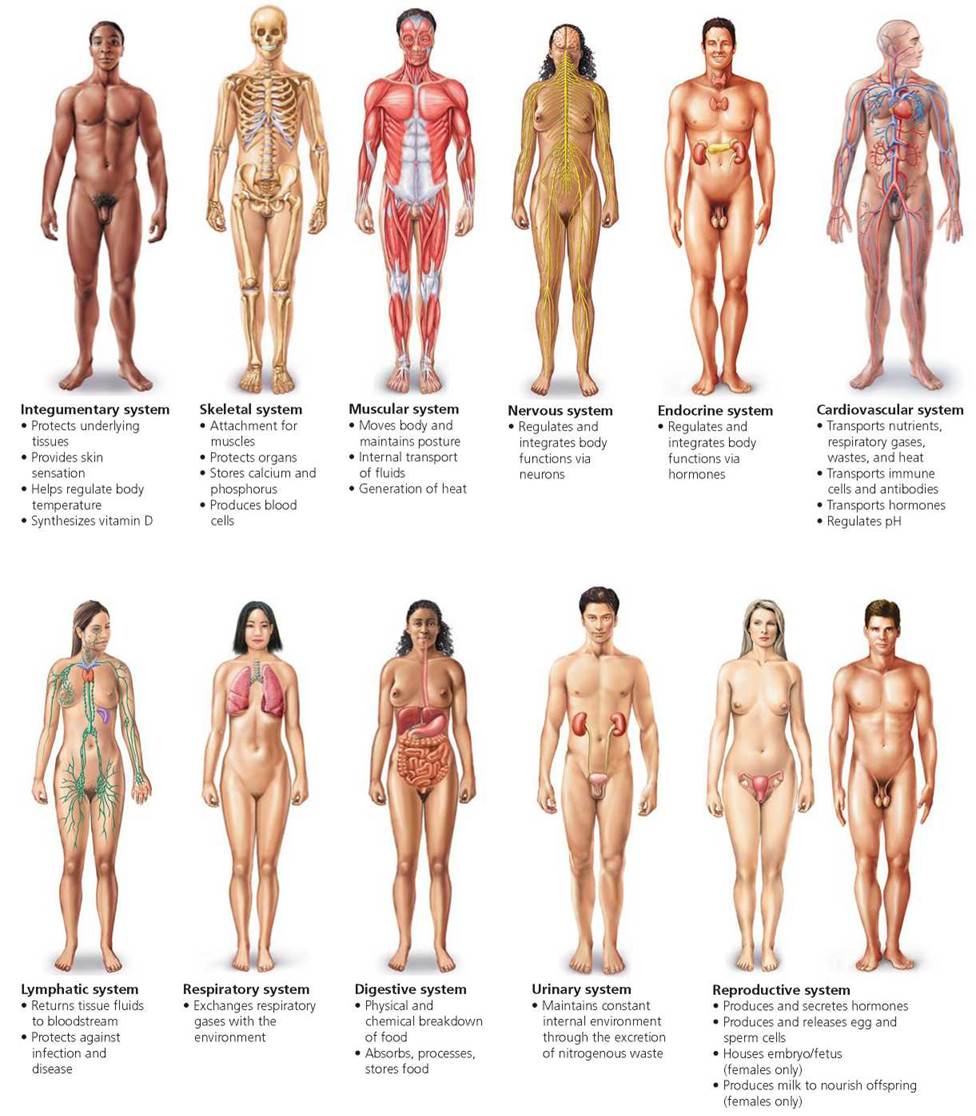
FIGURE 4.7. Major organ systems of the human body
________________________________________________________________
1 Reticular fibers have the same subunits as collagen fibers, but they are assembled into a slightly different kind of structure.
Skin: An Organ System
We have all been told that "beauty is only skin deep," but our skin does much more than just make us attractive. The skin and its derivatives—hair, nails, sweat glands, and oil glands— are sometimes called the integumentary system (an integument is an outer covering). It is considered an organ system because the skin and its derivatives function together to provide many services for the body.
Skin Functions
A major function of our skin is protection. It serves as a physical barrier that shields the contents of the body from invasion by foreign bacteria and other harmful particles, from ultraviolet (UV) radiation, and from physical and chemical insult. Besides offering this somewhat passive form of protection, skin contains cells called macrophages that have a more active way of fighting infection, as we will see in Chapter 13.
The skin has many other functions, as well. For example, because its outermost layer of cells contains the water- resistant protein keratin, the skin plays a vital role in preventing excessive water loss from underlying tissues. It plays a role in temperature regulation, too. Although we perspire (imperceptively) through our skin almost constantly, during times of strenuous exercise or high environmental temperatures our sweat glands become active and increase their output of perspiration dramatically. The evaporation of this perspiration from the skin's surface helps rid the body of excess heat. Later we will see how changes in the flow of blood to the skin help regulate body temperature. The skin even functions in the production of vitamin D. Modified cholesterol molecules in the skin's outer layer are converted to vitamin D by UV radiation. The vitamin D then travels in the bloodstream to the liver and kidneys, where it is chemically modified to assume its role in stimulating the absorption of calcium and phosphorus from the food we eat.
In addition, the skin contains structures for detecting temperature, touch, pressure, and pain stimuli. These receptors—components of the nervous system—help keep us informed about conditions in our external environment. Keep these many functions of the integumentary system in mind as you read on about the structure of the skin and its derivatives.
Skin Layers
On most parts of your body, the skin is less than 5 mm (less than a quarter of an inch) thick, yet it is one of your largest organs. It represents about one-twelfth of your body weight and has a surface area of 1.5 to 2 m2 (1.8 to 2.4 yd2).
The skin has two principal layers, as shown in Figure 4.8. The thin, outer layer, the epidermis, forms a protective barrier against environmental hazards. The inner layer, the dermis, contains blood vessels, nerves, sweat and oil glands, and hair follicles. Beneath the skin is a layer of loose connective tissue called the hypodermis or subcutaneous layer, which anchors the skin to the tissues of other organ systems that lie beneath.

FIGURE 4.8. Structures of the skin and underlying hypodermis
The epidermis. The outermost layer of skin, the epidermis, is itself composed of several layers of epithelial cells. The outer surface of epidermis, the part you can touch, is made up of dead skin cells. Thus, when we look at another person, most of what we see on the person's surface is dead. These dead cells are constantly being shed, at a rate of about 30,000 to 40,000 each minute. In fact, much of the dust in any room consists of dead skin cells. When you go swimming or soak in the bathtub for a long time, the dead cells on your skin's surface absorb water and swell, causing the skin to wrinkle. This is particularly noticeable where the layer of dead cells is thickest, such as on the palms of the hands and soles of the feet.
The skin does not get thinner as the dead cells are shed, because they are continuously replaced from below. The deepest layer of epidermis contains rapidly dividing cells. As new cells are produced in this layer, older cells are pushed toward the surface. On their way, they flatten and die because they no longer receive nourishment from the dermis. Along this death route, keratin—a tough, fibrous protein—gradually replaces the cytoplasmic contents of the cells. It is keratin that gives the epidermis its protective properties. About 2 weeks to a month pass from the time a new cell is formed to the time it is shed.
Drugs that must be continuously administered are often given across the skin (transdermally) using a drug-containing patch that adheres to the skin (Figure 4.9). Although the epidermis is a water-resistant protective barrier, lipid-soluble materials are able to cross the lipid cell membranes of the cells of the epidermis. Thus, if you dissolve a drug in a lipid solvent, it can cross the epidermis, diffuse into the underlying connective tissue, and be absorbed into the blood. Today, transdermal drug administration is commonly used to provide hormones for birth control or the treatment of menopausal symptoms, nicotine to ease the urge to smoke while trying to quit, and antiemetics to stop nausea from motion sickness.

FIGURE 4.9. A transdermal patch continuously delivers a drug across the skin. Here, a cigarette smoker uses a nicotine patch to help quit smoking.
What would you do?
To speed up the movement of a drug from a transdermal patch to the patient's blood supply, the patch is prepared with a higher concentration of the drug than would be found in a pill.
In transdermal patches that deliver hormones for birth control, the blood levels of hormones may also be higher than would result with birth control pills. During the last few years, several young women using a transdermal patch for birth control have had heart attacks or strokes; some have died. There are warning labels with contraceptive patches informing women of these increased risks. Do you think that women or their families should be able to sue the patch manufacturer for their losses?
The dermis. Over most parts of the body, the dermis is a much thicker layer than the epidermis. The dermis lies just beneath the epidermis and consists primarily of connective tissue. In addition, it contains blood vessels, hair follicles, oil glands, the ducts of sweat glands, sensory structures, and nerve endings. Unlike the epidermis, the dermis does not wear away. This durability explains why tattoos—designs created when tiny droplets of ink are injected into the dermal layer—are permanent (Figure 4.10). Because the dermis is laced with nerves and sensory receptors, getting a tattoo hurts. In the past, the only way to remove a tattoo was by surgical means, such as "shaving" (abrading) of the skin. Today, laser treatments that destroy the pigments of the tattoo can often be used for tattoo removal.
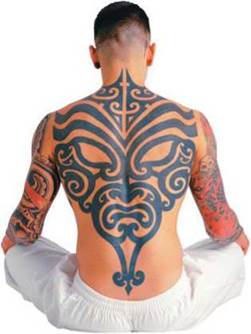
FIGURE 4.10. Tattoos—designs created when droplets of ink are injected into the dermis—are essentially permanent because, unlike the epidermis, the dermis is not shed.
Blood vessels are present in the dermis but not in the epidermis. Nutrients reach the epidermis by passing out of dermal blood vessels and diffusing through tissue fluid into the layer above. Such tissue fluid is probably quite familiar to you. Where skin is traumatized by, for example, a burn or an ill-fitting shoe rubbing against your heel, this fluid accumulates between the epidermis and dermis, separating the layers and forming blisters.
Stop and think
Burns—tissue damage caused by heat, radiation, electric shock, or chemicals—can be classified according to how deep the damage penetrates. First-degree burns are confined to the upper layers of epidermis, where they cause reddening and slight swelling. In second-degree burns, damage extends through the epidermis into the upper regions of the dermis. Blistering, pain, and swelling occur. Third-degree burns extend through the epidermis and dermis into underlying tissues. Severe burns, particularly if they cover large portions of the body, are life threatening. Given your knowledge of skin functions, what would you predict the immediate medical concerns to be when a patient has third-degree burns?
The lower layer of the dermis consists of dense connective tissue containing collagen and elastic fibers, a combination that allows the skin to stretch and then return to its original shape. The resilience of our skin also decreases as we age. The most pronounced effects begin in the late forties, when collagen fibers begin to stiffen and decrease in number and elastic fibers thicken and lose elasticity. These changes, combined with reductions in moisture and the amount of fat in the hypodermis, lead to wrinkles and sagging skin.
Certain wrinkles, such as frown lines, are caused by the contraction of facial muscles. A controversial and popular treatment for these wrinkles is to inject Botox, the toxin from the bacterium that causes botulism. When Botox is injected into facial muscles, they become temporarily paralyzed. The muscle contractions that form the wrinkles cannot occur, and the skin smoothes out. The muscles regain the ability to contract over the next several months, however, and the injection has to be repeated (Figure 4.11).

FIGURE 4.11. Before and after Botox injections
The hypodermis. The hypodermis, a layer of loose connective tissue just below the epidermis and dermis, is not usually considered part of the skin. It does, however, share some of the skin's functions, including cushioning blows and helping to prevent extreme changes in body temperature, because it contains about half of the body's fat stores. In infants and toddlers, this layer of fat that lies under the skin—often called baby fat—covers the entire body, but as we mature, some of the fat stores are redistributed. In women, subcutaneous fat tends to accumulate in the breasts, hips, and thighs. In both sexes, it has a tendency to accumulate in the abdominal hypodermis, contributing to the all-too-familiar potbelly, and in the sides of the lower back, forming "love handles."
Liposuction, a procedure for vacuuming fat from the hypodermis, is a way to reshape the body. The physician makes a small incision in the skin above the area of unwanted fat, inserts a fine tube, and moves the tube back and forth to loosen the fat cells, which are then sucked into a container. Liposuction is not a way of losing a lot of weight, because only a small amount of fat—not more than a few pounds—can be removed. However, it is a way of sculpting the body and removing bulges. Furthermore, because liposuction removes the cells that store the fat, fat does not usually return to those areas. The procedure is generally safe, but it is not risk free. In some patients, it has produced blood clots that traveled to the lungs, causing death. People who are considering liposuction should choose their doctor carefully.
What would you do?
Proponents claim that Lipodissolve is an effective, nonsurgical treatment for destroying unwanted pockets of fat. The treatment consists of a series of injections containing two main ingredients: one that chemically digests fat molecules and another that causes fat cells to burst. Although FDA has approved both drugs for other purposes, it has not approved this procedure combining the drugs for the purpose of eliminating unwanted fat. There is no evidence that Lipodissolve is unsafe, and there is no scientific evidence that it is effective. Do you think Lipodissolve should be illegal for this purpose? How important to you is FDA approval for a procedure?
Skin Color
Two interacting factors produce skin color: (1) the quantity and distribution of pigment and (2) blood flow. The pigment, called melanin, is produced by cells called melanocytes at the base of the epidermis. These cells, with their spiderlike extensions, produce two kinds of melanin: a yellow-to-red form and the more common black-to-brown form. The melanin is then taken up by surrounding epidermal cells, thus coloring the entire epidermis.
All people have about the same number of melanocytes. Differences in skin color are due to differences in the form of melanin produced and the size and number of pigment granules. A person's genetic makeup determines the combination of the yellowish red or the brown form of melanin produced.
Circulation also influences skin color. When well-oxygenated blood flows through vessels in the dermis, the skin has a pinkish or reddish tint that is most easily seen in lightskinned people. Intense embarrassment can increase the blood flow, causing the rosy color to heighten, particularly in the face and neck. This response, known as blushing, is impossible to stop. Other intense emotions may cause color to disappear temporarily from the skin. A sudden fright, for example, can cause a rapid drop in blood supply, making a person pale. Skin color may also change in response to changing levels of oxygen in the blood. Compared to well-oxygenated blood, which is ruby red, poorly oxygenated blood is a much deeper red that gives the skin a bluish appearance. Poor oxygenation is why the lips appear blue in extremely cold conditions. When it is cold, your body shunts blood away from the skin to the body's core, which conserves heat and keeps vital organs warm. This shunting reduces the oxygen supply to the blood in the small vessels near the surface of the skin. The oxygen-poor blood seen through the thin skin of the lips makes them look blue. When you do not get enough sleep, the amount of oxygen in your blood may be slightly lower than usual, causing the color to darken. In some people, the darker color of blood is visible through the thin skin under their eyes as dark circles.
Tanning is a change in skin color from exposure to the sun. Melanocytes respond to the UV radiation in sunlight by increasing the production of melanin. This is a protective response, because melanin absorbs some UV radiation, preventing it from reaching the lower epidermis and the dermis. The skin requires some UV radiation for the production of vitamin D, but too much can be harmful. See the Health Issue essay, Fun in the Sun?.
Hair, Nails, and Glands
The epidermis gives rise to many seemingly diverse structures: hair, nails, oil glands, sweat glands, and teeth. We will now consider the first four of these in view of their structure and roles in everyday life. (Teeth are discussed in Chapter 15.)
Hair Hair usually grows all over the body, except on a few areas such as the lips, palms of the hands, and soles of the feet. What functions do these dead cells serve? An important one is protection. Hair on the scalp protects the head from UV radiation. Hair in the nostrils and external ear canals keeps particles and bugs from entering. Likewise, eyebrows and eyelashes help keep unwanted particles and glare (and perspiration and rain) out of the eyes. Hair also has a sensory role: receptors associated with hair follicles are sensitive to touch.
A hair consists of a shaft and a root (see Figure 4.8). The shaft projects above the surface of the skin, and the root extends below the surface into the dermis or hypodermis, where it is embedded in a structure called the hair follicle. Nerve endings surround the follicle and are so sensitive to touch that we are aware of even slight movements of the hair shaft. (Try to move just one hair without feeling it.) Each hair is also supplied with an oil gland that opens onto the follicle and supplies the hair with an oily secretion that makes it soft and pliant. In the dermis, a tiny smooth muscle called the arrector pili is attached to the hair follicle. Contraction of this muscle—which pulls on the follicle, causing the hair to stand up—is associated with fear and with cold. The tiny mound of flesh that forms at the base of the erect hair is sometimes called a goose bump.
Health Issue
Fun in the Sun?
A beach crowded with people on a sunny day is hardly a scene we would equate with disfigurement and death. Nonetheless, that is a connection we should make, because skin cancers are increasing at an alarming rate, largely due to our exposure to the sun.
The ultraviolet (UV) radiation of sunlight causes the melanocytes of the skin to increase their production of the pigment melanin, which absorbs UV radiation before it can damage the genetic information of deeper layers of cells.
Unfortunately, this protective buildup of melanin is not instantaneous. In skin cancer, the genetic material in skin cells is altered by UV radiation so that the cells grow and divide uncontrollably, forming a tumor. Some experts fear that the rates of skin cancer will increase dramatically if the ozone layer, which blocks some of the UV radiation before it reaches Earth, continues to become thinner (the ozone layer is discussed in Chapter 24). Three types of skin cancer are caused by overexposure to the sun (Figure 4.A):
• Basal cell carcinoma, the most common form of skin cancer, arises in the rapidly dividing cells of the deepest layer of epidermis.
• Squamous cell carcinoma, the second most common form of skin cancer, arises in the newly formed skin cells as they flatten and move toward the skin surface.
• Melanoma is the least common and most dangerous type of skin cancer. It arises in melanocytes, the pigment-producing cells of the skin. Unlike basal or squamous cell carcinomas, melanomas, when left untreated, often metastasize (spread rapidly) throughout the body, first infiltrating the lymph nodes and later the vital organs. The survival rate in persons whose melanoma is found before it has metastasized is about 90% but drops to about 14% if the cancerous cells have spread throughout the body.
You can catch melanomas at an early stage if you carefully examine your skin while applying the ABCD mnemonic of the American Cancer Society:
A—stands for asymmetry. Most melanomas are irregular in shape.
B—stands for border. Melanomas often have a diffuse, unclear border.
C—stands for color. Melanomas usually have a mottled appearance and contain colors such as brown, black, red, white, and blue.
D—stands for diameter. Growths with a diameter of more than 5 mm (about 0.2 in.) are threatening.
The best way to avoid getting skin cancer is to avoid prolonged exposure to the sun. If you must be out in the sun, wear a hat, long sleeves, and sunglasses. Use a sunscreen with a sun protection factor (SPF) of at least 15. Apply your sunscreen about 45 minutes before going out into the sun, allowing time for it to be absorbed by the skin so that it is less likely to wash away with perspiration. Use sunscreen even when it is overcast, because UV rays can penetrate the clouds. Reapply it after swimming.
Always remember that sunscreens are not foolproof. Most block the higher-energy portion of the sun's UV radiation, known as UV-B, while providing only limited protection against the lower-energy portion, called UV-A. Whereas UV-B causes skin to burn, recent research suggests that exposure to UV-A weakens the body's immune system, possibly impairing its ability to fight melanoma. Ironically, by providing protection from sunburn, sunscreens have had the potentially devastating effect of enabling people to spend more time in the sun, possibly increasing their risk of developing melanoma.
Avoid tanning salons. For many years, tanning salons claimed to use “safe” wavelengths of UV radiation because they did not use skinreddening UV-B. But these “safe” wavelengths are actually UV-A. Given the apparent link between UV-A and increased risk of melanoma, the potential danger of these “safe” wavelengths is now obvious.
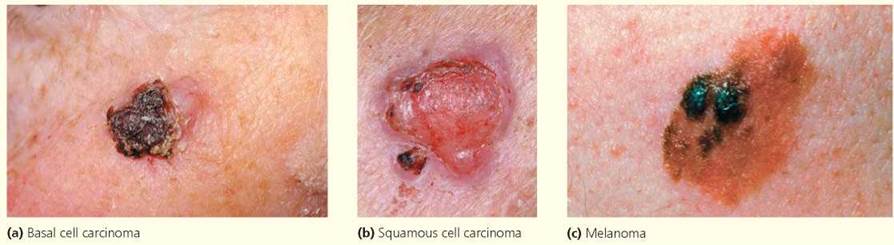
FIGURE 4.A. Three skin cancers
Questions to Consider
• Do you think that tanning salons should be required to explain the dangers of UV-A to the public?
• Some physicians are now warning that excessive use of sunscreen can lower the body's ability to produce enough vitamin D, which can lead to osteoporosis (a loss of bone density). What steps might you take to balance the risk of developing skin cancer with the risk of vitamin D deficiency?
Nails. Nails protect the sensitive tips of fingers and toes. Like hair, nails are modified skin tissue hardened by the protein keratin. Although the nail itself is dead and lacks sensory receptors, it is embedded in tissue so sensitive that we detect even the slightest pressure of an object on the nail. In this way, nails serve as sensory "antennas." They also help us manipulate objects, as when we undo a tight knot in a shoelace.
Health Issue
Acne: The Miseries and Myths
Acne and adolescence go hand in hand. In fact, about four out of five teenagers have acne, a skin condition that will probably annoy, if not distress, them well into their twenties and possibly beyond.
Simple acne is a condition that affects hair follicles associated with oil glands. During the teenage years, oil glands increase in size and produce larger amounts of oily sebum. These changes are prompted by increasing levels of “male” hormones called androgens in the blood of both males and females; the androgens are secreted by the testes, ovaries, and adrenal glands. The changes thus induced in the activity and structure of oil glands set the stage for acne. It should come as no surprise, then, that acne occurs most often on areas of the body where oil glands are largest and most numerous: the face, chest, upper back, and shoulders.
Acne is the inflammation that results when sebum and dead cells clog the duct where the oil gland opens onto the hair follicle (Figure 4.B). A follicle obstructed by sebum and cells is called a whitehead. Sometimes the sebum in plugged follicles mixes with the skin pigment melanin, forming a blackhead. Thus, melanin, not dirt or bacteria, lends the dark color to these blemishes. The next stage of acne is pimple formation, beginning with the formation of a red, raised bump, often with a white dot of pus at the center. The bump occurs when obstructed follicles rupture and spew their contents into the surrounding epidermis. Such ruptures may occur naturally by the general buildup of sebum and cells or may be induced by squeezing the area. The sebum, dead cells, and bacteria that thrive on them then cause a small infection—a pimple or pustule—that will usually heal within a week or two without leaving a scar.
Eating nuts, chocolate, pizza, potato chips, or any of the other “staples” of the teenage diet does not cause acne. Also, acne is not caused by poor hygiene. Follicles plug from below, so dirt or oil on the skin surface is not responsible. (Most doctors do, however, recommend washing the face two or three times a day with hot water to help open plugged follicles.)
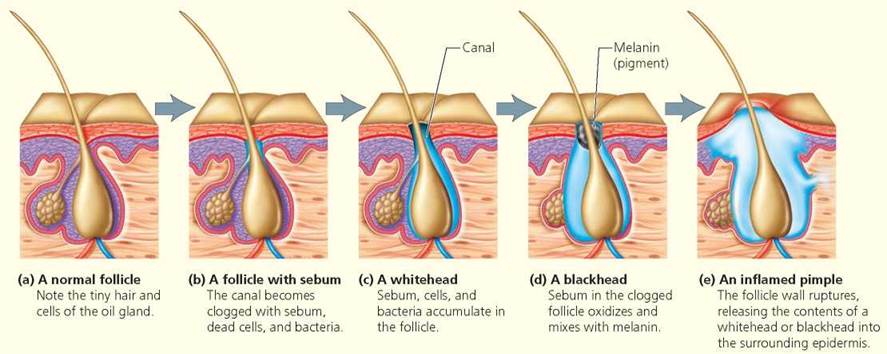
FIGURE 4.B. The stages of acne
Questions to Consider
• Why do you think that there are so many misconceptions about the causes of acne?
• If a new medication for acne were marketed, how would you decide whether to use it?
Glands. Three types of glands—oil, sweat, and wax—are found in the skin. Although all three types develop from epidermal cells, they differ in their locations, structures, and functions.
Oil (sebaceous) glands are found virtually all over the body except on the palms of the hands and soles of the feet. They secrete sebum, an oily substance made of fats, cholesterol, proteins, and salts. The secretory part of these glands is located in the dermis, as shown in Figure 4.8. Sebum lubricates hair and skin and contains substances that inhibit growth of certain bacteria. Sometimes, however, the duct of an oil gland becomes blocked, causing sebum to accumulate and disrupt the gland's proper function. Then, bacteria can invade the gland and hair follicle, resulting in a condition called acne. See the Health Issue essay, Acne: The Miseries and Myths.
As their name implies, sweat glands produce sweat, which is largely water plus some salts, lactic acid, vitamin C, and metabolic wastes such as urea. Although some wastes are eliminated through sweating, the principal function of sweat is to help regulate body temperature by evaporating from the skin surface. Wax glands are modified sweat glands found in the external ear canal. As their name implies, they produce wax, which protects the ear by trapping small particles.
Homeostasis
To remain healthy, the organ systems of the body must constantly adjust their functioning in response to changes in the internal and external environment. We have already learned that the body's organ systems are interdependent, working together to provide the basic needs of all cells—water, nutrients, oxygen, and a normal body temperature. Just as city dwellers breathe the same air and drink the same city water, the cells of the body are surrounded by the same extracellular fluid. Changes in the makeup of that fluid will affect every cell.
One advantage of our body's multicellular, multiorgan-system organization is its ability to provide a controlled environment for the cells. Although conditions outside the body sometimes vary dramatically, our organ systems interact to maintain relatively stable conditions within. This ability to maintain a relatively stable internal environment despite changes in the surroundings is called homeostasis (meaning "to stay the same"). But, conditions within the body never stay the same. As internal conditions at any level vary, the body's processes must shift to counteract the variation. Homeostatic mechanisms do not maintain absolute internal constancy, but they do dampen fluctuations around a set point to keep internal conditions within a certain range. Thus, homeostasis is not a static state but a dynamic one.
Illness can result if homeostasis fails. We see this in diabetes, a condition in which either the pancreas does not produce enough of the hormone insulin or the body cells are unable to use insulin. Normally, as a meal is digested and nutrients are absorbed into the bloodstream, the rising level of glucose in the blood stimulates the pancreas to release insulin. The general effect of insulin is to lower the blood level of glucose, returning it to a more desirable value. Without insulin, blood glucose can rise to a point that causes damage to the eyes, kidney, nerves, and blood vessels. A healthy diet, exercise, medication, and sometimes insulin injections can help people with diabetes regulate their blood glucose level.
Homeostasis depends on communication within the body. The nervous and endocrine systems are the two primary means of communication. The nervous system can bring about quick responses to changes in internal and external conditions. The endocrine system produces hormones, which bring about slower and longer-lasting responses to change.
Stop and think
When you exercise, your breathing rate, blood pressure, and heart rate increase. Is this a violation of homeostasis?
Negative Feedback Mechanisms
Homeostasis is maintained primarily through negative feedback mechanisms—corrective measures that slow or reverse a variation from the normal value of a factor, such as blood glucose level or body temperature, and return the factor to its normal value. When the normal value is reached, the corrective measures cease; the normal value is the feedback that turns off the response. (In contrast, a positive feedback mechanism causes a change that promotes continued change in the same direction. Positive feedback mechanisms, which are described in Chapter 10, do not promote homeostasis.)
Homeostatic mechanisms have three components (Figure 4.12).
1. A receptor detects change in the internal or external environment. A receptor, in this context, is a sensor that monitors the environment. When the receptor detects a change in some factor or event—some variable—it sends that information to the control center, the second of the three components.
2. A control center determines the factor's set point—the level or range that is normal for the factor in question. The control center integrates information coming from all the pertinent receptors and selects an appropriate response. In most of the body's homeostatic systems, the control center is located in the brain.
3. An effector, often a muscle or gland, carries out the selected response.
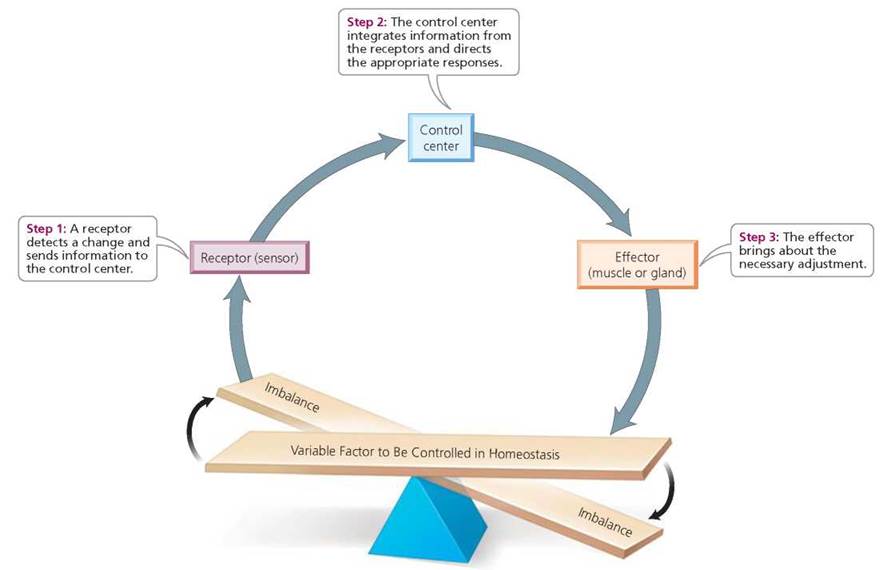
FIGURE 4.12. The components of a homeostatic control system maintained by negative feedback mechanisms
Stable blood calcium levels are important to many physiological processes. Calcitonin is a hormone from the thyroid gland that lowers blood calcium levels. Parathyroid hormone from the parathyroid glands is a hormone that raises blood calcium levels. Describe a negative feedback relationship involving these hormones as effectors that would maintain homeostasis by keeping blood calcium levels stable.
An elevation in blood calcium level would be sensed by receptors. In response, a control center in the brain would stimulate the thyroid gland to increase production of calcitonin, which lowers blood calcium level. If the calcium level dropped too low, receptors would signal the control center in the brain. In response, the control center would stimulate the parathyroid glands to increase production of parathyroid hormone, which would raise blood calcium levels.
Consider how a negative feedback mechanism controls the temperature in your home during the frigid winter months. A thermostat in the heating system serves as both the temperature-sensing receptor and the control center. If it senses that the temperature inside your home has fallen below a certain programmed set point, the thermostat turns on the heating system (the effector). When the thermostat senses that the internal temperature has returned to the set point, it turns the heating system off. Thus, the temperature fluctuates around the set point but remains within a certain range. Now, let's apply these principles to see how homeostatic mechanisms regulate body temperature.
Hypothalamus and Body Temperature
The body's temperature control center is located in a region of the brain called the hypothalamus. Its set point is approximately 37°C (98.6°F), although it differs slightly from one person to the next. Body temperature must not vary too far from this mark, because even small temperature changes have dramatic effects on metabolism. Temperature is sensed at the body's outer surface by skin receptors and deep inside the body by receptors that sense the temperature of the blood. The hypothalamus receives input from both types of receptor. If the input indicates that body temperature is below the set point, the brain initiates mechanisms to increase heat production and conserve heat. When the input indicates that body temperature is above the set point, the brain initiates mechanisms that promote heat loss.
Let's consider what happens when we find ourselves in an environment where the temperature is above our set point, say 38°C (100.4°F). Thermoreceptors in the skin detect heat and activate nerve cells that send a message to the hypothalamus, which then sends nerve impulses to the sweat glands to increase their secretions. As the secretions (perspiration) evaporate and body temperature drops below 37°C (98.6°F), the signals from the brain to the sweat glands are discontinued. In this homeostatic system, the thermoreceptors in the skin are the receptors, the hypothalamus is the control center, and the sweat glands are the effectors. The system is a negative feedback mechanism because it produces an effect (cooling of the skin) that is relayed (feeds back) to the control center, shutting off the corrective mechanism when the desired change has been produced.
Other mechanisms that the brain may activate to lower body temperature include dilation of blood vessels in the dermis and relaxation of the arrector pili muscles attached to the hair follicles. The former response releases more heat to the surrounding air and explains the flushed appearance we get during strenuous exercise. The latter keeps damp, cooling hair lying close to the skin. The brain may also initiate behavioral responses to a high body temperature, such as seeking shade or removing a sweatshirt.
Stop and think
As people age, the activity of their sweat glands declines. How does this explain why public authorities are less concerned about children than they are about the elderly developing a heat-related illness during a heat wave?
Now let's consider what happens when body temperature drops below the set point. Subtle drops in body temperature are detected largely by thermoreceptors in the skin, which send a message to the hypothalamus in the brain. The brain then sends nerve impulses to sweat glands, ordering a decrease in their activity, as well as messages to vessels in the dermis, telling them to constrict. This constriction reduces blood flow to the extremities, conserving heat for the internal organs and giving credence to the saying, "cold hands, warm heart." Another response to decreasing body temperature is contraction of arrector pili muscles, causing hairs to stand on end and thereby trapping an insulating layer of air near the body. This response, known as piloerection, is less effective in humans than in more heavily furred animals. The body also responds to cooling by increasing metabolic activity to generate heat and by the repeated contraction of skeletal muscles, known as shivering. Finally, behavioral responses, such as folding one's arms across one's chest, may be called upon to help combat a drop in body temperature. See Figure 4.13 for a summary of body temperature regulation.
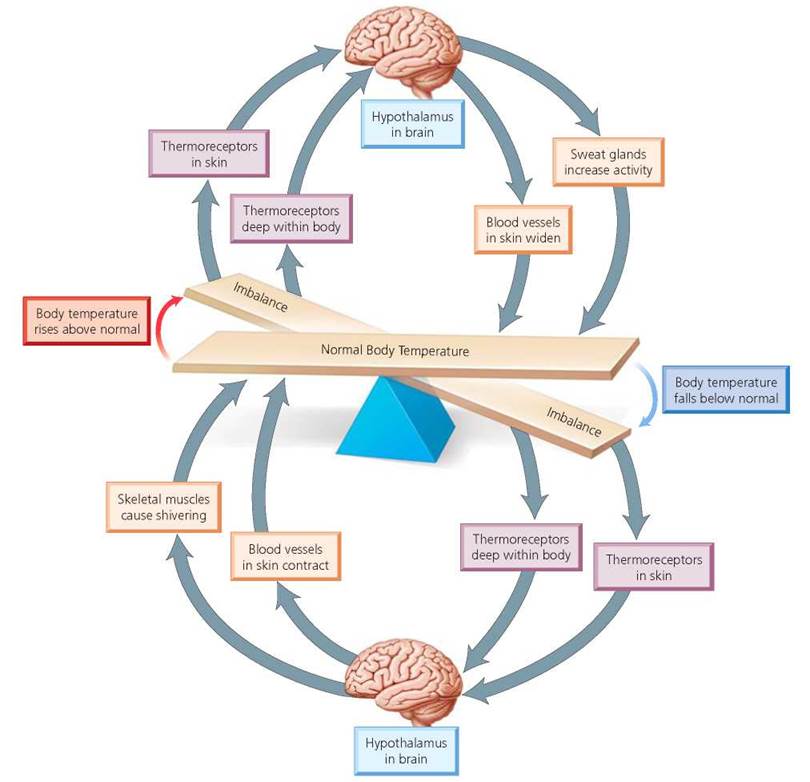
FIGURE 4.13. Homeostatic regulation of body temperature by negative feedback mechanisms. In this homeostatic control system, thermoreceptors are the sensors, the hypothalamus is the control center, and sweat glands, blood vessels in the skin, and skeletal muscles are the effectors.
Sometimes the mechanisms for lowering higher-than- normal temperatures fail, resulting in potentially deadly hyperthermia—abnormally elevated body temperature. Some marathon runners have died as a result of elevated core temperatures, as have people sitting in a hot tub heated to too high a temperature (say, up around 114°F). In both situations, perspiration could bring no relief; its evaporation would be prevented by high humidity in the case of the runners or by the surrounding water in the case of the hot-tubbers. Commonly called heat stroke, hyperthermia is marked by confusion and dizziness. If the core temperature reaches about 42°C (107°F), the heartbeat becomes irregular, oxygen levels in the blood drop, the liver ceases to function, and unconsciousness and death soon follow. Few people can survive core temperatures of 43°C (110°F).
If the body's temperature drops too far—to 35°C (95°F) or below—a condition called hypothermia results, disrupting nervous system function and temperature-regulating mechanisms. People suffering from hypothermia usually become giddy and confused at first. When their temperature drops to 33°C (91.4°F), they lose consciousness. Finally, at a body temperature of 30°C (86°F), blood vessels are completely constricted and temperature-regulating mechanisms are fully shut down. Death soon follows. Hypothermia can be treated if detected early enough. In severe cases, dialysis machines may be used to artificially warm the blood and pump it back into the body.
Stop and think
Frostbite is damage to tissues exposed to cold temperatures. Given what you know about the body's response to cold temperature, why are fingers and toes particularly susceptible to frostbite?
Looking ahead
In this chapter we saw how cells form tissues, tissues form organs, and organs form organ systems. Beginning with the next chapter, “The Skeletal System,” we will explore each organ system.
Highlighting the Concepts
From Cells to Organ Systems (pp. 68-76)
• Tissues are groups of cells that work together to perform a common function. There are four main types of tissue in the human body: epithelial (covers body surfaces, forms glands, and lines internal cavities and organs), connective (acts as storage site for fat, plays a role in immunity and in transport, and provides protection and support), muscle (generates movement), and nervous tissue (coordinates body activities through initiation and transmission of nerve impulses).
• All connective tissues contain cells in an extracellular matrix composed of protein fibers and ground substance. The types of connective tissue are connective tissue proper (loose and dense connective tissue) and specialized connective tissue (cartilage, bone, and blood).
• Blood consists of formed elements (red blood cells, white blood cells, and platelets) suspended in a liquid matrix (plasma). The protein fibers are normally dissolved in the plasma and play a role in blood clotting. Red blood cells transport oxygen and carbon dioxide; white blood cells aid in fighting infections; and platelets function in blood clotting.
• Muscle tissue is composed of muscle fibers that contract when stimulated, generating a mechanical force. There are three types of muscle tissue: skeletal, cardiac, and smooth. Skeletal muscle tissue is usually attached to bone, is voluntary, has cross-striations visible under a microscope, and has several nuclei in each cell. Cardiac muscle tissue is found in the walls of the heart, is involuntary, has cross-striations, and usually contains only one nucleus in each cell. Smooth muscle tissue is in the walls of blood vessels, airways, and organs. It is involuntary and lacks striations. A smooth muscle cell tapers at each end and has a single nucleus.
• Nervous tissue consists of cells called neurons and accessory cells called neuroglia. Neurons convert stimuli into nerve impulses that they conduct to glands, muscles, or other neurons. Neuroglia increase the rate at which impulses are conducted by neurons and provide neurons with nutrients from nearby blood vessels. Neuroglial cells can communicate with one another and with neurons.
• Three types of specialized junctions hold tissues together. Tight junctions prevent the passage of materials through the boundaries where cells meet. Adhesion junctions link cells by intercellular filaments attached to thickenings in the plasma membrane. Gap junctions have small pores that allow physical and chemical communication between cells.
• An organ is a structure that is composed of two or more different tissues and has a specialized function.
• Two or more organs that participate in a common function are collectively called an organ system. The human body has 11 major organ systems.
• Internal organs are located in body cavities. There are two main body cavities: (1) the dorsal cavity, which is subdivided into the cranial cavity, where the brain is located, and the spinal cavity, where the spinal cord is located; and (2) the ventral cavity, which is subdivided into the thoracic (chest) cavity and the abdominal cavity. The thoracic cavity is further divided into the pleural cavities, which contain the lungs, and the pericardial cavity, which contains the heart. Membranes line body cavities and spaces within organs.
Skin: An Organ System (pp. 76-82)
• The integumentary system includes the skin and its derivatives, such as hair, nails, and sweat and oil glands. It protects underlying tissues from abrasion and dehydration; regulates body temperature; synthesizes vitamin D; detects stimuli associated with touch, temperature, and pain; and initiates body defense mechanisms.
• The skin has two layers. The outermost layer, or epidermis, is composed of epithelial cells that die and wear away. The dermis, just below, is a much thicker, nondividing layer composed of connective tissue and containing nerves, blood vessels, and glands. Below the dermis is the hypodermis, a layer of loose connective tissue that anchors the skin to underlying tissues.
• The epidermis is a renewing barrier. Cells produced in the deepest layer are pushed toward the skin surface, flattening and dying as they move away from the blood supply of the dermis and replace their cytoplasmic contents with keratin.
• Skin color is partially determined by melanin, a pigment released by melanocytes at the base of the epidermis and taken up by neighboring cells on their way to the surface. Blood flow and blood oxygen content also influence skin color.
• Hair is a derivative of skin. The primary function of hair is protection.
• Nails are modified skin tissue hardened by keratin. They protect the tips of our fingers and toes and help us grasp and manipulate small objects.
• Oil and sweat glands are derivatives of skin. Sebum, the oily substance secreted by oil glands, lubricates the skin and hair, prevents desiccation, and inhibits the growth of certain bacteria.
Homeostasis (pp. 82-86)
• Homeostasis is the relative internal constancy maintained at all levels of body organization. It is a dynamic state, with small fluctuations occurring around a set point, and is sustained primarily through negative feedback mechanisms.
• Homeostatic mechanisms consist of receptors, a control center, and effectors.
Reviewing the Concepts
1. What are the four types of tissue found in the human body? p. 68
2. Contrast the organization of epithelial and connective tissues. How are differences in the matrix of different types of connective tissue related to their functions? pp. 69-73
3. Why does bone heal more rapidly than cartilage? p. 71
4. What type of tissue is blood? p. 71
5. Contrast skeletal, cardiac, and smooth muscle with respect to structure and function. pp. 73-74
6. What types of cells are found in nervous tissue? What are their functions? p. 74
7. List the functions of the integumentary system. pp. 76-82
8. Describe the roles of pigments and blood flow in determining skin color. p. 80
9. What causes goose bumps? pp. 80-81
10. What are oil glands? p. 82
11. Describe the functions of the sweat glands. p. 82
12. What is homeostasis? pp. 82-83
13. Describe the body's homeostatic mechanisms for raising and lowering core body temperature. pp. 83-85
14. The four basic tissue types in the body are
a. simple, cuboidal, squamous, columnar.
b. neural, epithelial, muscle, connective.
c. blood, nerves, bone, cartilage.
d. fat, cartilage, muscle, neural.
15. The lining of the intestine is composed primarily of
a. epithelial cells.
b. muscle cells.
c. connective tissue cells.
d. nerve cells.
16. Cells that form disks that cushion the vertebrae are
a. bone.
b. muscle.
c. epithelium.
d. cartilage.
17. The mineral that makes bone hard is _____.
18. The maintenance of body processes within a relatively constant range is called _____.
Applying the Concepts
1. Thor, a ski champion at his college, tore the cartilage in his knee in a ski accident. He asked the doctor if he would be ready to compete in a month. Why would you expect the doctor's answer to be "No"?
2. Hannah has the flu. As her fever rises, she gets the chills. She shivers and covers herself in extra blankets. She takes some acetaminophen and her fever breaks. As her body temperature returns to normal, she throws off the blankets, looks flushed, and perspires. Use the mechanisms of body temperature control to explain what is happening as Hannah's fever rises and falls.
3. Ehlers-Danlos syndrome (EDS) is a group of disorders caused by defects in genes that disrupt the production of collagen, which is a chief component of connective tissue. Explain why symptoms of EDS include joints that extend beyond their normal range and stretchy, saggy skin.
Becoming Information Literate
Prepare a brochure or other presentation explaining ways to avoid skin cancer. Use at least three reliable sources (books, journals, websites). List each source you considered, and explain why you chose the three sources you used.